What are the Best Sleeping Position for Peripheral Artery Disease?

Related products
Peripheral Artery Disease (PAD) is a circulatory issue where constricted blood vessels lead to reduced blood flow in the limbs. The main risk factor behind PAD is atherosclerosis, characterised by plaque buildup that narrows or obstructs arteries. Other prominent risk determinants for this disease include smoking, diabetes, and elevated cholesterol levels.
As per data from the American Heart Association, Peripheral Artery Disease affects 8.5 million US residents, with risks escalating as one grows older. More worryingly than these figures imply, those suffering from PAD are at heightened risk of coronary artery disease and cerebrovascular disease—both can potentially result in heart attacks or strokes.
Typical symptoms include muscle pain or cramping while walking but vanishing during rest periods; however, some people show no signs at all, making it more difficult since unnoticed progression may lead to severe consequences like stroke if left untreated for too long.
Physicians usually diagnose peripheral artery disease through physical examination, including checking pulse rates along leg arteries, followed by diagnostic tests such as the ankle-brachial index test and Doppler ultrasound, among others.
Management strategies involve lifestyle adjustments encouraging exercise & quitting smoking aided with specific medicines prescribed, mainly statins, alongside surgical intervention when required per the patient's condition severity.
When managing conditions like Peripheral arterial diseases, beyond medical treatments, personal habits indeed play pivotal roles. Adequate knowledge about proper sleep postures contributed tremendously to comfort maximization, thereby indirectly helping maintain good health overall.
What is Peripheral Arterial Disease?

Peripheral Arterial Disease, commonly known as PAD, is a circulatory problem in which narrowed arteries restrict blood flow to the limbs. It is primarily caused by atherosclerosis—the accumulation of fatty deposits on artery walls—and often results in reduced circulation to the legs and feet.
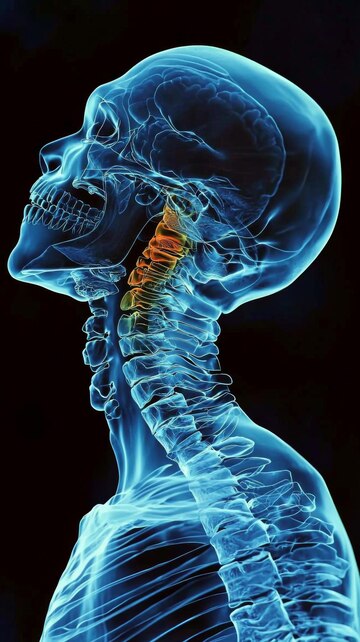
Narrowing or blockage of these peripheral arteries leads to decreased blood flow, affecting limb health primarily due to inadequate oxygen supply for cellular function, necessitating healthy blood movement. While PAD most frequently impacts the legs compared to arms or other parts of the body, when severe enough, it might signal more widespread arterial disease throughout the body — indicating an escalated risk for heart attack or stroke.
Causes Of Peripheral Arterial Disease
Peripheral Arterial Disease is primarily caused by several factors, each contributing to its development and progression.
- Atherosclerosis: Derived from the Greek words' there's—meaning gruel or paste—and 'sclerosis'—translating into hardness—atherosclerosis refers to the hardening and narrowing of arteries due to the accumulation of fatty deposits on their inner walls over time. This condition restricts normal blood flow rate through narrowed regions, potentially leading to PAD if not addressed in a timely manner.
- Smoking: Regular intake of tobacco, either via smoking or other forms, initiates damage in the lining structure within arterial walls, enhancing atherosclerotic processes - thereby increasing the risk for developing PAD among regular smokers compared with non-smokers, keeping other variables constant.
- Diabetes: High glucose levels associated with diabetes inflict direct injury onto arterial walls, expedited even more so when poorly controlled, as greater sugar content contributes towards quicker plaque formation, further advancing risks for circulatory diseases like PAD.
- Hypertension (High Blood Pressure): Consistent high pressure against arterial wall interiors accelerates wear & tear, eventually triggering inflammatory responses and initiating a cascade, ultimately ending up forming plaques referred to under the term 'Atherogenesis', which concerning PAD has been substantially demonstrated across numerous research studies.
- High cholesterol: Uncontrolled higher than recommended LDL ('bad') cholesterol accompanied by lower HDL('good') cholesterol along triglycerides facilitate faster plaque build-up.
- Age: Our bodies generally become vulnerable as natural ageing progresses. Exceeding a threshold beyond 50 dramatically increases the chances of contracting ailments, including Peripheral Artery Diseases, irrespective of gender differences.
- Genetic makeup/ Family history: People having close relatives diagnosed, especially first-degree such as parents/siblings, display heightened susceptibility reflective of inherent genetic predisposition.
Whilst these are major triggers, there remain others, too, yet they are still important, influencing overall vulnerability magnitude significantly and warranting preventive health measures adoption at the individual community level.
Symptoms Of Peripheral Arterial Disease
Peripheral Arterial Disease (PAD) manifests through a variety of symptoms, each indicating varying degrees of the disease's progression. Here are common signs associated with PAD:
Painful Cramping: Intense muscle cramps or discomfort in one's hips, thighs or calf muscles after certain activities, such as walking, is often an early sign related to PAD.
Leg Numbness or Weakness: Individuals might experience unexplained leg numbness and weakness on one side, which could be caused by reduced blood flow impacting normal nerve function.
Cold Legs: With compromised circulation comes temperature discrepancies; noticeably colder lower legs compared to other body parts remain another prevalent symptom indicating the likely presence underlying Peripheral Artery Diseases.
Slow healing Sores/ Wounds over Legs/Feet: Since there isn't sufficient healthy blood supply reaching the injury site, proper wound repair gets delayed, hence taking longer time than usual, even for minor injuries.
Colour Change in Skin: Lower limb skin tone unexpectedly turning pale/bluish suggests deteriorating arterial health where inadequate oxygen-rich fresh blood reaches extremities, making tissues appear discoloured.
Hair loss & slow toe-nail growth: Similar reasons like delayed wound recovery contribute towards decreased hair growth rate across legs along sluggish toe-nails since these require steady nutritional flow only possible under normal circulatory conditions.
Erectile dysfunction: Men diagnosed with Peripheral artery diseases relatively exhibit a higher likelihood of encountering erectile problems considering similar basic pathology involved in inducing both.
Diagnosis and Treatment Of Peripheral Arterial Disease
Diagnosis of Peripheral Artery Disease (PAD) follows a sequence involving physical examination and various diagnostic tests.
- Physical Exam: Physicians first observe symptoms and review medical history, followed by careful evaluation, which includes checking the pulse in the legs.
- Ankle-Brachial Index (ABI): Diagnostic procedure to compare blood pressure at ankle level with that measured arm-wise, assisting in identifying potential circulatory problems suggestive of PAD presence.
- Doppler Ultrasound: Imaging study utilising sound waves producing images of arteries highlighting any existing blockages due to plaque build-up.
- Angiography: Involving dye injection via catheter into bloodstream illuminated under X-ray guidance tracing flow pathway identifying narrowed/blocked regions.
For treatment purposes, the following tools are utilised:
- Medications: Drugs such as antiplatelet agents like aspirin or clopidogrel & statins help reduce risk clot formation/manage cholesterol levels, respectively
- Lifestyle Adjustments: Incorporating healthy lifestyle choices, namely diet modifications enforcing better nutrition and regular exercise enhancing overall cardiovascular health, smokers strongly recommended quitting smoking for optimal outcomes.
- Interventional Procedures/Surgery: Reserved severe cases without a satisfactory response to conventional techniques; procedures including angioplasty/stenting bypass surgery restore normal circulation deemed necessary patient's progression severity-wise.
What are the Best Sleeping Positions for Peripheral Artery Disease
Adequate sleep is essential for everyone, especially those with Peripheral Artery Disease (PAD), as specific positions enhance circulation, alleviating discomfort. Here are optimal sleeping position recommendations:
Elevated Legs Position

Peripheral Artery Disease (PAD) is a medical condition characterized by narrowed arteries, which reduces blood flow to the limbs. One helpful strategy in managing PAD symptoms, such as leg pain and cramping, involves adopting certain sleep positions. Specifically - resting with elevated legs.
Resting or sleeping with elevated legs poses several benefits for individuals with Peripheral Artery Disease. Firstly, this position assists in promoting better circulation of blood from the lower extremities back to the heart. The logic stands on simple physics where gravity aids venous return — an advantage that patients get when their feet are above the level of their heart.
Secondly, leg elevation while at rest might help reduce inflammation linked to PAD's progression. Evidence suggests that poor vascular function exacerbates inflammatory responses; lowering these levels potentially improves arterial health over time.
Moreover- deeper insights reveal how elevating legs during rest periods can alleviate discomfort associated with Intermittent Claudication –a common symptom associated with Peripheral Artery disease, implying intermittent muscle pain aggravated by physical activity but relieved upon rest due mostly to insufficient blood flow.
A study published in the Journal of the American Heart Association investigated whether different body postures affect limb hemodynamics among people suffering from Chronic Venous Insufficiency (CVI), another circulatory problem like PAD, often resulting in swollen ankles/feet and tired aching legs. It concluded that raising one's foot 20 cm above heart level increased venous drainage, thus decreasing ambulatory venous hypertension and indirectly proving beneficial against CVI –seemingly supporting pad benefit theory.
The Left-side Position

The left-side sleep position has been associated with several health benefits, including improved circulation, an essential requirement for PAD patients. Left lateral position augments gravitational force promoting venous return from lower limbs back towards the heart – most crucial amidst decreased arterial supply due to narrowed peripheral vessels characteristic of PAD.
Additionally, people suffering from intermittent claudication—another common symptom among PAD patients where inadequate blood flow leads to leg pain during physical activity—might find comfort in resting on their left side since this posture appears favorable for better limb perfusion, thus reducing muscular discomfort upon exertion.
Sleeping Without Crossing Legs
Sleeping without crossed legs fosters improved flow of oxygenated blood throughout body extremities, including lower limbs, which are most affected in peripheral artery disease. The cross-legged position tends to compress veins, potentially impairing optimal venous return back to the heart, thereby likely exacerbating PAD symptoms, especially leg pain, and cramping associated with intermittent claudication. Moreover, choosing not to cross-leg sleeping posture aids against undesirable pooling or clotting risks that might be enhanced owing to obstructed circulatory pathways and detrimental pressure points incurred due to unnatural twists & turns when individuals sleep with their limbs overlapped.
Frequently Asked Questions
How should I sleep with peripheral artery disease?
Individuals with Peripheral Artery Disease need to maintain the right sleep posture, which is recommended mainly by lifting legs slightly higher than heart level. This augments overall circulation due to optimized venous return, using gravity advantageously to ensure ample oxygen supply reaching all parts.
What is the best sleeping position for leg blood flow?
An elevated position proves beneficial for promoting leg blood flow because it counters gravitational pressure, allowing easier movement of deoxygenated blood back towards the heart, ultimately achieving improved circulatory efficiency.
How do you treat peripheral artery disease leg pain at night?
To alleviate pain commonly linked with peripheral artery disease, specifically during night hours, keeping limbs raised and taking prescribed medicines before bed usually helps manage symptoms more effectively for a well-rested wake-up the next morning.
Which sleep is best for blood circulation?
Side sleeping is best for stimulating enhanced blood circulation as this pose doesn't impede gravitational forces required in fluid transportation within veins, thereby accomplishing holistic regulation throughout body systems.
What is the best natural treatment for peripheral artery disease?
Natural treatments incorporate dietary changes by introducing low-fat foods, fibre, and content items that include fruits, vegetables, and whole grains alongside seafood-rich omega-3 fatty acids paired with vitamins B6/B12/C/E, significantly contributing to managing PAD progression.
What is the best exercise for blocked arteries in the legs?
Exercise plays a crucial role, particularly in the lower extremities, where blocked arteries are present. A supervised routine involving treadmill workouts and strength training sessions designed per individual capacity under professional guidance allows gradual stamina build-up, reducing symptom severity over consistent timeframes and substantially enhancing the patient's quality of life.
Summary
Peripheral Artery Disease (PAD) is a circulatory issue with narrowed arteries limiting blood flow to limbs. Atherosclerosis, smoking, diabetes and hypertension constitute key factors resulting in PAD development. Notably, though it primarily affects the legs, it might signal widespread arterial issues leading to heart attacks or strokes.
Optimal sleep positions like elevating legs slightly above heart level and sleeping on one's left side maximize comfort & aid overall symptom management for people dealing with PAD. Lifestyle modifications featuring healthier dietary choices combined with regular physical activity, particularly aerobic exercises, come highly recommended alongside medication under professional medical supervision, providing the best outcomes in managing such conditions effectively and ensuring better health.




























 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews