Casein Intolerance & Allergies - Symptoms, Testing and Causes


Related products
The importance of understanding casein intolerance and allergies
Understanding casein intolerance and allergies is crucial for the health and well-being of those affected by these conditions. Both issues can cause adverse reactions to dairy products and other casein-containing foods, but they stem from different physiological mechanisms. Proper identification and management can help individuals avoid discomfort and maintain a balanced diet. For individuals unsure of their symptoms, consider a Combined Allergy and Intolerance Blood Test to help with early identification.
The role of casein in dairy products
Casein is a major protein found in dairy products, accounting for approximately 80% of the total protein content in cow's milk. It plays a vital role in the structure, texture, and nutritional value of dairy products, as well as their potential allergenicity for some individuals .To learn more about Allergies, read our comprehensive guide that covers: Allergies:, Types, Causes, Symptoms, Diagnosis, and Treatment options. If you are looking for treatments for hay fever or general allergens, then visit our extensive page with allergy and hayfever medication and tablets.
Casein: An Overview
What is casein?
Definition and properties
Casein is a family of phosphoproteins found in mammalian milk. It is composed of several subunits, including alpha, beta, and kappa caseins. The protein has a unique structure, which allows it to form micelles – large, spherical structures that play a role in the digestion and absorption of nutrients in the gastrointestinal tract.
Sources of casein in food
Main dietary sources include cow's milk, cheese, yoghurt, and butter. Casein may also be added to processed foods as a stabilizer or protein supplement. If you're unsure of how your body reacts to casein, consider taking a Food Intolerance Test to confirm potential triggers.
The role of casein in nutrition
Protein content
Casein is a high-quality protein source, containing all nine essential amino acids required by the human body for proper growth and maintenance. Its slow digestion rate allows for a sustained release of amino acids into the bloodstream, which can be particularly beneficial for muscle repair and growth.
Impact on digestion and absorption
The unique structure of casein micelles allows them to form a clot or curd in the stomach, which slows down the rate at which the protein is digested and absorbed. This slow-release property of casein can be beneficial for maintaining a steady supply of amino acids to the body over an extended period, potentially aiding in muscle recovery and growth, as well as appetite control. If you're experiencing digestive discomfort or want to explore potential sensitivities, you can browse a range of intolerance tests to better understand how your body reacts to casein and other common food components.
Casein Allergy
Definition and causes of casein allergy
Immune system response
Casein allergy is a type of food allergy where the immune system mistakenly identifies casein proteins as harmful substances and mounts an immune response against them. This reaction can lead to the release of histamine and other inflammatory substances, causing a range of symptoms.
Genetic factors
A predisposition to food allergies, including casein allergy, can be inherited. Individuals with a family history of allergies or atopic diseases, such as asthma, eczema, or hay fever, may be at an increased risk of developing a casein allergy.
Symptoms of casein allergy
Symptoms of casein allergy can vary from person to person, and may include respiratory, gastrointestinal, skin reactions, and in some cases, anaphylaxis. These symptoms can occur within minutes to hours after consuming casein-containing foods.
Respiratory symptoms
Respiratory symptoms associated with casein allergy may include nasal congestion, runny nose, sneezing, coughing, wheezing, and difficulty breathing. In some cases, these symptoms can be severe and require medical attention.
Gastrointestinal symptoms
Gastrointestinal symptoms of casein allergy can include abdominal pain, nausea, vomiting, diarrhoea, and bloating. These symptoms can cause significant discomfort and may interfere with daily activities.
Skin reactions
Skin reactions associated with casein allergy can include hives, itching, redness, and eczema. These symptoms can be uncomfortable and may persist for several hours or even days after exposure to casein.
Anaphylaxis
In rare cases, casein allergy can lead to anaphylaxis, a severe and potentially life-threatening allergic reaction. Symptoms of anaphylaxis can include rapid heartbeat, difficulty breathing, swelling of the face and throat, dizziness, and loss of consciousness. Anaphylaxis requires immediate medical attention and can be fatal if left untreated.
Diagnosis of casein allergy
Diagnosis of casein allergy typically involves a combination of medical history, physical examination, and allergy testing.
Medical history and physical examination
During the initial consultation, a healthcare professional will gather information about the patient's symptoms, their onset, and any potential triggers. They will also perform a physical examination to assess the patient's overall health and identify any signs of an allergic reaction.
Skin prick tests
Skin prick tests involve the application of a small amount of casein extract to the skin, usually on the forearm or back. A needle is then used to prick the skin through the extract, allowing it to enter the skin's surface. If the patient is allergic to casein, a raised, red, itchy bump called a wheal will appear within 15 to 30 minutes.
Blood tests
Blood allergy tests can help detect the presence of specific immunoglobulin E (IgE) antibodies in response to casein. High levels of casein-specific IgE antibodies may indicate an allergy to casein. However, blood tests alone are not sufficient for a definitive diagnosis, as false-positive results can occur. Blood tests are often used in conjunction with skin prick tests and other diagnostic tools.
Elimination diets
Elimination diets involve removing all sources of casein from the patient's diet for a specified period, typically 2-4 weeks. If symptoms improve during this time, casein is then gradually reintroduced to determine whether the symptoms return. This process can help confirm a casein allergy or intolerance and assist in identifying specific trigger foods.
Casein Intolerance
Definition and causes of casein intolerance
Lack of lactase enzyme
Casein intolerance is a non-immunological response to casein proteins, often caused by an inability to properly digest and absorb these proteins. This can occur due to a lack of lactase enzyme, which is responsible for breaking down lactose, a sugar found in milk and dairy products. When lactose is not adequately digested, it can lead to gastrointestinal symptoms. Often linked to lactose intolerance, where the body cannot properly digest dairy sugars. A Premium Intolerance Test can help pinpoint specific sensitivities.
Genetic factors
Genetic factors can contribute to casein intolerance. For example, some individuals may inherit a reduced ability to produce lactase, resulting in lactose intolerance. Additionally, some genetic variations have been associated with an increased risk of developing casein intolerance.
Symptoms of casein intolerance
Casein intolerance can cause various symptoms, primarily gastrointestinal in nature. In some cases, skin reactions may also occur.
Gastrointestinal symptoms
Gastrointestinal symptoms of casein intolerance can include abdominal pain, bloating, gas, diarrhoea, and nausea. These symptoms typically occur within a few hours of consuming casein-containing foods and can vary in severity.
Skin reactions
Although less common, some individuals with casein intolerance may experience skin reactions, such as rashes or itching, after consuming casein-containing foods.
Diagnosis of casein intolerance
Diagnosing casein intolerance typically involves a combination of medical history, physical examination, and diagnostic tests.
Lactose intolerance tests
Lactose intolerance tests, such as the lactose tolerance test or lactose breath test, can help determine whether lactose intolerance is the cause of the patient's symptoms. These tests involve measuring the body's ability to digest lactose and can be useful in identifying casein intolerance due to lactose malabsorption.
Hydrogen breath tests
Hydrogen breath tests measure the amount of hydrogen in the breath after consuming a casein-containing food. High levels of hydrogen can indicate incomplete digestion and absorption of casein, which may be indicative of casein intolerance.
Stool acidity tests
Stool acidity tests can help detect undigested lactose in the stool, which can be a sign of casein intolerance. This test is less commonly used but can provide valuable information in some cases.
Elimination diets
As with casein allergy, elimination diets can be useful in diagnosing casein intolerance. By removing casein-containing foods from the diet and monitoring symptom improvement, healthcare professionals can determine whether casein intolerance is the likely cause of the patient's symptoms.
Management and Treatment
Management and treatment of casein intolerance primarily involve dietary modifications and lifestyle adjustments.
Avoidance of casein-containing foods
The primary treatment for casein intolerance is to avoid consuming foods that contain casein. This can be achieved by:
Reading food labels
Carefully reading food labels is essential to identify and avoid casein-containing foods. Casein can be listed as milk protein, milk solids, or simply as casein on food labels.
Identifying high-risk foods
Some common high-risk foods that may contain casein include milk and milk products, such as cheese, yogurt, and ice cream. Additionally, casein may be found in processed foods, such as baked goods, chocolate, and salad dressings.
Alternative sources of calcium and protein
Individuals with casein intolerance need to ensure they obtain adequate calcium and protein from alternative sources. Some options include: Calcium-fortified plant-based milks, such as almond, soy, or oat milk Leafy green vegetables, like kale, spinach, and broccoli Fish with soft bones, such as sardines and salmon Tofu and other soy-based products Nuts and seeds, like almonds and chia seeds Incorporating these foods into the diet can help individuals with casein intolerance maintain optimal nutrition while avoiding casein-containing foods.
Non-dairy sources of calcium
Apart from the calcium-fortified plant-based milks and leafy green vegetables mentioned earlier, other non-dairy sources of calcium include: Fortified cereals and grains Legumes, such as beans and lentils Oranges and other calcium-rich fruits Seaweed, like kelp and dulse Including these foods in the diet can help individuals with casein intolerance meet their daily calcium requirements.
Plant-based protein sources
In addition to tofu and soy-based products, other plant-based protein sources include: Quinoa, a complete protein grain Legumes, such as chickpeas, lentils, and black beans Tempeh, a fermented soybean product Seitan, a wheat-based protein source Nuts, seeds, and nut butters, like peanut butter and almond butter Incorporating these plant-based protein sources can help individuals with casein intolerance maintain a balanced diet without relying on casein-containing foods.
Medication
In some cases, medication may be helpful in managing the symptoms of casein intolerance and allergies.
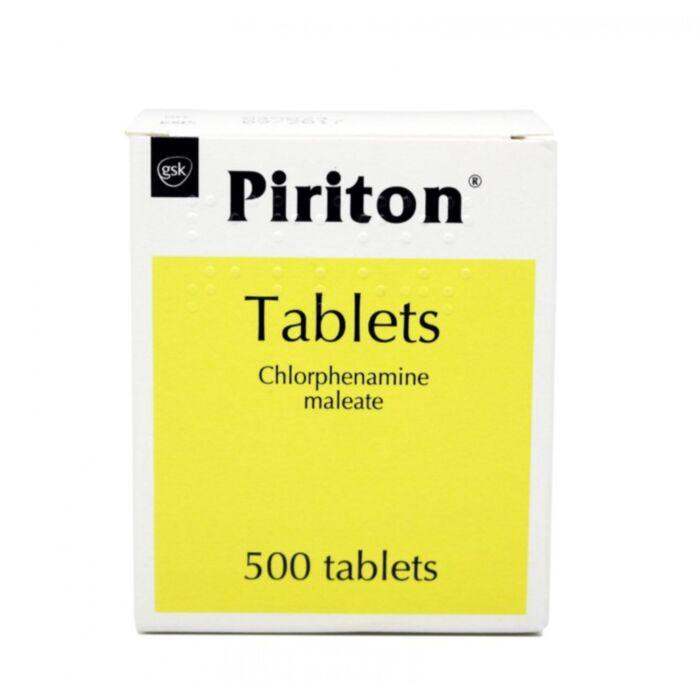
Antihistamines for allergy symptoms
Antihistamines can help alleviate some of the symptoms associated with casein allergy, such as itching, hives, and swelling. It is important to consult a healthcare professional before using antihistamines to ensure they are appropriate for the individual's specific allergy symptoms.
Lactase supplements for intolerance symptoms
For individuals with casein intolerance due to lactose malabsorption, lactase supplements can help break down lactose and alleviate some gastrointestinal symptoms. These supplements should be taken as directed by a healthcare professional.
Lifestyle changes
Managing casein intolerance and allergies often requires making specific lifestyle changes.
Communicating allergy or intolerance to restaurants and food providers
Informing restaurants and food providers about one's casein allergy or intolerance can help ensure that meals are prepared without casein-containing ingredients. This can help reduce the risk of accidental exposure and associated symptoms.
Building a support network
Creating a support network of friends, family members, and healthcare professionals can be beneficial for individuals with casein intolerance or allergies. This support can provide guidance, encouragement, and assistance in managing dietary restrictions and coping with the challenges of living with a food allergy or intolerance.
Conclusion
The importance of understanding casein intolerance and allergies
Understanding the differences between casein intolerance and allergies is crucial for proper diagnosis, management, and treatment. Recognising the symptoms, causes, and appropriate interventions can help individuals affected by casein intolerance or allergies maintain a healthy, balanced diet and reduce the risk of adverse reactions.




















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews