Coil Contraception: Everything You Need to Know

The coil is a type of contraception that can be fitted into your uterus. The contraceptive coil works by preventing sperm from reaching an egg, and it's one of the most effective forms of contraception out there. It's a good option for women who want something long-term but don't want to deal with taking the pill every day or having an implant put under their skin—and it can last for up to five years!
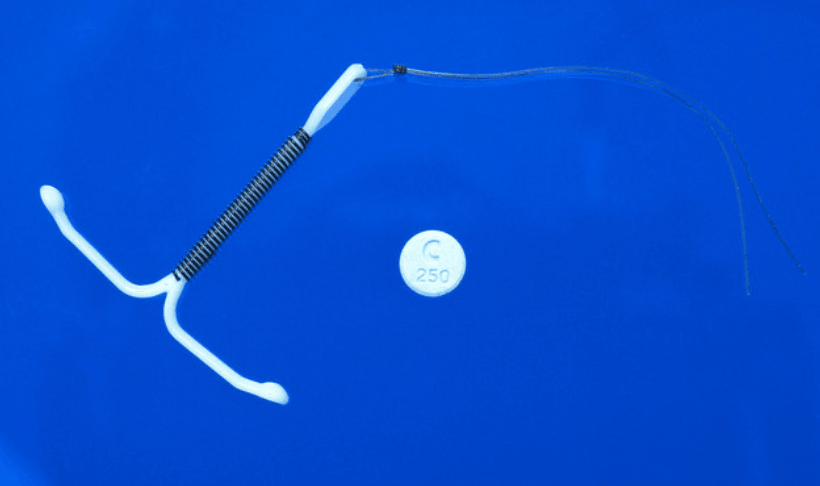
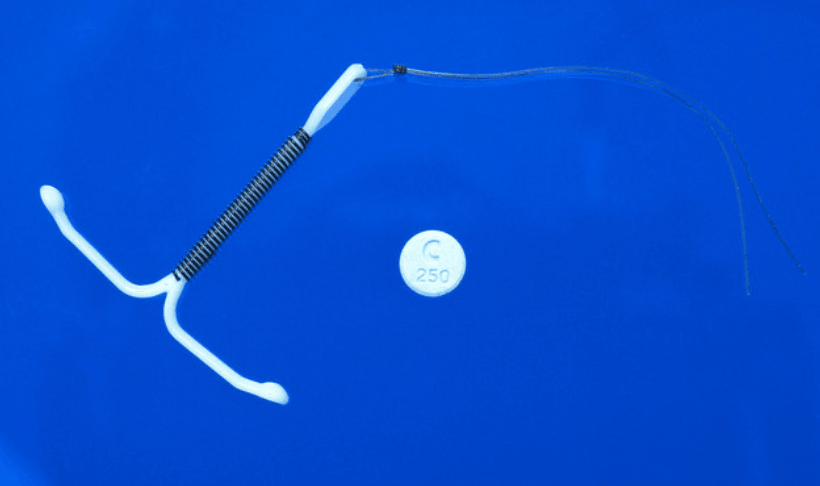
Copper coils are small T-shaped metal coils coated in copper. It's inserted into the female womb causing small copper ions to be released into the womb. Copper ions are similar to spermicides because they kill sperm. A further possibility is that the coil may prevent the implantation of fertilised sperm into the womb. It consists of threads that can be attached to check whether it remains in place correctly. Usually, this coil needs an experienced health professional who checks if it stays in place and changes its position if necessary until you get used to using it yourself before removing it at any time (usually after five years).
Intrauterine devices or copper cables (IUDs) are tiny plastic- and copper - devices inserted into the uterus that is placed in the body. Usually, copper coils are made of polyethylene plastic and barium sulphate with copper wire wrapped around vertical legs. Contraceptives are not hormone controlled. In a copper IUD, pregnancy is not possible because its effectiveness is 99%.
The coil is placed in the womb by a trained doctor or nurse during your period when it is most flexible and able to be inserted comfortably without pain or discomfort. The device has two strings attached to it that hang down from your cervix so you can remove it easily if necessary.
IUDs are similar to the intrauterine system or IUS (hormonal coil). Instead of introducing a progestogen like the IUS, the IUD releases copper into pregnancy. Copper alters the cervical mucus on the cervical surface, making sperm difficult to access an egg. The toxins in the blood prevent fertilised eggs from being implanted. IUDs are available until menopause, or you stop using contraceptives until your 40s or 60s.
Coil prevents fertilisation by:
Blocking ovulation: The coil is inserted into your uterus before you ovulate so it can prevent sperm from coming into contact with your egg
Blocking fallopian tubes: If there is no egg released, then there will be no way for fertilisation to take place
Preventing implantation of embryos: As mentioned above, if there is no embryo, then there cannot be a pregnancy
You can book an appointment with your doctor or nurse to have a coil inserted. Your doctor will also advise you on how to take care of yourself after the insertion.
Next, you must make sure that:
You are not pregnant
You do not have sexually transmitted infections (STIs) such as chlamydia or gonorrhoea (this is because these infections can cause complications if you become pregnant while using this method). If this is the case, a doctor will give you antibiotics to prevent an infection.
The IUD is a practical, non-hormonal method of contraception. It can be left in place for up to 10 years, with the potential for pregnancy occurring after 3 to 6 months. The device can be fitted once and then forgotten until it's time to remove it. In addition, you don't have to worry about remembering a daily pill or putting on a condom before sex.
It could be worth considering if you want to use the IUD while breastfeeding or has given birth within six weeks. Some women cannot take oestrogen; if this is the case for you and you'd like an alternative option to prevent pregnancy, the IUD may be right for you too!
The coil does not protect against STIs. It only protects against pregnancy, so if you want protection against STIs, use a condom.
You should also be aware that the coil is NOT effective at preventing the spread of some STIs such as Herpes and HPV (the virus that causes warts).
If you're in the UK, getting the IUD fitted as soon as six weeks after giving birth is possible. But if you don't need contraception immediately, there's no need to rush into having this procedure done. You can have your IUD fitted whenever—even years after childbirth—and still be protected against pregnancy.
If you get fitted with a copper IUD within six weeks of giving birth and are breastfeeding your baby, watch out for side effects like heavy bleeding and cramping. These could be signs that your body is rejecting the device, meaning you should remove it immediately. If not, speak with your doctor about what to do next.
Side effects are rare but can include:
Menstrual irregularities
Headaches
Back pain
Vaginal discharge
Irregular bleeding (including spotting) after IUD insertion
PID-pelvic inflammatory disease (PID) is a bacterial infection of the female reproductive organs. Chlamydia, gonorrhoea, or other bacteria in your vagina or cervix caused it. This infection may lead to infertility if not treated. Signs and symptoms include painful periods with heavy bleeding, abdominal pain and tenderness, fever, nausea and vomiting. PID is not a common side effect of using the copper IUD for contraception. If you think you have an STD such as chlamydia or gonorrhoea that can cause PID even though you're not having sex with a new partner or multiple partners at once, see your doctor immediately. They will diagnose your condition based on symptoms like these and tests from their office visit. If necessary, they may prescribe antibiotics to treat these STDs.

If you think the IUD has come out, the first thing to do is to check. If you are bleeding and there's no sign of it, it hasn't come out. However, some women experience spotting when their IUDs are still in place.
However, if your IUD copper coil fails to perform as contraception, an ectopic pregnancy might occur. An ectopic pregnancy happens when a fertilised egg gets stuck in one of the fallopian tubes outside the womb.
If you think your IUD has come out, it is essential to check your menstrual cycle. Look for signs of bleeding or spotting if you have had sex recently and are concerned that the IUD may have become dislodged. If these changes continue for longer than seven days, contact your GP or practice nurse immediately.
Suppose you have had sex and experienced vaginal bleeding. This may indicate that the device has been expelled from the uterus into the vagina. This type of bleeding is called 'extravaginal' because it occurs outside of the uterus in an area where pregnancy cannot develop (this is not possible with an IUD).
You can also take a pregnancy test if there are any concerns about whether you are pregnant or not. The test can tell whether you are pregnant within minutes of taking it.
An IUD is an effective way to prevent pregnancy, and it can help reduce heavy bleeding and painful periods.
The hormone progestogen causes most of the side effects experienced while using a hormonal contraceptive like the IUD or pill. The progestogen is released into your body when you take certain birth control pills or use other forms of contraception like an implant or intrauterine device (IUD). This hormone causes some women to have altered moods—such as feeling more emotional—during their time on birth control. Progestogen also makes some people bleed more heavily than usual during their period and can even cause cramping in some individuals, especially when taken at higher doses over more extended periods.
So why does this matter? Because all contraceptive methods contain some form of synthetic progestogen—including all IUDs! Suppose you are not used to having high levels of hormonal contraceptives present in your system over long periods. In that case, it may react badly by causing pain during menstruation (or "periods").
The answer to this question is not straightforward. The answer will depend on why you are considering having an IUD removed, whether or not there are other forms of contraception, and what these are. If you have only had one IUD fitted and want to stop using it because your partner has started taking an alternative form of contraception, then yes, it is possible to remove the original device (but talk first with a doctor or nurse). However, if you are using another method of contraception alongside your IUD, then this should not be stopped unless advised by a medical professional. Suppose no other form of contraception is being used alongside your IUD. In that case, there may be little point in removing an implantable contraceptive. So removal may not be appropriate at all times.
The IUD can be fitted up to five days after your last period. You will need to use additional contraception (e.g. condoms) for seven days after the IUD is fitted.
After inserting your IUD, you must check it six months or earlier if you have any concerns. If you are happy with how it's working, you should repeat this every three years.
Suppose you want to get pregnant in the future. In that case, you will need to have your IUD removed before this happens, so take care when making decisions about family planning.
The IUD is a contraceptive device inserted into your womb by trained doctors or nurses. They're available in different forms and sizes, depending on where you live and what type of contraception you choose.
They are effective at preventing pregnancy and can be removed at any time as long as they've been left inside for seven days or more (this gives sperm enough time to die). Contraceptive implantation has been proven to be an effective and reliable means of birth control. Still, some risks are involved with using this method, such as perforation of the baby during pregnancy, infection etc. So, make sure you talk about these things beforehand with your doctor if you decide that this method would work best for you!
In most cases, when your IUD is inserted, it should cause no pain or discomfort whatsoever. However, if anything feels unusual, please ask someone who knows what's going on before proceeding further down those lines. In rare cases where this happens, health professionals recommend talking directly with your doctor about how best to manage things like pain management techniques which might help reduce discomfort levels significantly over time!
An IUD is a safe and effective form of contraception used by women to prevent pregnancy. It is particularly recommended for those who do not want to use hormones or have surgery as it does not interfere with natural processes in the body.
If you're looking for a new way to prevent pregnancy, many options are available.
One option is the copper coil, which releases copper ions into your body to prevent the sperm from reaching the egg. The copper ions react with the cervical mucus, making it harder for sperm to swim through it, making it harder for them to fertilise an egg. This method can be used as a form of emergency contraception as well.
Another option is visiting your GP or nurse and discussing your medical history with them. They can then provide you with information about other methods of contraception, such as the pill or implant, that may work better for you than others.
You can also visit one of your local contraception clinics, where they will give you more information on different types of contraception. They would even help you find one that best suits your lifestyle needs and preferences.
If you want to learn more about the various types of contraception, click here.










Plus get the inside scoop on our latest content and updates in our monthly newsletter.