Asthma-COPD Overlap: Definitions, Symptoms, Causes, Diagnosis and Treatment
Related products
Asthma-COPD Overlap Overview
For many years, asthma and Chronic Obstructive Pulmonary Disease (COPD) were perceived as distinct disorders with specific symptoms, causes, and treatment strategies. Recent studies, however, challenge this traditional dichotomy by revealing overlaps between the two conditions - an area of interest in scientific research that has led to the emergence of a new term: Asthma-COPD Overlap.
Asthma COPD Overlap (ACO), also known as ACOS or Asthma-Overlap Syndrome, is characterized by persistent airflow limitation with several features usually associated with asthma and COPD. Those diagnosed often face more substantial health complications than those suffering from either condition alone, thus making its understanding crucial for effective patient care.
This article will explore ACO definitions and potential symptoms patients might encounter. We'll delve into probable causative factors contributing to its occurrence before moving on to diagnostic practices clinicians employ when suspecting such overlapped cases. Afterwards, we'll evaluate existing treatment approaches designed to cater to these particular medical situations unfolding at the junction between two historically separate but frequently coexisting airway diseases.
What is Asthma-COPD Overlap?
The term "Asthma-COPD Overlap" refers to the clinical condition presenting features from asthma and Chronic Obstructive Pulmonary Disease (COPD). It's a complex syndrome exhibiting persistent airflow obstruction, which isn't fully reversible.
Patients with ACO face significantly worse respiratory symptoms and health-related quality of life than those living only with COPD or asthma alone, thus emphasising the need for effective therapeutic strategies tailored towards this specific overlap.
The World Health Organization’s ICD-10 characterises both under the chronic obstructive pulmonary disease category but distinguishes them based on significant differences. Even though their primary differentiation remains unclear medically due to the overlapping shared features, such as progressive lung disorders causing difficulty in breathing. It's important here to understand individually what constitutes Asthma and COPD:
Asthma: is an inflammatory disease commonly diagnosed in childhood that narrows airways episodically. In other words, individuals experience periods of relative normalcy punctuated by shortness of breath caused by inflammation-induced contraction (spasm) in bronchial muscles surrounding the lungs' airway passages.
COPD: Unlike the episodic nature seen in asthmatics, patients suffering chronic obstructive pulmonary disease endure constant narrowing coupled with progressive deterioration over time primarily due to the destruction of lung tissue referred to as 'Emphysema' or abnormal thickening lining these tiny brachial tubes leading to the formation of excessive mucus termed 'Chronic Bronchitis'. While being two separate entities under the umbrella term COPD, chronic bronchitis and emphysema typically coexist, presenting a progressive disease with increased breathlessness over time.
Now that we've laid out definitions for asthma and COPD individually, it's easier to grasp what ACO signifies. It represents patients with an 'overlap' of symptoms from both conditions. For instance, these individuals might exhibit variability in their airway obstruction episodes (characteristic of asthma) but also face constant narrowed lung passageways/intensity worsening over time (metaphoric to COPD). There are more severe health impairments and hospitalisation risks compared with either Asthma or COPD occurring individually.
Evidence suggests approximately 15-45% of COPD patients may demonstrate asthmatic features, while 20-30% of Asthma patients may exhibit COPD-like symptoms. This results in a considerably large population potentially being at risk for ACO, often leading to higher healthcare utilisation due to more severe exacerbations.
This overlapping nature often leads clinicians towards unique challenges for correctly diagnosing and managing such cases—primarily because standard therapy approaches designed originally either for treating asthma or mentored towards combating COPD don't fully address overlapping features exhibited by those diagnosed with this condition.
While we've made significant strides in understanding how two generally separate entities previously thought to occupy different spaces in the lung diseases spectrum could converge toward familiar crossroads, further research is needed to understand underlying biological mechanisms driving this coexistence scenario fully so newer treatment strategies might be developed targeting specifically those straddling intersection between asthma and COPD.
How does Asthma-COPD Overlap coexist?
While Asthma and COPD are traditionally seen as separate conditions due to their particular symptom manifestation and disease mechanisms, in reality, there are many instances where the lines get blurred, leading toward coexistence form.
Asthma is generally diagnosed in childhood following episodic symptoms such as wheezing and shortness of breath, often linked with allergic reactions or triggered by specific irritants. It responds well to bronchodilators, signifying a largely reversible airway obstruction pattern where periods of symptom flare-ups subside towards near-normal breathing intervals before the next episode kicks off.
On the other hand, COPD primarily affects adults over 40 years, predominantly presenting a history of prolonged exposure to smoking – the principal driving agent causing irreversible lung tissue damage, leading to a progressively worsened persistent state of obstructed airways, unlike periodic relief observed across asthmatic cases.
So when we refer to overlap between these two conditions—ACO—we imply a combined feature set observed simultaneously within the same patient: chronic airflow limitations (a marker for COPD), interspersed episodes of acute worsening respiratory status exhibited on top baseline dyspnea characterising Asthma flares.
Medical expert consensus has acknowledged this overlap syndrome primarily stems from chronic inflammation culminating in both bronchial hyperactivity, also called 'airway remodelling characteristic of asthma, along with progressive airway damage, which predominantly features consistent with persistent exposure to harmful agents like tobacco smoke leading towards COPD pathway eventually hence presenting shared inflammatory response attributed by immune system priming causing irreversible structural changes impacting normal respiratory functioning accordingly thus giving rise unified yet contrary clinical picture at times perplexing diagnosis process initially surrounding such cases.
Studies have shed light on various genetic and environmental factors shaping the susceptibility risk of developing ACO among the population. For instance, the crucial role Th2 cell-mediated cytokines interleukin (IL)-4 IL-13 plays contributes to eosinophilic inflammation linked to asthmatic features. At the same time, neutrophilic infiltration akin to emphysematous change hallmark possible via cellular responses triggered oxidative stress factor commonly associated with underlining COPD progression among individuals has been documented. So, it's plausible for asthma and COPD markers to be expressed dually under certain physiological circumstances, causing overlapping phenomena.
However, understanding exactly how these divergent pathways converge within a single individual is still the subject of ongoing investigations globally aimed at decoding mysteries surrounding this intriguing overlap syndrome, unravelling its root cause and unveiling therapeutic targets, thus paving the way for potential cure possibilities, perhaps in future leading towards breath freedom eventuality.
Existing evidence supporting 'overlap' arrived only recently when clinicians started identifying patients who didn't fit neatly into traditional diagnostic categories, either representing 'pure' asthma or typical instances showcasing COPD. The evidence from several large-scale epidemiological studies suggests that a considerable number of patients exhibited features of both conditions.
A compelling study titled "Asthma and COPD Overlap in Women", published in the journal Annals of Allergy, Asthma & Immunology revealed that nearly 50% of women having persistent asthma might develop symptoms indicative of chronic obstructive diseases later on in their lives if they continue smoking besides having this pre-existing asthmatic condition.
Additionally, these hybrid presentations have been observed more frequently amongst adults with long-standing asthma than the younger version population, where 'purity' one-sided ailment often prevails over mixed manifestations. This noted shift has raised interest within medical research communities in further investigating actual biological mechanisms driving such converging trends; for instance - could it be due to constant exposure irritants leading progressive transformation episodic reversible blockage towards irreversible damage lung tissues as seen under typical cases denoting COPD?
Supporting this hypothesis are results of another groundbreaking investigation – A Swedish cohort study disclosed data supporting the inference of how long-term severe asthma can eventually lead to fixed airflow obstruction, implying a potential evolution pattern rendering Asthmatics susceptible to developing combination airway syndromes dominated primarily by hallmark elements worsened respiratory functionality across overlapping scenarios represented between traditionally separate domains envisaged historically regarding Asthma and COPD. This study, published in The Journal of Allergy & Clinical Immunology: In Practice, followed patients over time to show that their airway remodelling essentially happened due to underlying asthmatic inflammation worsened with repeated exposure to noxious particles or gases; this persistent irritation might lead a shift towards 'hardening' lung tissue mimicking patterns observed within conventional chronic obstructive pulmonary disease.
It is worth mentioning another piece of evidence from the PLATINO Study, which found that around 12% - 13% of adults aged above 40 years living across Latin America represented mixed characteristics hours following inhalation of bronchodilators, lending credence toward the existence of such overlapping disorders primarily succeeding advanced age besides prevalent smoking habits shared commonly reported cases discussing origins these prevailing respiratory issues.
At the molecular level, there's growing recognition that genetics can also play a role in defining predisposition developing Asthma-COPD Overlap. A groundbreaking research presented at the European Respiratory Society's annual congress (2016) hinted that a variant gene named MMP-12 could increase susceptibility among individuals experiencing harsh combination symptoms imitating distinct aspects of both separately classified ailments uniting somehow into a unique entity-Asthma-COPD overlap, thereby suggesting probable hereditary links contributing.
ACO's complexity underscores a critical need for continued research - ranging from population-based studies to more intimate examinations of genetic influence and cellular behaviour within the lungs, all directed towards understanding this nuanced phenomenon better. As healthcare professionals, recognising its existence is the first step toward improved diagnosis while understanding underlying dynamics in clinical scenarios funnels down refining management strategies, hence shaping crucial aspects of patient care, rationalising individualised treatment plans focused on attenuating symptom burden improvise overall life quality those navigating waters marked by overlapping symptoms amid two most prevalent airway diseases.
Thus, confirmed presence, along with growing recognition of Asthma-COPD Overlap (ACO) at the intersection of the global respiratory landscape, signals a new era where responsibilities multiply, not merely compartmentalising these disorders' traditional standalone categories instead looking beyond such simplistic interpretations, embracing advanced scientific insights providing comprehensive outlook addressing challenging status-quo further building knowledge base benefit generations diagnosed with mixed manifestations complicating clear-cut diagnostic pathways.
How does Asthma-COPD Overlap differ from other types of Asthma?
Differentiating asthma-COPD overlap from other types of asthma is crucial for an accurate diagnosis and developing effective treatment strategies.
Asthma presents itself in several forms, such as allergic asthma, non-allergic asthma, adult-onset asthma, or exercise-induced bronchoconstriction, to name a few. Each variant carries its unique set of triggers inducing symptom onset besides following distinct progression patterns while sharing common ground around the existence of inflammation-caused airway obstruction, which stays largely reversible.
ACO's divergence begins at this very juncture, where typical asthmatic cases witness bouts of breathing difficulty interspersed by periods of relief. Patients diagnosed with Asthma -COPD overlap endure persisting airflow limitations mimicking behaviour observed under chronic obstructive pulmonary disease scenarios. In essence, it demonstrates mixed attributes combining critical aspects of both separately classified ailments into a shared platform, leading to worse health impairments than individuals experiencing specific types of 'pure' asthma.
A large-scale study published in the Journal of Allergy & Clinical Immunology explored differences among these subsets, grouping them primarily basis age-onset severity levels across participants. The researchers found that subjects with late adulthood asthma showed a more pronounced deficit in their lung functions coupled with higher exacerbation rates plus extended healthcare utilisation, lending credibility to hypotheses suggesting transformation patterns representing a progressive shift from classic asthma towards a more persistent type of airway obstruction dominant feature COPD - thereby putting the spotlight on this very existence of ACO.
Another intriguing aspect of differentiating asthma-COPD overlap from other types of asthma resides within the response factor. Traditional Asthma cases usually respond favourably to initial bronchodilator treatment exhibited through increased lung function post-administration. At the same time, in scenarios like ACO, such responses become blunted, indicating decreased reversibility airflow limitation linking closer towards principle attributes of chronic obstructive pulmonary diseases, especially prominent among those with long-term smoking history.
Research presented by the European Respiratory Journal evidenced that patients identified with 'overlap' displayed diminished responses to classic steroid treatments compared to those diagnosed exclusively with the typical kind, possibly hinting at pharmacological resistance common amongst overlap instances. This professional knowledge advises clinicians towards individualising management plans potentially involving combined use of inhaled corticosteroids alongside long-acting beta2-adrenoceptor agonists, even extending newer strategies like using phosphodiesterase type 4 inhibitors specifically allowing improved control symptoms across particular population groups.
It is also worth noting that patients representing features of both disorders have faced frequent exacerbations besides higher hospitalisation rates than their counterparts diagnosed only with either condition. This was confirmed by a Japanese study published in Respiratory Investigation, which denoted poorer health outcomes, including significant mortality risks associated specifically amongst overlap instances versus isolated occurrences, conventional terms visualizing demarcation lines separating boundaries around previously known categories.
Lastly, beyond the clinical symptoms and treatment response diversity posing challenges to healthcare providers are factors like quality of life (QoL) deterioration seen widely among patients battling this overlap. Due to recurrent exacerbations contributing significantly towards increased morbidity, it's not uncommon to encounter severe decline QoL indices amongst diagnosed groups throwing light complexity predicament dealing with combination syndrome as opposed to discrete disease forms individually presenting either typical asthmatic episodes or featuring classic COPD manifestations.
Epidemiological study revealed in Respiratory Medicine highlighted considerable negative impact on everyday living conditions ensuing such overlaps effect much more profound compared standard asthma cases, underlining distinct difficulties associated with managing ACO. These insights highlight the critical need to develop novel targeted approaches to improve health-related outcomes, specifically patient population marred overlapping respiratory ailments, enlarging the scope of available intervention strategies.
In summary, the different asthma types have similar features with reversible airway blockage mainly due to inflammation. However, a key difference arises when these traits become less responsive to traditional treatments, commonly seen in chronic obstructive pulmonary disease (COPD). This phenomenon is now recognized as 'Asthma-COPD Overlap' (ACO), distinguishing itself from other asthma types by combining aspects of both asthma and COPD in its clinical presentation within obstructive lung diseases.
In-depth understanding and knowledge about these differences enable healthcare providers to better tailor diagnostic processes and therapeutic strategies into individualised care plans. By recognizing this convergence space between Asthma & COPD, its unique challenges, as well as crucial differences compared with traditional singular presentations, we can pave the way for more effective patient-centred treatments, providing feasible options maintainably combating worsened health status frequently associated among those experiencing difficulties navigating intricacies born around diagnosis: Asthma-COPD overlap (ACO).
Is Asthma-COPD Overlap a Severe Type of Asthma?
No, it's essential to understand that Asthma-COPD overlap (ACO) is not technically classified as a severe type of asthma'; instead, this term represents a unique clinical entity comprised of distinct features drawn from both asthmatic and COPD conditions exhibiting simultaneous components marking characteristic chronic lung disorder territory in its unified manner.
Asthma can be categorized by severity: intermittent, mild persistent, moderate persistent, and severe persistent. Here, the classifications are based primarily upon frequency symptom occurrence daytime-nighttime along functionality limitation degree where intermittent considered least severe while moving towards most end spectrum eventually with distinctive management protocol aligned each division accordingly.
In contrast, ACO combines physiological traits reflective of obstructive pulmonary disease caused by continuous exposure to harmful particles-gases leading to gradually progressive breathing troubles with reoccurring wheezing- shortness of breath representing allergic airway inflammation-related triggers seen joint within asthmatic individuals, therefore making them uniquely entangled web symptoms causing complexity around their diagnosis-treatment procedures rather than being merely extended version sickened state' falling under pre-conceived conventional 'mild-to-severe' categorizations upheld universally describing standalone asthma condition essentially hence necessitates need identification novel strategies handling these complicated cases employing patient-specific considerations predominantly.
Within ACO, there's indeed the presence of severe airway inflammation, which may resemble severe asthma. However, the contributing environmental and lifestyle components often lean towards COPD influences such as long-term smoking or occupational hazards that lead to eventual emphysema-chronic bronchitis types, suggesting probable dual-pathways interaction resulting in this phenomenon occurrence, thereby resisting categorization under isolated singular disorder.
Research from various cohorts suggests that patients with overlapping characteristics experience worse health outcomes than those suffering exclusively from COPD or asthma. Individuals presenting features typical for both conditions are generally associated with increased symptom severity, frequent exacerbations, hospitalizations, poor quality of life, and faster decline in lung function - all hallmarks indicating heightened disease severity compared to solely asthmatic counterparts. One study published in the International Journal of Respiratory Medicine revealed approximately 27% of patients diagnosed with coexisting manifested significantly greater airflow obstruction contrasted against standalone ailments
To sum up, despite prominent increased complications associated with the overlap of asthma and COPD, characterizing it as a severe form of asthma is not universally accepted. This discrepancy in opinions stems from several elements, including variations in clinical presentations, research methodologies used for diagnosis, lack of standard diagnostic criteria, and individual patient histories differing vastly, along with many other factors.
What are the Common Symptoms of Asthma-COPD Overlap?
Individuals with asthma-COPD overlap often exhibit a combination of symptoms traditionally associated with both conditions. While these signs can vary among patients based on severity and frequency, several commonly reported symptoms highlight this condition:
- Shortness of breath: Also known as dyspnea, it refers to difficulty or discomfort while breathing. It is often more severe in the mornings and frequently occurs during physical activity
- Wheezing: A high-pitched whistling sound when you breathe out—it's caused by narrowed or compressed airways, which results from inflammation in both asthma and COPD.
- Chest tightness: Many individuals experience feelings akin to pressure or squeezing within their chest region—an uncomfortable sensation typically resulting from spasms within bronchial tubes due to irritated surrounding lung tissue.
- Breathing Distress: This is a common manifestation in ACO, referring to discomfort experienced either at rest or during strenuous activities. It often worsens under unfavourable weather conditions like those in cold seasons.
- Feeling winded: A sense of fatigue or exhaustion makes it tough to catch one's breath, even after minor physical exertion.
- Excessive mucus production: Both conditions can stimulate the overproduction of mucus in the lungs, leading to congestion and frequent urges to clear the throat, making breathing more difficult with constricted airways resulting from an accumulation of this sticky substance produced excessively as the body's immune response trying to protect against inflammatory triggers prevalent under both disease spectrums.
- Recurring Coughing: Chronic cough, which tends to be dry within asthmatic individuals while producing phlegm COPD patients, often becomes a common symptom combination therein seeing a distinct shift towards productive nature over suggesting likely overlap existence midst usually persistently being present its form symptomatic feature giving rise relentless discomfort alongside interfering daily activities regularly indicating students severity may require immediate medical attention for relief.
- Inadequate Physical Capacity for Exercise: Inactivity or exercise intolerance where performing routine tasks or engaging in moderate exercises like walking becomes strenuous due to constant breathlessness disrupting normal functioning, adversely affecting a person's quality of life, significantly causing social isolation and psychological distress, hinting progressive lung damage having settled into system heartening comprehensive diagnosis intervention at earliest convenience thereby avoiding further health adversity potentiality standing eventually.
What Causes Asthma-COPD Overlap?
Defining the exact causes of asthma-COPD overlap (ACO) can be complex since ACO isn't just a single disease but rather represents coexisting features of both conditions in an individual. However, several common triggers and risk factors have been identified through research that contribute to its development.
The foremost factor is tobacco smoking, which has long been recognized as the primary cause of COPD while also worsening asthmatic symptoms significantly - hence increasing the likelihood of overlaps. It's estimated that 40% or more people diagnosed with ACO have had a history of heavy smoking; this proportion goes up substantially when considering elderly populations where cumulative exposure rates tend to be higher.
Exposure to indoor and outdoor air pollutants like dust mites, vehicle emissions along animal dander, etc., exacerbate existing respiratory issues and potentially precipitate onset combined. Interestingly, research increasingly links environmental pollution, particularly fine particulate matter PM2 developing alone.
Moreover, individuals' prolonged occupational exposure to certain chemicals, irritants, coal mine gas fumes, and agricultural sprays heightened risk. These toxins, upon inhalation, induce chronic inflammatory responses in the lungs, causing bronchial epithelial damage to snowball into full-fledged. Lastly, genetic predisposition plays a definite role. Twin studies show even identical twins raised in different environments share liability. Suggesting inheritable component
Respiratory infections during early childhood also significantly increase the likelihood of developing ACO. This link has primarily been attributed to lung damage occurring in a developmental stage, resulting in long-term impairment or heightened vulnerability towards respiratory diseases later in life.
Further research is being done on how ageing affects this overlap as older adults manifest mixed features more often than younger counterparts. This suggests that the natural age-related decline in lung function (senile emphysema) might be an unaccounted contributor driving partial overlaps. This 'ageing-lung' hypothesis postulates that just like other organs, our lungs, too, have a predetermined functioning span beyond which they gradually lose efficiency and start exhibiting symptoms akin to COPD-asthma irrespective of external factors alone.
Comorbidity with certain conditions, such as bronchiectasis, could also predispose individuals to develop both asthma and COPD concurrently because these disorders share several physiological dysfunctions, including increased airway inflammation susceptibility and recurrent respiratory infections.
However, while we know many risk triggers contribute to the expression, the scientific community conclusively identifying precise mechanisms leading to coexistence pathways involved remains largely elusive. Hence, ongoing focus on understanding better managing and preventing its consequences
In conclusion, despite knowing key contributors causing myriad complex interplaying variables render individuals susceptible, it necessitates personalized approach diagnosis treatment rather than a one-size-fits-all strategy.
It is also important to point out that the causes of ACO are not necessarily independent from each other - they interact in ways which could potentially amplify an individual's susceptibility to developing overlapping symptoms. For instance, a smoker working in high-exposure occupations or living in polluted regions might experience compounding effects, hastening the deterioration of lung health.
In cases like these, comprehensive profiling involving thorough medical histories coupled with continuous monitoring of environmental exposures becomes crucial for early detection and preventative measures against progression towards overlap syndrome. Specific lifestyle changes such as quitting smoking, maintaining a healthy body weight, and exercising regularly have been proven effective in mitigating risks associated with both diseases independently, thus demonstrating potential benefiting people showing asthmatic-COPD features.
Moreover, understanding a patient's genetic makeup opens the door to precision medicine therapies tailored to unique biological disease manifestations. This makes the case for whole-genome sequencing studying identified gene variants strongly implicated in asthma COPD inception.
As can be seen, there isn't a single factor responsible for triggering; instead, multiple interrelated factors contribute to developing a complex picture. We continue to unveil better equipment to manage and reduce the burden patients suffer from this debilitating condition worldwide. Hence, ongoing biomedical research fields in epidemiology, pulmonology, and genetics hold key unlocking mysteries surrounding collusion underlying pathogenesis management interventions unusually challenging respiratory disorders such as overlap.
What are the Risk Factors for Asthma-COPD Overlap?
Certain risk factors increase susceptibility towards developing asthma-COPD overlap. Here's a look at crucial contributors pushing an individual's scale toward this unique syndrome:
- Tobacco Smoke: Both active and passive smoking are significant risk factors. The harmful substances in tobacco smoke can trigger asthmatic reactions, while long-term exposure damages air sacs, leading to emphysema–a COPD condition.
- Air Pollution: Chronic exposure to indoor and outdoor pollutants can induce asthma and COPD symptoms by irritating the respiratory system and causing an inflammatory response, thus laying the groundwork for potential ACO evolution.
- Occupational Exposure: Certain jobs expose workers to fumes, dust, or chemicals triggering lung damaging changes, making them more susceptible to persistent airflow limitations characteristic under these disorders, hinting likely development into an overlapped state if already existing.
- History of Respiratory Infections: Recurrent infections, especially early childhood, could cause lasting impacts on developing lungs, setting the stage for chronic Airways disease establishment later potentially escalating convergence phase unchecked promptly well managed throughout course time certainly highlighting the necessity of effective preventive measures place safeguarding health priorities first above all-where every breath counts definitely!
- Age and Gender: The onset of ACO is often noticed in adults over 40, and it's slightly more common in women than men. Ageing causes changes to lung structures while hormonal shifts seen among females could impact immune responses, contributing mix factors adding susceptibility risk accumulation henceforth.
- Uncontrolled Asthma: If asthma isn't well-managed throughout its course since childhood, it may gradually develop irreversible airflow obstruction, marking progression from merely asthmatic characteristics toward which resembles COPD nature too, thereby indicating overlap tendency later stages of adulthood, particularly sparking need-focused comprehensive care promptly ensuring optimal disease outcomes further down line life trajectory tracing eventualities closely associated varied lung-health states uniquely intermingling them.
- Comorbidities: Certain underlying diseases like allergy, obesity, and chronic rhinosinusitis are found to be linked with ACO indication, thereby suggesting closer look into these conditions might provide clues to understanding the aetiology behind asthma-COPD overlap manifestation progressively increasing risk confronting such dual-disorder existenc
These factors play a pivotal role in the development of Asthma-COPD Overlap; Noting these specific risks might help clinicians better strategize preventive measures while guiding a person's management plan, ensuring improved health outcomes throughout life, even when faced with chronic conditions like ACO.
How is Asthma-COPD Overlap Diagnosed?
Diagnosing asthma-COPD overlap (ACO) can be particularly challenging due to the co-existence of features typical for both diseases in a single patient. However, there are several clinical presentations and testing strategies that physicians rely upon for identifying ACOs.
Firstly, it's essential to understand that diagnosis involves an inclusive assessment of medical history, including onset age symptoms, severity frequency, exacerbations, known allergies, comorbidities, etc. In many cases, individuals experiencing greater than expected variability airflow limitation or those showing evidence of airway hyperresponsiveness while also having persistent non-fully reversible obstruction indicate overlapping.
Spirometry is an essential tool used in diagnosing respiratory conditions like these. This test measures how much air you can breathe out (forced expiratory volume 1 second, FEV1) and quickly do so (forced vital capacity FVC). Patients suspected have usually displayed a post-bronchodilator ratio of less than %, indicating COPD and abnormally high reversibility after administration -- pointer suggesting asthmatic participation.
Other relevant tests include serum eosinophil counts measuring fraction exhaled nitric oxide FeNO levels, which are markers of inflammation and often elevated people. Additionally, chest X-rays and computed tomography scans help identify any structural abnormalities within the lungs, such as emphysema or bronchiectasis, that are more common in COPD while ruling out other potential causes of patient symptoms.
Furthermore, a detailed examination might also involve allergy skin testing. This is done to detect any allergic responses towards specific triggers like dust mites, pollen, etc., which provides further evidence pointing towards asthmatic tendencies since they're hardly ever seen amongst standalone COPD cases.
However, one challenge in diagnosing lies in the absence of internationally accepted criteria to classify conditions, causing variations in the interpretations of different healthcare providers. Consequently, the approach primarily involves clinical judgment based on various diagnostic information rather than a single definitive test tool.
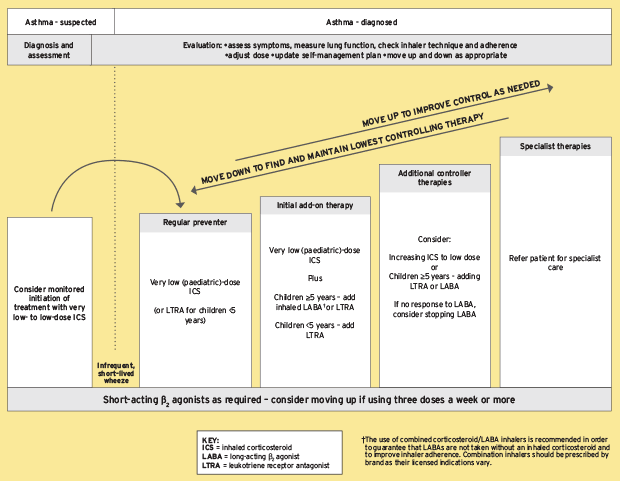
Despite these difficulties, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Asthma Management Strategy (GINA), two leading global coalitions of respiratory medicine, provided guidelines to identify Key features, including age onset, history of smoking variability, lung function tests, among others. These rely heavily on the patient's medical history, and presentations can confirm diagnosis.
Nevertheless, the research develops a thorough, comprehensive understanding of overlapping characteristics and hopes to better guide physicians in accurately diagnosing and managing conditions accordingly. Additionally, the workers' field advocates the development of uniform, official, universally recognised help streamline classification treatment strategies in the future.
In conclusion, ACO is diagnosed carefully through patient interviews, physical examinations, and several vital instrumental insights. However, a precise standardised definition still needs to be discovered, and current methods provide an approximation rather than concrete assurance, making timely accuracy crucially dependent on a doctor's experience and clinical acumen. Thus, continuous research is essential to bridge the gap between existing diagnostic methods and a universally accepted guideline specific to ACO for early detection, effective treatment planning, and overall better patient prognosis.
In the meantime, educating patients about both their similarities and differences will aid in self-monitoring disease progression and promote adherence to prescribed interventions. As we continue to uncover complexities associated with diagnosing overlap syndrome, it remains imperative to strive for rigorous yet accessible approaches to analyse reducing lingering uncertainty surrounding this unique confluence of diseases, ensuring appropriate care management for those affected by Asthma-COPD Overlap.
What Tests are Used to Diagnose Asthma-COPD Overlap?
The following tests are used to diagnose Asthma-COPD Overlap:
- Spirometry: This test measures the amount (volume) and speed (flow) of air that can be inhaled and exhaled, primarily checking for signs of airflow limitation or obstruction commonly seen in asthma and COPD. In an ACO context, spirometry results typically exhibit a post-bronchodilator FEV1/FVC ratio of less than 70%, suggesting COPD and a significant response to bronchodilators indicating asthmatic traits.
- Chest Imaging: Chest X-rays or CT scans assist doctors by providing detailed images of lung structure, helping them rule out other respiratory diseases while detecting conditions like emphysema, often linked to patients dealing
- Fractional Exhaled Nitric Oxide Test(FeNO): Elevated levels of nitric oxide exhalation indicate inflammation of airways typical for those suffering from allergic asthma and thus serve helpful diagnostic pointers when identifying overlap patterns
- Allergy skin tests- Often employed to detect sensitivities towards common allergens such as dust mites, pollen, etc. If positive, these suggest proclivity. Practitioners might take results in supportive evidence pointing to concurrent manifestations
- Blood Eosinophil counts: A high blood eosinophil (a type of white blood cell) count is associated with asthma or severe COPD, hence its utility in detecting overlap. Elevation could indicate an immune response suggestive of asthmatic tendencies, while these cells in sputum can depict a picture similar to that seen during COPD exacerbations.
- Bronchodilator Responsiveness Testing– This involves administering a bronchodilator drug and subsequently retesting spirometry to evaluate the patient's responsiveness. An increase of 12% and at least 200 mL in FEV1 (Forced Expiratory Volume - it's a measure of how much air you can exhale with force in one second) post-bronchodilator use is generally suggestive as per global guidelines marking improved ventilation response pattern commonly associated with asthmatic conditions.
In cases exhibiting stable COPD, patients often show less significant improvement following bronchodilation. While calculating a fixed ratio where FEV1/FVC value being <=70% indicates the presence of persistent obstruction
- Methacholine Challenge test- In this procedure, patients inhale increasing amounts of methacholine aerosol mist before, which indicates any hyperreactivity in the airway common among asthmatics. If they react to low concentration, said to have "bronchial challenges," it helps detect subtle forms of mixed features that might not picked up in regular testing
- Complete Blood Count (CBC): While it doesn't directly contribute towards identifying overlaps, a general health check is often recommended since other conditions, like anaemia, pulmonary embolism, etc., mimic symptoms and thus must be ruled out.
- Pulse oximetry test: Physicians may measure your blood's oxygen level. While this doesn't diagnose ACO directly, it offers valuable information about how well lungs function and can help monitor disease severity or response to treatment over time.
These tests are integral to diagnosing asthma-COPD overlap, providing physicians with insightful data on patients' lung function, structural abnormalities, if any, and their bronchial responsiveness, amongst other vital parameters. Despite the plethora of available diagnostic tools, they remain primarily clinical based on a doctor's comprehensive analysis history symptomatology corroborated findings from various investigations. Remember, early detection leads to effective, timely management; hence, the importance of these cannot overstated.
Are Blood Tests Done to Diagnose Asthma-COPD Overlap?
The short answer is no. A blood test alone cannot definitively diagnose the overlap of asthma and chronic obstructive pulmonary disease (COPD). Diagnosis of these conditions is primarily based on an individual's complete medical history, symptoms, and results from certain diagnostic tests such as spirometry.
Asthma and COPD exhibit differences in underlying causes; hence, asthmatic inflammation differs significantly from COPD inflammation. As a result, no specific marker can be detected through blood tests exclusively for diagnosing ACO (Asthma-COPD Overlap).
Although blood tests may not be the absolute diagnostic method for asthma-COPD overlap, it's important to acknowledge their significance in controlling these conditions. For instance, they can offer critical information about a patient’s overall health and assist in eliminating other potential causes of symptoms.
Elevated counts of eosinophils – white blood cells implicated in allergic responses and inflammation - could indicate the existence of asthma or COPD. Studies have shown that patients with high levels typically exhibit improved response to particular treatments like corticosteroids; this helps minimise airway inflammation, resulting in enhanced lung functionality over time.
Blood testing also plays an integral part when considering coexisting medical conditions common across individuals suffering from either asthma or COPD, including cardiovascular diseases & diabetes, among others. This all-rounder utility offered by simple peripheral venous blood draws weighs favourably on its usage within targeted diagnostic workup plans despite its limited scope concerning confirming ACO conclusively.
As part of regular follow-up care for asthma and COPD alone, physicians commonly conduct blood tests to monitor the effectiveness of therapies. Suppose a patient doesn't respond well enough despite following prescribed medication routines seriously. In that case, it flags signs pointing towards disease overlap features not previously recognised, thus indicating ACO existence specifically when accompanied by persistent symptoms linked with both individual diseases maintained over time.
Notably, while routine blood work might provide beneficial insights into organ performance aspects like liver & kidney functions, lipid profile levels, vitamin deficiencies, etc.- they all add onto essential data points needed during the formulation phase, where personalised action plans are developed based upon each unique clinical presentation scenario.
In summing up, although there's no dedicated 'blood test' that comprehensively diagnoses Asthma-COPD Overlap owing largely towards its multifaceted nature showcasing combined pathological patterns staying true across every distinct case, it shouldn't undermine the immense importance these tests carry overall within a broader perspective concerning diagnostic management besides suggesting potential treatment strategies revolving around complex cardiopulmonary disorders including ACO.
How accurate are the tests for Asthma-COPD Overlap?
Asthma and chronic obstructive pulmonary disease (COPD) overlap, or ACO, is a complex condition that can be difficult to diagnose due to accurate overlapping symptoms. The tests used in diagnosing this condition must possess precision capabilities.
Pulmonary function tests like spirometry play an essential role. However, they cannot definitively distinguish between the two conditions independently. One of the typical approaches includes spotting eosinophilic inflammation often present in asthma patients but not generally seen in pure COPD cases during blood or sputum examination.
The identification of individuals with ACO relies mainly on confirmed, persistent airflow limitation together with a significant history of asthma before 40 years old, as stated by Dr Magnussen from the Pulmonary Research Institute at Lung Clinic Grosshansdorf (Magnussen et al., 2014). The statement implies that diagnosis relies not solely on testing methods' accuracy but on comprehensive patient medical histories.
More recent studies have delved into utilising biomarker discovery strategies for better accuracy. There might still be variation which makes it more difficult than thought to diagnose ACO accurately with single tests or biomarkers, as declared by Dr Sator L Lehtimäki from University Hospital Tampere. (Lehtimäki et al., 2019).
Utilising multiple diagnostic parameters, such as high blood eosinophil counts and a history of asthma, helps differentiate individuals with COPD who have overlapping features as emphasised by Prof. Don D. Sin from the University of British Columbia (Sin et al., 2017). This further amplifies the need for detailed medical histories in conjunction with lab results. Furthermore, Dr Klaus F Rabe from Lung Clinic Grosshansdorf suggested comprehensive testing involving CT-scan imaging, mentioning that "high-resolution computed tomography may contribute to identifying patients showing signs of both inflammations."
In summary, while current diagnostic tools like spirometry and inflammation markers provide insightful data toward an accurate diagnosis, combining these results with clinical examinations remains crucial. The combination offers a more holistic approach to accurately identifying Asthma-COPD Overlap syndrome.
What are the Treatments for Asthma-COPD Overlap?
Treating asthma-COPD overlap (ACO) intricate due to its dual nature. The goal is to manage symptoms associated with both diseases while preventing flare-ups and slowing down progression whenever possible.
- Pharmacological therapy: This forms the cornerstone of managing ACO. In general terms, inhalers are first-line treatment options, including long-acting bronchodilators that reduce obstruction, like tiotropium formoterol or salmeterol. Inhalation corticosteroids (ICS) such as fluticasone mometasone are also commonly prescribed to control inflammation with regular use, which has proven to decrease exacerbations
- Combination Therapy: Often, a combination of medications that include an ICS and one or more bronchodilators is recommended to manage patients optimally. Essentially using a 'triple strategy, ' patients have persistent airflow limitation despite receiving mono-dual therapies
- Pulmonary Rehabilitation: Comprises patient education, psychosocial support, exercise training, and nutritional counselling to improve physical endurance, reduce breathlessness, and enhance the overall quality of life.
- Vaccinations: Regular vaccinations against pneumonia and annual flu shots are advised to protect vulnerable lungs from recurring infections that often trigger acute episodes in susceptible individuals
- Biological therapies: For those with frequent exacerbations despite regular use of recommended treatments, such as monoclonal antibodies targeting specific immune responses can be considered. These include omalizumab (for patients with severe allergic asthma), mepolizumab and benralizumab (both for eosinophilic Phenotype).
- Lifestyle modifications: smoking cessation, maintaining a healthy body weight, and ensuring sufficient physical activity. These play essential roles not only in controlling symptoms but also in slowing down disease progression, thereby improving life expectancy quality
- Self-management plans: Providing individuals with a written plan outlining how to monitor their condition when increasing medication or seeking medical help empowers them to manage symptoms effectively and identify signs of impending exacerbation in the early stages
- Lung volume reduction surgery: Severe unresponsive cases to other traditional interventions might require more drastic measures. Pulmonologists resort to such surgical procedures as lung volume reduction surgery (LVRS), endoscopic valve placement, and even transplantation in extreme instances. However, these are typically the last resorts explored if all else fails.
- Lastly, the evolving field of precision medicine holds promise, offering targeted, individualised, unique genetic, molecular profile biomarkers. This approach is still in the research phase and will potentially revolutionise how we treat these complex diseases in the future.
The above treatments can considerably help manage symptoms and improve the quality of life for most patients. Patient-centred care is essential - individuals need to work closely with their healthcare provider to decide which therapeutic strategy or combination best suits their specific condition.
It's also crucial to note that response to treatment varies significantly amongst different individuals – hence, regular monitoring of disease progression becomes crucial in adjusting treatment plans accordingly. Researchers ongoingly explore newer avenues, including anti-inflammatory drugs targeting particular pathways involved in both diseases separately and conjointly aiming at better control over exacerbations plus enhancing lung functions, thereby slowing down overall rate decay.
With advances in medical science and a growing understanding of underlying pathophysiological processes, we aim to chart effective strategies to properly equip doctors worldwide to tackle this hybrid ailment properly, ultimately improving health outcomes and reducing the burden on those affected by asthma-COPD overlap.
Can Asthma-COPD Overlap be Cured?
No, currently, there is no known cure for asthma-COPD overlap. While this might sound disheartening, it's important to note that proper management can significantly improve the quality of life and slow disease progression.
The main goal in treating ACO is to control symptoms, prevent exacerbations and enhance overall lung function. This includes regular use of prescribed medications such as bronchodilators or corticosteroids, which help manage airway inflammation, thereby mitigating symptomatic distress among patients.
Emphasis on lifestyle modifications such as avoiding exposure to irritants like tobacco smoke, managing body weight, and maintaining physical activity alongside a balanced diet improves patient outcomes, thus facilitating healthier living even under chronic conditions like 'overlap syndrome'. Regular vaccination against flu pneumococcus also reduces the risk of severe infectious complications, potentially worsening existing pulmonary pathologies.
Pulmonary rehabilitation programs emphasising educational sessions aimed at teaching self-management skills, exercise therapy, and psycho-social support are instrumental in providing comprehensive care despite the incurable nature of these diseases.
To sum up, while the current medical landscape does not offer a cure for Asthma-COPD Overlap, it doesn't mean individuals diagnosed with ACO cannot lead fulfilling lives. The central focus lies in managing symptoms effectively, preventing exacerbations, and halting disease progression as far as possible through medication, lifestyle modifications and regular health check-ups.
Prospects look promising with ongoing research aiming towards new treatment breakthroughs that may eventually bring us closer to finding definitive solutions for conditions like 'Overlap Syndrome'. Until then, we continue our stride toward optimal symptom control, ensuring improved longevity and quality of life for those suffering under the combined influence of asthmatic & COPD pathology.




















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews