Luteal phase: Length and how to calculate

Related products
The menstrual cycle, central to a woman's reproductive well-being, is the biological metronome, establishing her fertility chronology. This recurrent pattern initiates from puberty and culminates at menopause — essential thresholds in every female's lifecycle journey.
Typically spanning 28 days - though variations between 21-35 days exist - the menstrual cycle comprises several key phases marked by significant hormonal shifts. The follicular phase (day 1 to day 14) witnesses the maturation of eggs within ovarian follicles; ovulation around day 14 propels the release of the mature egg for fertilization; and finally, the luteal phase sets the stage from day15 through day 28, gearing up uterus lining readying itself for implantation.
A study reveals that subtle hormonal imbalances during the luteal phase have been observed in women diagnosed with strictly classified unexplained infertility when contrasted against fertile counterparts.
Phases Of Menstrual Cycle
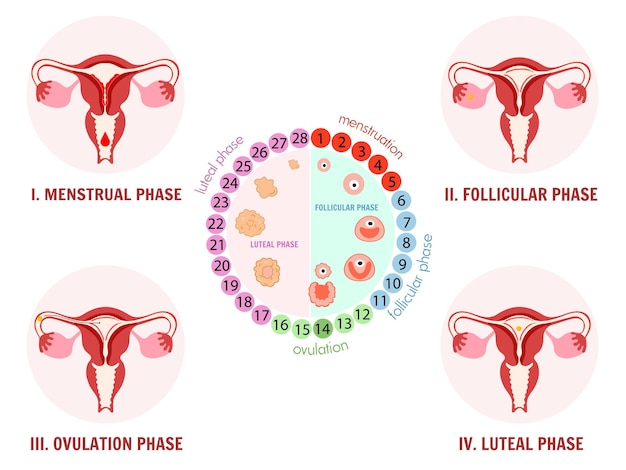
The menstrual cycle, a central part of female reproductive health, consists of several key phases. Distinct hormonal changes spark each phase and play an indispensable role in fertility potential.
Menstrual Phase (Day 1-5)
At the start of this phase, if no fertilized egg implants into the uterus for pregnancy to occur, then menstruation begins—shedding off the thickened lining layer developed within the uterus, marked by bleeding, serving as an indicative sign commencing a new monthly cycle routine.
Follicular Phase (Day 1-13)
During the follicular stage, which runs simultaneously along the initial five-day course with a menses period followed up next until around the thirteenth-day mark, hypothalamus secretion triggers pituitary gland stimulation, leading to the production of hormones that lead to the commencement of the primary ovarian follicle maturation process, which houses immature, awaiting-release eggs.
Ovulation Phase (Around Day14)
Depicting prime fertile window opportunity usually extending one single day long wherein matured ovum leaves ovaries reaching fallopian tube ready towards possible sperm reception event at time intercourse occurrence therein highlighting peak conception likeliness.
Luteal Stage
Spanning between the fifteenth through the final approximated twenty-eighth menstrual cycle, the last stretch involves corpus luteum formation post rupture leftover remnant follicle which aids progesterone hormone excretion supporting uterine lining even further enrichment anticipation implantation provided successful fertilization outcome happens else degeneration results causing onset next flow termed conveniently as periods experienced after every four weekly-set interval lapse completely resetting groundwork anew another hopeful journey wait reproduction miracle unfold again.
What Happens During the Luteal Phase

The luteal phase, extending from day 15 to around day 28 of the menstrual cycle, is characterized by significant hormonal activity. Following ovulation, a corpus luteum structure forms in the ovaries from remnants of the ruptured follicle.
This corpus luteum secretes progesterone hormone, which enriches the uterine lining or endometrium for potential implantation if fertilization occurs. However, without successful egg and sperm fusion noted during this stage, regression starts where the non-functional corpus luteum makes a decrease in hormones till it stops completely, resulting in menstruation onset marking the cessation of one full-cycle round resetting again upcoming course run anew continuing natural progression long-term until menopause arrives, universally among women irrespective geographical dispersion boundaries emphasizing the fact that menstrual cycles constitute defining attribute womanhood existence core foundation aspect element.
A parallel can be drawn here with respect to fertility treatment-seeking couples who might find difficulty realizing family-building dreams due to issues maintaining optimal healthy, balanced hormonal environment facilitating functional ovulatory mechanisms, thereby hinting medical intervention requirement consult immediate effect.
How To Calculate Luteal Phase
Calculating the luteal phase is crucial to fully comprehend and monitor female fertility. Traditionally, this phase extends from day 15 through day 28 of a typical menstrual cycle. However, individual variations are quite common.
Here's how:
- Identify the total length of your complete menstrual cycle, which should be calculated from the first day of menstruation until one day before the next period begins.
- Subtract fourteen (representing an average timing for ovulation post-follicular stage completion), and what remains after gives you the duration of the Luteal Phase accurately, providing insight into the number of days accounting for that particular span within the overall timeline estimate at hand under consideration.
Short And Long Luteal Phases
The luteal phase typically lasts approximately 14 days in an average menstrual cycle. However, differing lengths have been noted.
Short Luteal Phase: A period under twelve days is classified as a short luteal phase, often hinting at 'Luteal Phase Deficiency.' Such a state usually correlates with suboptimal progesterone levels, potentially hindering endometrial development necessary for hopeful embryo nesting that otherwise might translate into early pregnancy termination or miscarriage scenario unfolding.
Long Luteal Phase: Conversely, when this stage stretches over sixteen days duration, marker potential conditions like Polycystic Ovarian Syndrome (PCOS) or irregularities within monthly cycles raise attention-gaining concerns, prompting medical advisement fundamental managing reproductive health aspects ideally in either experience - shortened lengthened phases alike.
Causes of Abnormal Luteal Phase
The luteal phase, a crucial element in female reproductive health, can sometimes exhibit abnormalities. These irregularities often contribute to issues surrounding conception and fertility.
Luteal Phase Defect
Luteal Phase Defect (LPD) pertains to a condition in women’s reproductive health correlated with inconsistent progesterone levels, often obstructing the efficient anchoring of a fertilized egg.
The luteal phase typically witnesses high progesterone secretion, essential for uterus preparation for potential fertilization. If deficient production or sudden drop of such hormones occurs, it impacts the thickness of the uterine lining and thereby impedes healthy pregnancy progression. This effect creates challenges around fertility and natural conception possibilities.
A research article appearing in the Journal of Obstetric, Gynecologic & Neonatal Nursing disclosed that a Luteal phase defect - typified by inadequate progesterone steroidogenesis from corpus luteum - is observed among primary infertility instances and approximately 35% of couples recurrently suffering pregnancy loss.
Symptoms include shorter than usual cycles or spotting between periods—diagnosis relies mainly on the patient's medical history analysis complemented by repeated clinical testing data centered on accurate testosterone level determination.
Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) represents a widespread hormonal imbalance condition impacting women within their fertile years. It frequently results in heightened male hormone presence, instigating disturbances during ovulation phases.
Symptoms range from irregular menstrual cycles and infertility due to non-ovulation to physical changes such as excessive hair growth or acne triggered by high amounts of circulating androgens.
Moreover, PCOS has been associated with insulin resistance, which can lead to weight gain or obesity, increasing the risk for Type 2 Diabetes over time along with prolonged menstrual cycles exceeding 35 days or infrequent menstruations less than eight times per year, suggesting an erratic pattern driven primarily by fluctuating hormones.
Hyperprolactinemia
Overproduction of prolactin interferes with normal functioning hormones like estrogen and progestogen, resulting in potential disturbances predominantly affecting premenstrual cycle stages. Thus, it indirectly influences the length norm associated with one's respective luted days count.
High Levels Of Stress Or Extreme Physical Activity
Intense mental stressors or excessive exercise have substantial effects on physiological functions impacting menstrual regularity, including time frame deviations specifically relating to an individual's perspective and limited course span limits. This further emphasizes how behavior choices substantially impact such parameters, determining fertile capability extent.
How Do I Know If I am In The Luteal phase?

Determining the luteal phase of a menstrual cycle is crucial for fertility tracking. Here are key signs indicating entrance into this stage:
Post-Ovulation Symptoms: Following ovulation, indicators like breast tenderness or slight abdominal discomfort suggest the onset of the luteal phase.
Rise in Basal Body Temperature (BBT): An increase in resting body temperature post-ovulation often signals a transition into premenstrual days.
Progesterone Surge: A dominance of progesterone after ovulation indicates progression into this final leg of a monthly cycle - increased cravings and emotional changes further hint at an approaching menstruation period.
Premenstrual Signs Presence: Symptoms such as bloating, mood swings, or heightened specific food sensitivity confirm that the cycle is nearing its conclusion towards the next flow onset.
Takeaway
Recognizing the luteal phase is critical for monitoring fertility and understanding menstrual health. Key indicators include post-ovulation symptoms, a rise in basal body temperature, progesterone dominance, and premenstrual signs. With such knowledge of physiological changes, effective planning around conception or identifying potential irregularities becomes feasible—underscoring the importance of women's well-being through informed family planning decisions.
Frequently Asked Question
What is the ideal luteal phase length for pregnancy?
The optimal length of the luteal phase conducive to conception generally spans between 12-14 days, facilitating efficient implantation and maintenance of early pregnancy.
How do you calculate menstrual cycle phases?
Calculation commences from day one of menstruation (the start point being the cycle's first day). The follicular phase encompasses this initial bleeding period until ovulation around mid-cycle. Ovulation typically occurs on or about the fourteenth cycle day in a 28-day pattern, marking commencement towards the subsequent luteal stage lasting through the impending menstrual flow start next turn course.
What is the standard luteal phase?
Universally recognized standard luteal phase duration maintains an approximate range limit countdown constituting roughly half monthly-cycle stretch accounting for the last two weeks timeline span chartered figure set mark typical expectancy boundary is drawn line discreetly separating follicular from premenstrual time zone slots distinctly apart individually classified separate divide group partition sectioning clearly.
What is the average luteal phase length for a 29-day cycle?
In such cycles, an average luteal stage maintains roughly a half-month course timeline, similar to others.























 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews