
 Instagram
Instagram
Hormonal Contraception and Risk of Breast Cancer

Related products
Hormonal Contraception: An Overview
Definition and types of hormonal contraception
Hormonal contraception comprises methods that utilise hormones to prevent ovulation and hence, pregnancy. The hormonal contraception family includes birth control pills, contraceptive patches, injections, implants, and vaginal rings. These vary in their hormone types, delivery methods, and frequency of use, but all aim to provide reliable contraception for women.
Brief explanation of how hormonal contraceptives work
Hormonal contraceptives work primarily by releasing synthetic versions of female hormones (estrogen and/or progestin) that inhibit ovulation, the release of an egg from the ovaries. They also thicken cervical mucus, making it more difficult for sperm to reach an egg, and thin the lining of the uterus, making it less hospitable for a fertilised egg. "The hormones in these contraceptives essentially trick the body into thinking it's already pregnant, thereby preventing actual pregnancy", states Dr. Sophia Yen.
Popularity and convenience of hormonal contraception
In the UK, hormonal contraception has seen widespread adoption due to its convenience and effectiveness. Over 3.1 million women use hormonal contraception methods, with the contraceptive pill being the most popular choice, according to a 2020 report from the Faculty of Sexual & Reproductive Healthcare. The popularity of these methods is a testament to their convenience and efficacy in preventing unwanted pregnancies.
Understanding the Breast Cancer Risk
Overview of breast cancer: what it is and how it develops
Breast cancer is a malignant tumour that originates from the cells of the breast. The disease typically begins in the ducts that transport milk to the nipple or the lobules, the glands that produce milk. It can spread beyond the original tumour to nearby lymph nodes and other areas of the body. Breast cancer is the most common cancer in the UK, accounting for 15% of all new cancer cases in 2018, according to Cancer Research UK.
Brief look at factors contributing to breast cancer risk
There are numerous factors that contribute to breast cancer risk, including age, family history, early menstruation, late menopause, later age at first childbirth, and certain gene mutations. The potential influence of hormonal contraception on breast cancer risk has also been a topic of considerable research and debate in recent years. "Understanding the full range of risk factors for breast cancer is essential in our efforts to tackle this disease", as Professor David Hunter.
Hormonal Contraception: Unpacking the Breast Cancer Risk
Detailed look at studies and research linking hormonal contraception and breast cancer
A number of studies have attempted to discern the relationship between hormonal contraception and breast cancer. A landmark Danish study published in the New England Journal of Medicine in 2017 found a small but significant increase in breast cancer risk among women using hormonal contraception compared to those who did not. "While the overall risk remains low, the study findings reinforce the importance of considering all potential risks and benefits of hormonal contraception", highlights Dr. Marisa Weiss,
How different types of hormonal contraceptives may contribute to the risk
It's important to understand that not all hormonal contraceptives carry the same risk. Research has indicated that combined hormonal contraceptives, containing both estrogen and progestin, may present a slightly higher risk than progestin-only methods. "The increased breast cancer risk appears to be associated with prolonged exposure to higher levels of hormones found in some types of hormonal contraceptives", as stated by Dr. Deirdre Tobias. More research is required to fully understand this complex relationship, but these findings contribute to an ever-evolving dialogue around hormonal contraception and breast cancer risk.
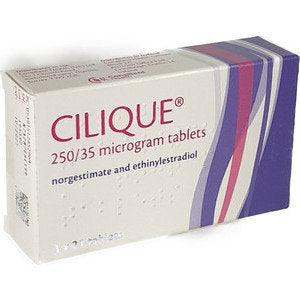
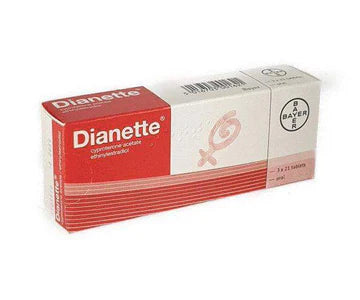
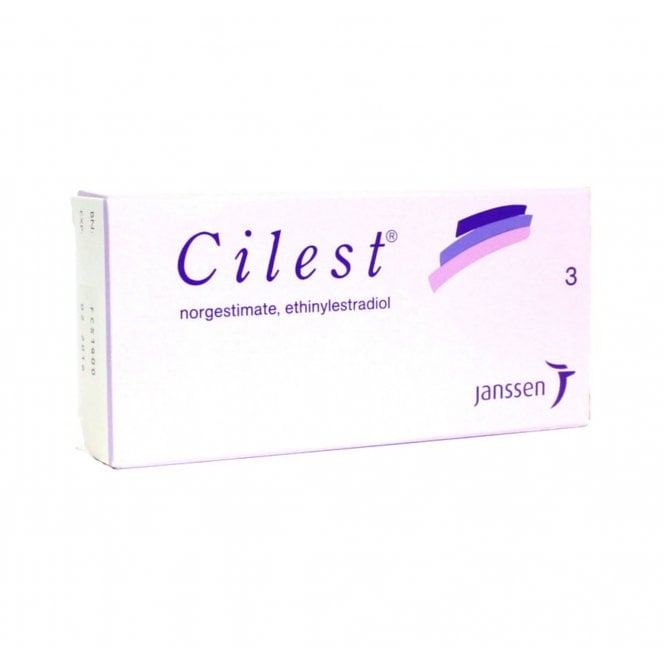
Combined Hormonal Birth Control Pills and Breast Cancer Risk
Explanation of how combined pills work
Combined hormonal birth control pills, often simply referred to as "the pill", contain synthetic versions of both estrogen and progesterone. They work by inhibiting ovulation, thickening the cervical mucus to prevent sperm penetration, and thinning the lining of the uterus to inhibit fertilized egg implantation.
Details of studies linking combined pills to breast cancer
Studies have reported an increased risk of breast cancer in women who use combined oral contraceptives. For example, the aforementioned Danish study published in the New England Journal of Medicine indicated a small but significant increase in breast cancer risk among users of combined pills.
Assessing the degree of risk
The degree of increased risk is small, but not negligible. "It is important for women to weigh this increased risk against the benefits of combined pills, such as highly effective contraception and potential reduced risk of ovarian and endometrial cancers" explains Dr. Deirdre Tobias.
Progestin-Only Pills and Breast Cancer Risk
Explanation of how progestin-only pills work
Progestin-only pills (POP), also known as mini-pills, contain only one hormone, progestin. They function by thickening the cervical mucus, preventing sperm from reaching the egg, and also by thinning the uterine lining, making it less likely for a fertilised egg to implant and grow.
Details of studies linking progestin-only pills to breast cancer
Research into the link between progestin-only pills and breast cancer has yielded mixed results. While some studies suggest a slightly increased risk, others have found no significant link. As such, further research is needed to clarify this potential association.
Assessing the degree of risk
Given the inconclusive nature of current research, it's difficult to precisely determine the degree of risk associated with POP use. However given their lower hormonal dosage, the risk associated with progestin-only pills may be less than that associated with combined pills.
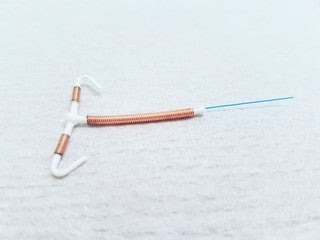
Intrauterine Devices (IUDs) and Breast Cancer Risk
Explanation of how hormonal IUDs work
Hormonal Intrauterine Devices (IUDs) release progestin directly into the uterus, preventing pregnancy by thickening the cervical mucus, thinning the uterine lining, and potentially inhibiting ovulation.
Details of studies linking hormonal IUDs to breast cancer
Research on the link between hormonal IUDs and breast cancer is still developing. Some studies suggest a small increase in risk, particularly for a specific type of breast cancer known as hormone-receptor-positive breast cancer. However, the overall risk remains relatively low and more research is needed .
Assessing the degree of risk
The degree of breast cancer risk associated with hormonal IUD use is currently not definitively established. While some studies suggest a small increase in risk, this must be balanced against the many benefits of IUDs, including their effectiveness and long-acting nature.
Contraceptive Implants and Breast Cancer Risk
Explanation of how contraceptive implants work
A contraceptive implant is a small flexible rod that is placed under the skin of the upper arm. It releases progestin into the body, preventing ovulation, thickening the cervical mucus to stop sperm reaching an egg, and thinning the uterine lining.
Details of studies linking contraceptive implants to breast cancer
Research regarding the link between contraceptive implants and breast cancer is not extensive, and current studies have not conclusively determined an increased risk. Further studies are needed to elucidate this potential relationship.
Assessing the degree of risk
The degree of risk associated with contraceptive implants is currently undefined due to the limited research. As with all forms of hormonal contraception, the potential risk must be considered in light of the benefits, such as high effectiveness and long-term convenience.
Contraceptive Injections and Breast Cancer Risk
Explanation of how contraceptive injections work
Contraceptive injections, such as Depo-Provera, deliver a high dose of progestin. They work by preventing ovulation, thickening the cervical mucus to stop sperm from reaching an egg, and thinning the uterine lining.
Details of studies linking contraceptive injections to breast cancer
Research on contraceptive injections and breast cancer risk has produced mixed results. Some studies suggest a slightly increased risk, while others find no significant association. Further research is necessary to establish a clearer understanding of the potential risk.
Assessing the degree of risk
Given the current state of research, the degree of breast cancer risk associated with contraceptive injections remains uncertain. "consider the current evidence and discuss personal risk factors with their healthcare provider", says Dr. Marisa Weiss.
Non-Hormonal Contraception Options
Brief overview of non-hormonal contraception options
For those concerned about the potential risks of hormonal contraceptives, there are various non-hormonal options available, including condoms, female condoms, copper IUDs, diaphragms or caps, and fertility awareness methods.
Considerations for individuals concerned about breast cancer risk
Individuals with a higher risk of breast cancer may wish to consider non-hormonal options. "Choosing a non-hormonal method can be a reasonable decision for those with a high risk of breast cancer, particularly when coupled with regular screening and other risk-reducing strategies", says Dr. JoAnn Manson.
Making Informed Decisions about Hormonal Contraception
Discussion on the importance of considering individual risk factors
Each individual's risk of breast cancer is influenced by a combination of factors, including age, genetics, lifestyle, and reproductive history. When considering hormonal contraception, it's important to assess these individual risk factors in consultation with a healthcare provider.
Strategies for mitigating risk: regular screenings, lifestyle changes, etc.
While hormonal contraception can slightly increase breast cancer risk, other modifiable risk factors can be addressed to help mitigate this risk. Regular exercise, maintaining a healthy weight, reducing alcohol consumption, and breast cancer screenings are all strategies recommended by the Cancer Research UK.
Role of healthcare providers in helping make informed decisions
Healthcare providers play a crucial role in guiding patients through the process of making informed decisions about contraception. A comprehensive discussion about the potential risks and benefits, taking into account individual circumstances and preferences, is key to finding the most appropriate method for each individual.
Conclusion
Recap of the connection between hormonal contraception and breast cancer risk
The connection between hormonal contraception and breast cancer risk is complex, with research indicating a slight but significant increase in risk. It's important to remember that risk is individual and multifactorial, and hormonal contraception is just one piece of the puzzle.
Final thoughts on the importance of informed decision-making
Making decisions about contraception is a personal process and should be based on a comprehensive understanding of the potential risks and benefits. A healthcare provider can provide invaluable guidance in this process, helping individuals make decisions that align with their health goals and lifestyle.
Encouraging readers to continue learning and researching their options
As knowledge about the link between hormonal contraception and breast cancer continues to evolve, it's important to stay informed and be proactive in understanding the potential implications for personal health. Resources such as the Breast Cancer Organisation and Cancer Research UK can provide updated information and research findings.
Call to action for regular health checks and discussions with healthcare providers.
Regular health checks and open discussions with healthcare providers are essential in managing personal health and making informed decisions about contraception. Don't hesitate to raise any concerns or questions you may have about hormonal contraception and breast cancer risk with your healthcare provider.
















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews