Can Hayfever Cause Nosebleeds?


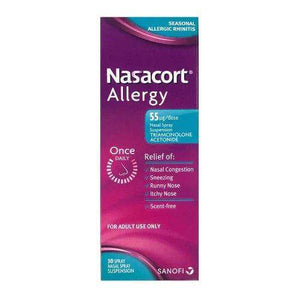
Related products
Hay fever, medically termed allergic rhinitis, is an allergic response to outdoor or indoor allergens such as pollen, dust mites, or pet dander. This condition is prevalent, affecting a significant proportion of the population, particularly during peak pollen seasons. Symptoms typically include sneezing, itchy and watery eyes, and a runny or congested nose. Given these manifestations, this article aims to explore a less frequently discussed aspect of hay fever: its potential to induce nosebleeds, known medically as epistaxis. The exploration is rooted in understanding the delicate interplay between nasal health and allergic reactions facilitated by hay fever.
What is Hay Fever?
Hay fever is triggered by the immune system's response to airborne allergens. Pollen from trees, grasses, and weeds; dust mites from household dust; and pet dander from animals are the primary provocateurs. Upon inhalation of these allergens, susceptible individuals experience an immune reaction that leads to the release of histamine and other chemicals, causing inflammation and symptoms associated with hay fever.
Dr. Emily Foster, a consultant allergist, explains, "The hyperactivity of the nasal passage due to allergens is profound in hay fever patients, leading to symptoms that significantly impact their quality of life." This inflammation is pivotal as it sets the stage for further complications such as nasal dryness and potential bleeding.
Typical Symptoms of Hay Fever
The hallmark symptoms of hay fever include sneezing, itchy eyes, and nasal congestion. These symptoms result from the body's inflammatory response to the allergens. Nasal congestion, in particular, is caused by the swelling of nasal passages, which impedes normal airflow and leads to significant discomfort.
"Chronic inflammation from allergens can disrupt the integrity of the nasal membranes, making them more susceptible to irritation," states Dr. Foster. This persistent irritation can exacerbate the nasal lining, heightening the risk of nosebleeds in affected individuals.
What Causes Nosebleeds?
Epistaxis, or nosebleeds, occur when the delicate blood vessels in the nasal mucosa rupture. These incidents can range from minor to severe and are influenced by various factors. In the context of hay fever, understanding how these typically benign occurrences might relate to allergic reactions is critical.
Nosebleeds can be precipitated by several factors including dry air, which desiccates the nasal membranes, trauma to the nose, certain medications that affect blood clotting, and other health conditions that alter the nasal environment or blood vessels.
Dr. Alan Hayes, a specialist in otolaryngology, notes, "While there are many causes for nosebleeds, environmental factors combined with individual health conditions can significantly elevate the risk." These insights are essential in linking the occurrence of nosebleeds with hay fever.
What is the Connection Between Hay Fever and Nosebleeds?
The connection between hay fever and nosebleeds is primarily through the mechanism of nasal inflammation and frequent nose blowing. "Frequent nose blowing can exert pressure on the already inflamed and sensitive nasal vessels, often leading to ruptures," Dr. Hayes remarks. Additionally, the chronic nasal inflammation seen in hay fever sufferers can weaken the nasal membranes, making them more prone to bleeding.
Allergens like pollen can exacerbate nasal dryness and irritation. The body's response to fight these allergens often involves overproduction of mucus, which paradoxically can dry out the nasal passages. The constant irritation from allergens and the resultant dryness can make the nasal tissue brittle and more likely to bleed.
While antihistamines and other hay fever treatments are designed to alleviate symptoms by suppressing the immune response, they can also contribute to drying out the nasal passages. Dr. Foster advises, "Patients should be aware of the drying effects of some antihistamines and consider using nasal saline sprays to maintain moisture in the nasal passages."
This comprehensive understanding of the physiological interactions between hay fever and the nasal environment underscores the importance of integrated care in managing symptoms and preventing complications such as nosebleeds.
Preventing and Managing Nosebleeds During Hay Fever Season
Managing hay fever effectively is crucial to reducing the frequency of nosebleeds. Dr. Alan Hayes recommends several preventive measures: "Keeping windows closed during high pollen days to limit allergen exposure, using air purifiers at home, and staying hydrated can all help maintain the integrity of the nasal passages." Additionally, gentle nasal care practices such as avoiding excessive nose blowing and using soft tissues can minimize nasal trauma.
To combat nasal dryness, saline nasal sprays or gels can be employed to keep the nasal lining moist. Dr. Emily Foster suggests, "Saline solutions not only help in hydrating the nasal passages but also in clearing allergens that stick to the nasal walls." For home remedies, using a humidifier at night to keep the air moist and applying a small amount of petroleum jelly to the edges of the nostrils can also reduce dryness. Learn more about Hay Fever Injections: Side Effects, Costs and How Does it Work?
While occasional nosebleeds might not typically warrant concern, frequent or severe episodes during hay fever season are a signal to seek medical advice. "Persistent nosebleeds could be a sign of an underlying disorder or an indication that hay fever is not being managed effectively," states Dr. Hayes. Medical intervention is essential to rule out other causes and to potentially adjust allergy medications.
Expert Opinions and Studies on the Connection Between Hay Fever and Nosebleeds
Medical professionals agree that while hay fever primarily causes inflammation and irritation of the nasal passages, these conditions do predispose patients to nosebleeds. The chronic inflammation associated with hay fever weakens the nasal membranes, making them susceptible to bleeding from minor irritations or trauma.
Recent studies have shown varying results. Some research indicates a significant increase in the incidence of nosebleeds among patients with severe allergic rhinitis compared to those without allergies. However, other studies suggest that while there is an increase in nasal dryness and irritation, the actual frequency of nosebleeds may not be significantly higher. These discrepancies highlight the need for further research to understand fully the dynamics between hay fever and nosebleeds.
People Also Ask
Can High Pollen Cause Nose Bleeds?
Yes, high pollen levels can exacerbate hay fever symptoms leading to increased inflammation and nasal dryness, which may cause nosebleeds in some individuals.
Do Antihistamines Help Nosebleeds?
Antihistamines are not typically used to treat nosebleeds directly; they can reduce the severity of hay fever symptoms. However, they might contribute to nasal dryness, potentially worsening nosebleeds unless counteracted with moisturizing treatments.
Can Hay Fever Cause Headaches and Nosebleeds?
Hay fever can indeed lead to headaches and nosebleeds. Headaches often result from sinus pressure due to blocked nasal passages, and the same inflammation can increase the likelihood of nosebleeds.
How Long Do Allergy Nose Bleeds Last?
Allergy-induced nosebleeds usually last a few minutes but can be recurrent. Keeping the nasal area moist and treating the underlying allergy symptoms is key to reducing their frequency and duration.
Conclusion
The correlation between hay fever and the incidence of nosebleeds, while evident in certain aspects, requires awareness and proactive management. Understanding and addressing the underlying nasal inflammation and dryness through appropriate treatments and lifestyle adjustments can significantly mitigate the risk of nosebleeds. Continuous research and clinical insights are vital to enhancing our management strategies, ensuring that individuals with hay fever can lead more comfortable lives during allergy seasons.

























 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews