Health hub
Learn everything you need to know about a healthy and balanced life in one place. From your cholesterol levels and liver function to women's health, we cover a range of topics to help improve your health knowledge.
Mens Health
View all-

11 Best Men’s Hair Products of 2025
Selection of the best products for Men's Hair requires navigation of a lot of hair sprays, waxes, gels, and pomades, and all these products claim to be the best ones....
11 Best Men’s Hair Products of 2025
Selection of the best products for Men's Hair requires navigation of a lot of hair sprays, waxes, gels, and pomades, and all these products claim to be the best ones....
-

10 Best Natural Testosterone Supplements
Testosterone, a hormone mostly produced in the testicles for men and the ovaries and adrenal glands for women, has a significant impact on our health. It is responsible for maintaining...
10 Best Natural Testosterone Supplements
Testosterone, a hormone mostly produced in the testicles for men and the ovaries and adrenal glands for women, has a significant impact on our health. It is responsible for maintaining...
-

What is the Life Expectancy After Prostate Remo...
What is Prostate Removal? Prostate removal, also known as prostatectomy, is a surgical procedure used to treat prostate cancer. Removing the prostate for health concerns is a significant decision. It...
What is the Life Expectancy After Prostate Remo...
What is Prostate Removal? Prostate removal, also known as prostatectomy, is a surgical procedure used to treat prostate cancer. Removing the prostate for health concerns is a significant decision. It...
Women's Health
View all-

Best Panty Liners for Comfort in 2025, Tried an...
Dr Muhammad Zeeshan AfzalThe right pantyliner makes a big difference in hygiene and everyday comfort. Women who are concerned about their comfort during light flow days choose them. In 2025, many market options...
Best Panty Liners for Comfort in 2025, Tried an...
Dr Muhammad Zeeshan AfzalThe right pantyliner makes a big difference in hygiene and everyday comfort. Women who are concerned about their comfort during light flow days choose them. In 2025, many market options...
-

11 Best Shaving Creams for Women
Dr Muhammad Zeeshan AfzalShaving is vital to many women's grooming routines, and the choice of the right shaving creams makes a huge difference. A good shaving cream not only ensures a closer shave...
11 Best Shaving Creams for Women
Dr Muhammad Zeeshan AfzalShaving is vital to many women's grooming routines, and the choice of the right shaving creams makes a huge difference. A good shaving cream not only ensures a closer shave...
-

7 Top Women’s Hair Waxes to Help Tame Your Locks
Dr Muhammad Zeeshan AfzalThe perfect choice of hair waxes is a game changer for women looking for an ideal definition, control, and effortless style to tame their sculpted intricate and frizz styles or...
7 Top Women’s Hair Waxes to Help Tame Your Locks
Dr Muhammad Zeeshan AfzalThe perfect choice of hair waxes is a game changer for women looking for an ideal definition, control, and effortless style to tame their sculpted intricate and frizz styles or...
Pet Health
View all-

Best Diarrhea Medicine for Dogs of 2025
Dog Diarrhoea Relief: Why is it Important? Diarrhoea in dogs isn’t a particular disease but a symptom of a lot of possible health problems. In dogs with diarrhoea, the food...
Best Diarrhea Medicine for Dogs of 2025
Dog Diarrhoea Relief: Why is it Important? Diarrhoea in dogs isn’t a particular disease but a symptom of a lot of possible health problems. In dogs with diarrhoea, the food...
-

10 Best Dog Multivitamins for Your Furry Friend
Pet supplements are a vital part of taking proper care of your pet since they will help to complement a balanced diet. Dogs also require certain nutrients for them to...
10 Best Dog Multivitamins for Your Furry Friend
Pet supplements are a vital part of taking proper care of your pet since they will help to complement a balanced diet. Dogs also require certain nutrients for them to...
-
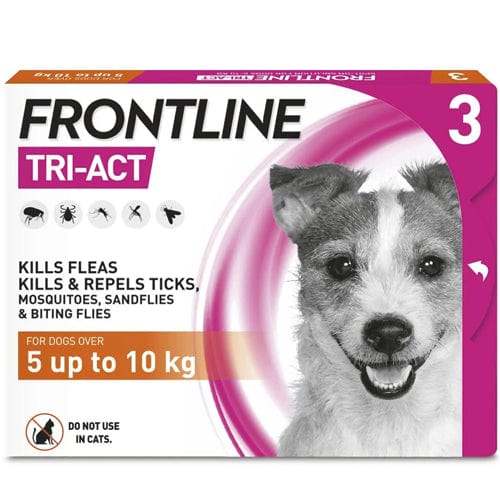
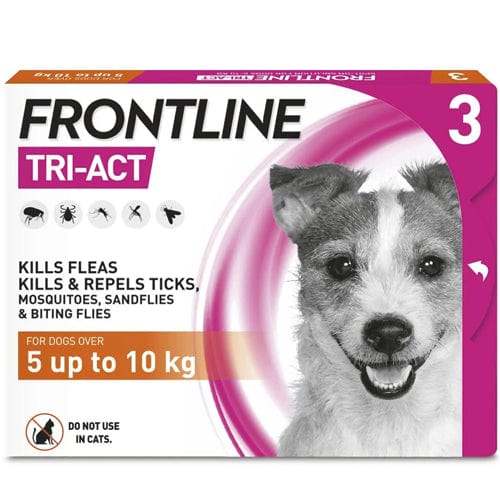
5 Best Dog Flea Treatments for Your Pup
Dealing with a flea infestation is one of the most common problems that dog owners encounter. These microscopic parasites are not only uncomfortable, but they also seriously endanger the dog's...
5 Best Dog Flea Treatments for Your Pup
Dealing with a flea infestation is one of the most common problems that dog owners encounter. These microscopic parasites are not only uncomfortable, but they also seriously endanger the dog's...
Bone & Joint Health
View all-

Crepitus & Clicking Joints: Symptoms, Treatment...
Crepitus, or joint popping, is the term for audible noises produced by a moving joint, such as popping, cracking, and grinding. When these "pops" occur, pressure seems to be released...
Crepitus & Clicking Joints: Symptoms, Treatment...
Crepitus, or joint popping, is the term for audible noises produced by a moving joint, such as popping, cracking, and grinding. When these "pops" occur, pressure seems to be released...
-

Broken Knuckle: Diagnosis, Symptoms and Treatment
The broken knuckle is largely sustained through direct trauma or by applying excessive force on the hand. Proper and accurate medical attention is urgently called for the complete functional restoration...
Broken Knuckle: Diagnosis, Symptoms and Treatment
The broken knuckle is largely sustained through direct trauma or by applying excessive force on the hand. Proper and accurate medical attention is urgently called for the complete functional restoration...
-

7 Best Lumbar Support Pillows of 2025
The lumbar spine often becomes achy while in a single position, e.g., standing and sitting for a considerable time. The lumbar pillows deliver support to the lumbar spine where it...
7 Best Lumbar Support Pillows of 2025
The lumbar spine often becomes achy while in a single position, e.g., standing and sitting for a considerable time. The lumbar pillows deliver support to the lumbar spine where it...
Sports Performance
View all-

Top 8 Pre-Workout Supplements to Fuel Your Work...
The idea of pre-workout supplements as a means of improving the workout experience is alluring to athletes and those who exercise for fitness. Pre-workouts come in various forms and are...
Top 8 Pre-Workout Supplements to Fuel Your Work...
The idea of pre-workout supplements as a means of improving the workout experience is alluring to athletes and those who exercise for fitness. Pre-workouts come in various forms and are...
-

11 Best Supplements for Muscle Growth
Building muscle is not just about training in the gym, it's about fuelling your body with the right nutrients to maximise your gains. Have you ever wondered why some athletes...
11 Best Supplements for Muscle Growth
Building muscle is not just about training in the gym, it's about fuelling your body with the right nutrients to maximise your gains. Have you ever wondered why some athletes...
-

Hack Squat: How to Do Them Properly for Stronge...
Hack squats are among the most famous leg-strengthening exercises, and there are many reasons for this claim. They help improve the stability and strength of glutes and quads and involve...
Hack Squat: How to Do Them Properly for Stronge...
Hack squats are among the most famous leg-strengthening exercises, and there are many reasons for this claim. They help improve the stability and strength of glutes and quads and involve...
Vitamin & Nutrition Blog
View all-

15 Best Carnitine Supplements for Overall Health
Carnitine supplements are very popular among people who want to optimise their physical performance and enhance overall health. It is a natural amino acid derivative that plays an important role...
15 Best Carnitine Supplements for Overall Health
Carnitine supplements are very popular among people who want to optimise their physical performance and enhance overall health. It is a natural amino acid derivative that plays an important role...
-

11 Best Lion’s Mane Supplements to Improve Over...
Lion's Mane, or Hericium erinaceus, is a medicinal mushroom well known for its beneficial impact on overall wellbeing, immunity, and brain health. It is one of the most adaptogenic supplements,...
11 Best Lion’s Mane Supplements to Improve Over...
Lion's Mane, or Hericium erinaceus, is a medicinal mushroom well known for its beneficial impact on overall wellbeing, immunity, and brain health. It is one of the most adaptogenic supplements,...
-

Top Astaxanthin Supplements of 2025
Astaxanthin is a highly potent antioxidant sourced from microalgae. It has gained a lot of popularity in the last decade due to its immense health benefits. It is a vibrant...
Top Astaxanthin Supplements of 2025
Astaxanthin is a highly potent antioxidant sourced from microalgae. It has gained a lot of popularity in the last decade due to its immense health benefits. It is a vibrant...
Blood Tests
View all-

Introducing BloodTestsOnline.co.uk – The UK's N...
Dr Adam WilliamsWe are proud to announce the launch of BloodTestsOnline.co.uk, the UK’s first fully dedicated home blood testing platform. Built to address the growing demand for fast, accurate, and convenient diagnostic...
Introducing BloodTestsOnline.co.uk – The UK's N...
Dr Adam WilliamsWe are proud to announce the launch of BloodTestsOnline.co.uk, the UK’s first fully dedicated home blood testing platform. Built to address the growing demand for fast, accurate, and convenient diagnostic...
-

What Level of Eosinophils Indicate Cancer?
Dr Sadia SaeedEosinophils are a type of white blood cell that make up a tiny portion of the white blood cells in the bloodstream. Like other white blood cells, it also plays...
What Level of Eosinophils Indicate Cancer?
Dr Sadia SaeedEosinophils are a type of white blood cell that make up a tiny portion of the white blood cells in the bloodstream. Like other white blood cells, it also plays...
-

MCHC Blood Test Results: Meaning of Low and Hig...
Dr Muhammad Zeeshan AfzalThe mean corpuscular haemoglobin concentration (MCHC) test measures the haemoglobin concentration in a specific volume of the packed red blood cells (RBCs). Haemoglobin is an iron-containing carrier protein that transports...
MCHC Blood Test Results: Meaning of Low and Hig...
Dr Muhammad Zeeshan AfzalThe mean corpuscular haemoglobin concentration (MCHC) test measures the haemoglobin concentration in a specific volume of the packed red blood cells (RBCs). Haemoglobin is an iron-containing carrier protein that transports...
Antibiotics
View all-

Trimethoprim vs. Other Antibiotics: A Comparati...
Antibiotics are potent drugs employed in modern medicine that kill or inhibit the growth of microorganisms, specifically bacteria, and certain parasites, to prevent and treat infections in humans and animals...
Trimethoprim vs. Other Antibiotics: A Comparati...
Antibiotics are potent drugs employed in modern medicine that kill or inhibit the growth of microorganisms, specifically bacteria, and certain parasites, to prevent and treat infections in humans and animals...
-

The Future of Antibiotics: Innovations and Chal...
The Future of Antibiotics: Innovations and Challenges Antibiotics, often hailed as one of the greatest medical discoveries of the 20th century, have revolutionized the field of medicine and saved countless...
The Future of Antibiotics: Innovations and Chal...
The Future of Antibiotics: Innovations and Challenges Antibiotics, often hailed as one of the greatest medical discoveries of the 20th century, have revolutionized the field of medicine and saved countless...
-

Antibiotics for Dental Issues: A Closer Look at...
Antibiotics for Dental Issues: A Closer Look at Oral Health Antibiotics have played a pivotal role in modern medicine, revolutionizing the treatment of bacterial infections and saving countless lives. While...
Antibiotics for Dental Issues: A Closer Look at...
Antibiotics for Dental Issues: A Closer Look at Oral Health Antibiotics have played a pivotal role in modern medicine, revolutionizing the treatment of bacterial infections and saving countless lives. While...
Beauty & Cosmetics
View all-

Best Women’s Perfumes in 2025, According to Fra...
Perfume is not just a fragrance but a way of expressing yourself and finishing with a touch that makes the lasting impression. In 2025, the world of women's fragrances is...
Best Women’s Perfumes in 2025, According to Fra...
Perfume is not just a fragrance but a way of expressing yourself and finishing with a touch that makes the lasting impression. In 2025, the world of women's fragrances is...
-

Top 10 Men’s Perfumes of 2025, Recommended by E...
Choosing an excellent perfume is not just about choosing a scent but about leaving a lasting impression throughout the day. Men's perfumes are different from home perfumes and women's perfumes...
Top 10 Men’s Perfumes of 2025, Recommended by E...
Choosing an excellent perfume is not just about choosing a scent but about leaving a lasting impression throughout the day. Men's perfumes are different from home perfumes and women's perfumes...
-

Top 10 Men’s Hair Pomades of 2025
Top 10 Men's Hair Pomades of 2025 The selection of an ideal pomade makes a big difference in hairstyle, whether looking for a more textured or voluminous finish or a...
Top 10 Men’s Hair Pomades of 2025
Top 10 Men's Hair Pomades of 2025 The selection of an ideal pomade makes a big difference in hairstyle, whether looking for a more textured or voluminous finish or a...
Baby & Child
View all-

10 Best Nasal Aspirators of 2025
Choosing the right nasal aspirator for both babies and adults can make a huge difference - especially during cold and allergy seasons. Nasal congestion impacts sleep, feeding, and overall comfort,...
10 Best Nasal Aspirators of 2025
Choosing the right nasal aspirator for both babies and adults can make a huge difference - especially during cold and allergy seasons. Nasal congestion impacts sleep, feeding, and overall comfort,...
-

Baby Acne and Breast Milk: Causes and Treatment
Many new parents are surprised to discover small red or white bumps on their baby’s face, backs, cheeks, and chin, often appearing weeks or months after birth. This common condition, known...
Baby Acne and Breast Milk: Causes and Treatment
Many new parents are surprised to discover small red or white bumps on their baby’s face, backs, cheeks, and chin, often appearing weeks or months after birth. This common condition, known...
-

Do Babies Have Kneecaps?
When it comes to babies and their fascinating growth journey, one common question parents often ask is, “Do babies have kneecaps?” The answer is both simple and complex - yes,...
Do Babies Have Kneecaps?
When it comes to babies and their fascinating growth journey, one common question parents often ask is, “Do babies have kneecaps?” The answer is both simple and complex - yes,...
Cold & Flu
View all-

11 Best Cough Sweets to Relieve Sore Throat
What is a Sore Throat? Painful, scratchy, or irritated sensation in all or part of the throat, especially with difficulty swallowing. A sore throat can range from just a minor...
11 Best Cough Sweets to Relieve Sore Throat
What is a Sore Throat? Painful, scratchy, or irritated sensation in all or part of the throat, especially with difficulty swallowing. A sore throat can range from just a minor...
-

12 Best Teas for Sore Throat to Help You Get Th...
Cold and flu season is here again, bringing along stuffy noses and sore throats. It can feel like a never-ending cycle of discomfort, but thankfully, tea can help you feel...
12 Best Teas for Sore Throat to Help You Get Th...
Cold and flu season is here again, bringing along stuffy noses and sore throats. It can feel like a never-ending cycle of discomfort, but thankfully, tea can help you feel...
-

Why does putting vicks on your feet stop Coughing?
Vicks VapoRub, a ubiquitous name in households worldwide, stands as a testament to the enduring legacy of over-the-counter remedies. Its formulation, a blend of camphor, eucalyptus oil, and menthol, has...
Why does putting vicks on your feet stop Coughing?
Vicks VapoRub, a ubiquitous name in households worldwide, stands as a testament to the enduring legacy of over-the-counter remedies. Its formulation, a blend of camphor, eucalyptus oil, and menthol, has...
Erectile Dysfunction
View all-

Erectile Dysfunction: Symptoms, Causes, Diagnos...
A Comprehensive Guide to Erectile Dysfunction: Symptoms, Causes, Diagnosis and Treatment Erectile Dysfunction (ED), also known as impotence, is a common male health issue in which a male is either...
Erectile Dysfunction: Symptoms, Causes, Diagnos...
A Comprehensive Guide to Erectile Dysfunction: Symptoms, Causes, Diagnosis and Treatment Erectile Dysfunction (ED), also known as impotence, is a common male health issue in which a male is either...
-

Simple Trick to Cure ED: 7 Simple Steps
7 Simple Tricks to Cure Erectile Dysfunction Explanation of Erectile Dysfunction (ED) Erectile dysfunction (ED) is a prevalent health issue affecting millions of men worldwide. It is a condition characterised...
Simple Trick to Cure ED: 7 Simple Steps
7 Simple Tricks to Cure Erectile Dysfunction Explanation of Erectile Dysfunction (ED) Erectile dysfunction (ED) is a prevalent health issue affecting millions of men worldwide. It is a condition characterised...
-

Can a Blood Test Check for Erectile Dysfunction?
Also known as impotence, erectile dysfunction (ED) is a common condition affecting millions of men worldwide. It refers to the inability to maintain or achieve an erection sufficient for sexual...
Can a Blood Test Check for Erectile Dysfunction?
Also known as impotence, erectile dysfunction (ED) is a common condition affecting millions of men worldwide. It refers to the inability to maintain or achieve an erection sufficient for sexual...
Hair Loss
View all-

7 Best HRT for Hair Loss: Reviewed by Experts
Dr Muhammad Zeeshan AfzalHair loss is a common issue regardless of gender and is mostly linked to hormonal imbalances and fluctuations. Other factors, such as environmental factors, genes, and lifestyle, have some role,...
7 Best HRT for Hair Loss: Reviewed by Experts
Dr Muhammad Zeeshan AfzalHair loss is a common issue regardless of gender and is mostly linked to hormonal imbalances and fluctuations. Other factors, such as environmental factors, genes, and lifestyle, have some role,...
-

Double Crown Hair: What Is It and What Does It ...
Dr Sadia SaeedMost people have a certain pattern of hair development near the head's crown. The head starts to bend downward towards the rear of the skull at this point. A normal...
Double Crown Hair: What Is It and What Does It ...
Dr Sadia SaeedMost people have a certain pattern of hair development near the head's crown. The head starts to bend downward towards the rear of the skull at this point. A normal...
-

Topical Finasteride: Does It Work for Hair Loss?
Dr Sadia SaeedHair loss is a common problem that affects millions of people all over the world. It has many different causes that range from non-modifiable causes such as age and genetics...
Topical Finasteride: Does It Work for Hair Loss?
Dr Sadia SaeedHair loss is a common problem that affects millions of people all over the world. It has many different causes that range from non-modifiable causes such as age and genetics...