Non-Allergic Asthma: Causes, Symptoms, Diagnosis, and Treatment


Related products
Non-Allergic Asthma Overview
Asthma, a chronic respiratory condition characterised by episodes of breathlessness and wheezing, is generally associated with an allergic response; however, there exists another type known as Non-Allergic Asthma. Unlike its counterpart, atopic or extrinsic asthma, which results from exposure to allergens like pollen or dust mites, non-allergic asthma occurs without any distinct triggers.
Non-allergic asthma forms part of intrinsic types of asthma, where individuals experience symptoms unrelated to allergies but still exhibit asthmatic conditions. Comprehending the causes and necessitating early diagnosis are important steps toward effective treatment for this specific form of disease.
The primary causes of non-allergic asthma range widely and often include irritants such as smoke (including second-hand tobacco smoke), strong odours from chemicals or perfumes, changes in weather, especially cold air temperature, and even viral infections, particularly those affecting the respiratory system. Stress serves as a significant contributing factor in aggravating attacks among patients suffering from the non-allergic type.
People affected by allergic asthma typically encounter similar symptoms to those experienced with other forms: shortness of breath, chest tightness, or pain, along with bouts of coughing during night-time sleep, making detection difficult due to these overlapping traits among different types.
Diagnosing it involves identifying typical signs through a series of pulmonary function tests. Physicians assess the patient's lung capacity and airway responsiveness through methods such as spirometry, peak flow monitoring, or methacholine challenge test. These procedures are designed to measure different aspects of breathing efficacy, thus aiding in distinguishing non-allergic asthma from other types.
When it comes to treatment options for non-allergic asthma, there is no one-size-fits-all solution given its highly individualised nature; however, medical professionals typically resort to avoiding known triggers while incorporating pharmaceutical interventions that focus on controlling symptoms and preventing episodes rather than curing the condition entirely.
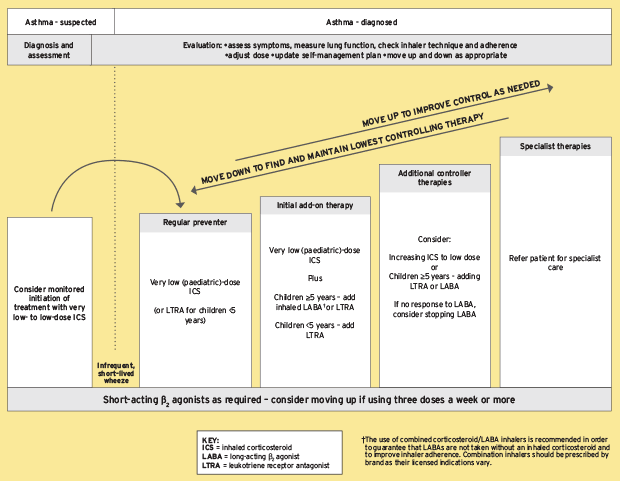
Common medication options include inhaled corticosteroids, which work by reducing inflammation inside airways, thereby making them less sensitive to triggers. An alternative approach involves bronchodilators — either short-acting for immediate relief during an attack or long-acting ones used routinely for prevention purposes — which assist in relaxing muscles encircling the lungs' airways, thereby improving airflow into/out of them.
Patients might be recommended additional treatments according to their specific needs, including leukotriene modifiers (medications disrupting actions/activity within substances causing inflammation) along with biologics - drugs targeting immune system elements leading towards asthmatic responses.
Regular assessments help monitor disease progression while providing patients with means for effectively managing their condition. It is crucial for patients, particularly those with severe non-allergic asthma symptoms, to maintain regular consultations with healthcare professionals.
Further strategies involve occupational therapy and targeted lifestyle changes, such as adopting a healthier diet or incorporating certain exercises that aid in enhancing lung function.
What is Non-Allergic Asthma?
Non-allergic asthma, often referred to as intrinsic asthma, is a type of chronic respiratory disorder that exhibits typical asthmatic symptoms. Unlike the common form of allergic or extrinsic asthma, where exposure to allergens acts as a trigger for an episode, non-allergic asthma occurs independently from any distinct environmental stimuli.
Understanding "what is non-allergic asthma" involves recognising its complex nature. It manifests through similar symptoms observed in other types, like breathlessness and wheezing; nevertheless, these episodes are not associated with usual allergies but are induced by certain factors such as weather changes (like cold air), strong odours emanating from perfumes or chemical substances, etc.
Multiple forms of irritants have been identified as capable of causing attacks amongst patients with this disease - smoke being one prominent example, including second-hand tobacco smoke along with viral infections affecting the respiratory system.
However, it's important to note that pinpointing specific triggers might be challenging, given their contextual sensitivities vary dramatically across individuals. Hence, overarching preventive strategies usually focus on the general avoidance of known causes while ensuring consistent monitoring routines suitable according to each person's unique needs.
Due to the absence of allergy-related elements contributing towards pathogenesis within the intrinsic version of the care plan developed differs significantly compared to their counterpart versions - a combined approach involving lifestyle alterations alongside medications is adopted geared at managing rather than curing the condition. The core treatment method resides in the use of anti-inflammatory medicines, mainly corticosteroids, which help to reduce inflammation within the bronchial tubes, hence alleviating symptoms and suppressing episodes.
Bronchodilators serve as another common form of medication used regularly for prevention or in moments of severe attacks. They act by relaxing muscles surrounding airways, thereby ameliorating airflow into and out of the lungs and facilitating easier breathing.
Given its intricate nature comprising numerous triggers along with shared symptomatology among other types– diagnosing non-allergic asthma emerges as a challenging task that necessitates a series of tests helping medical professionals identify typical signs indicative of this specific kind while excluding possibilities of any allergic component playing a role in disease manifestation.
Knowing what intrinsic asthma is important entails grasping how regular check-ups are key to monitoring progress - particularly crucial for those experiencing heightened severity of their asthmatic symptoms. Exercising caution regarding influencing factors, lifestyle, and dietary habits, amongst others, allows for forging effective management plans mitigating the impact of potential bouts of breathlessness associated with them, ultimately leading to enhanced quality of life for patients suffering from a less recognised yet equally impactful version of chronic respiratory disorders known as non-allergic asthma.
What is another term for Non-Allergic Asthma?
Non-allergic asthma is often referred to by another term – Intrinsic Asthma. Unlike atopic or extrinsic asthma, which is triggered in response to specific allergens like dust mites or pollen, intrinsic asthma does not have a clear connection with allergies.
In the realm of medical science and research studies focused on different types of asthma, findings continually reinforce that intrinsic asthma manifests independently from an external allergic reaction. Instead, it gets instigated primarily through non-allergic triggers such as cold air temperature changes, smoke inhalation, including second-hand tobacco smoke exposure along with respiratory infections.
Furthermore, emotional stress has been connected within this context - acting significantly towards precipitating episodes among individuals affected by the non-allergic (intrinsic) type of this disease.
Thus, broadly speaking about these terms, if one refers to "atopic" or "extrinsic", it implies allergy-triggered asthmatic conditions, whereas the mention of "non- allergic" or indeed its more commonly used counterpart "intrinsic" indicates a form devoid of any direct relation with known allergenic factors but still presenting significant symptoms characteristic for all cases pertaining to overall clinical picture diagnosed as 'asthma'.
How many people have Non-Allergic Asthma?
As it pertains to non-allergic asthma, acquiring precise prevalence ratios remains a challenge due to its significant overlap with other types of the disease. According to one study conducted by the Global Initiative for Asthma (GINA), around 300 million people worldwide are affected by some form of asthma – out of which approximately 10-33% suffer from a non-allergic variant.
When considering adult populations specifically, the American Academy of Allergy Asthma & Immunology reported that nearly half (around 50%) of all adult asthma cases do not stem from allergies, implying their potential categorisation as 'non-allergic' subjects.
Children seem less likely than adults in terms of encountering this condition, although definite figures remain elusive; however, estimates suggest that only one-third or fewer paediatric patients exhibit symptoms aligning with the characteristics typical towards non-allergic forms--a figure considerably lesser compared against statistics amongst older age groups suggesting an intriguing trend associated with developing susceptibility over time and implicating factors beyond simple allergen exposure at play here.
Nevertheless, these figures warrant further scientific exploration while reinforcing the need for tailored diagnostic approaches aimed at differentiating between allergy-induced versus intrinsic varieties, thereby facilitating effective treatment strategies based on the underlying cause rather than symptomatic presentation alone.
How does Non-Allergic Asthma differ from other types of asthma?
Non-allergic asthma significantly differs from other types of asthma primarily due to its triggers or the lack thereof. While allergic, or atopic, and other forms of extrinsic asthma are triggered by allergens such as dust mites, pet dander, pollen, or mould spores (American Academy of Allergy Asthma & Immunology), non-allergic asthmatics experience attacks without exposure to these common stimuli.
Instead, individuals with non-allergic asthma experience symptoms often in response to various environmental factors, including cold air temperatures, exposure to smoke and strong odours like perfumes, stress/emotion-induced changes within their bodies; even viral infections affecting the respiratory system leads to the onset of an attack (National Heart Lung Blood Institute).
The exact cause behind disease progression remains uncertain, yet researchers believe it involves inflammation responses that might not necessarily be allergy-driven(American Journal Of Respiratory Critical Care Medicine).
Symptomatically differences emerge between both categories: despite sharing generic symptoms like coughing, shortness of breath, chest tightness/pain, and nocturnal disturbances during sleep, patients with non-asthma exhibit stable periods interrupted by severe episodes, whereas those suffering from allergies have frequent flare-ups resulting in continual daily life disruption(Mayo Clinic).
Diagnostically, bronchial provocation tests play a key role in detecting intrinsic(non-allergic) form and often include methods such as spirometry, peak flow monitoring, or the methacholine challenge test. While these tests are utilised for other types of asthma as well, they become particularly important in diagnosing non-allergic asthma since common allergy testing procedures do not show a clear cause (American Lung Association).
With respect to treatment, both allergic and non-allergic asthmatics benefit from avoiding known triggers and taking prescribed medications that aim primarily at controlling symptoms rather than providing an outright cure. However, some key differences arise here, too - while treatments generally focus on reducing inflammation within airways for those with allergic type, individuals suffering from the intrinsic variety might additionally require targeted therapies aimed specifically towards their unique trigger-less nature (Asthma UK).

What causes Non-Allergic Asthma?
Non-allergic asthma is often caused by anxiety, smoke, stress, fragrances, vigorous exercise, dry and cold air, respiratory viruses and infections and fumes and chemicals.
1. Anxiety
Anxiety, commonly defined as an emotional state characterised by feelings of apprehension and worry often accompanied by physical symptoms such as palpitations or sweating, presents itself in various forms, including Generalised Anxiety Disorder (GAD) and panic Disorders, among others. One notable fact is that chronic anxiety disorders involve a prolonged duration wherein individuals suffer from intense episodes lasting six months or longer.
Emerging research suggests strong links between anxiety and non-allergic asthma, namely that heightened levels of stress resulting in anxiety might act as triggers leading to asthmatic attacks in those suffering from the intrinsic form of the disease. A study published within Psychosomatic Medicine found correlations between patients with higher trait anxiety scores experiencing more frequent severe exacerbations despite having controlled their exposure towards common known allergens, thus reinforcing the idea about the role played by psychological factors as contributors towards worsening this specific type of asthma.
While the mechanism behind the exact cause-effect relationship remains under continued exploration, current theories suggest when the body experiences stress, and it releases certain chemicals that tighten muscle bands around airways - a condition referred to as bronchoconstriction - thereby inducing situations similar to asthmatic episodes(Respiratory Research). Treatment options need to address physiological needs and incorporate strategies aiding sufferers to manage underlying mental health conditions. Hence, they effectively control all aspects related to their unique manifestation of asthma.
2. Smoke
Smoke, by definition, is a collection of airborne solid and liquid particles along with gases emitted during the combustion process or burning. It contains an array of harmful substances, including but not limited to carbon monoxide, volatile organic compounds (VOCs), heavy metals, and fine particles, which causes significant harm, especially when inhaled into the lungs.
Among key concerns associated with smoke exposure is its potential trigger role within non-allergic asthma attacks. The irritating qualities present within smoke often lead to inflammation responses inside airways among susceptible individuals, thus causing symptoms typically seen among asthmatic patients like wheezing tightness, chest shortness of breath, and even bouts of coughing, particularly during sleep time(National Heart Lung Blood Institute).
There isn't any clear consensus yet on the precise mechanism behind how exactly these symptoms develop; however, researchers propose that it might be related to irritation caused by inhaling noxious components found within different types of smoke - whether from cigarettes, wood fires, industrial emissions or otherwise(Center Disease Control Prevention).
One study revealed, for instance, that high levels of second-hand tobacco smoking result in an increased risk of developing severe forms of intrinsic(non-allergic) form, thereby suggesting a direct relationship between two factors (American Journal Respiratory Critical Care Medicine).
While additional research required further establishing exact causal linkages, ample evidence suggests minimising avoiding altogether whenever feasible serves as an effective preventative measure against non-allergic asthma exacerbations. Indeed, smoke-free environments contribute significantly towards improved respiratory health since exposure reduction equates with decreased inflammation inside the lungs (World Health Organization).
Medical professionals often advise individuals already diagnosed with any type of asthma to avoid instances of potential smoke inhalation as it remains a common irritant that easily triggers an episode.
3. Stress
Stress — a natural physical and mental response to life experiences, both positive and negative — occurs when the body responds as if under attack and prepares for protective counteractions. Despite its crucial role in preparing humans to face challenges or escape dangerous situations, persistent stress is linked with various health conditions, including contributing to non-allergic asthma.
Prolonged periods of distress lead to an overstimulated immune system, which then trigger inflammation - one source suggests that such sustained inflammatory responses act upon airways, consequently causing asthmatic symptoms (Journal Of Allergy Clinical Immunology).
Understanding how stress affects asthma becomes particularly pertinent given this connection. Stress triggers the production of hormones like cortisol that usually work by reducing inflammation; however, bodies enduring chronic levels become less sensitive, resulting in reduced efficacy of these anti-inflammatory effects, leading to aggravated asthmatic conditions(National Institute Mental Health).
Furthermore, emotional anxiety-related stress induces physiological changes within respiratory patterns, causing hyperventilation, whereby individuals take rapid, shallow breaths instead of deeper, slower ones necessary, keeping lung passages open and thus exacerbating any pre-existing breathing difficulties(American Psychological Association).
In terms of managing coping strategies, including adopting relaxation techniques, e.g., deep-breathing exercises, yoga, etc., along with seeking professional help to maintain mental well-being alongside medical treatment(Anxiety Depression Association America).
4. Fragrances
Fragrances, defined as a complex combination of natural and/or synthetic substances that contribute to the olfactory characteristics of consumer products (National Institute Of Environmental Health Sciences), often contain volatile organic compounds that easily evaporate at room temperature. Smelling pleasant might seem harmless, yet research indicates fragrances are among the leading environmental triggers for individuals suffering from non-allergic asthma.
Inhaled fragrance molecules, whether via perfumes or scented household items - candles, air fresheners, etc., represent significant irritants potentially provoking respiratory symptoms such as coughing, wheezing, and shortness of breath in persons diagnosed with intrinsic(non-allergic) form. A report published by the Environmental Protection Agency highlights how some commonly used fragrance ingredients cause irritation and demonstrate potential toxicity, harming the lungs' delicate tissues over time.
Accordingly, several studies were conducted exploring the connection between exposure to these aromatic particles & and the progression of symptom severity amongst asthmatics; one visible correlation being evident within the study featured Journal Allergy Clinical Immunology demonstrating a 34% increase in attacks following intensified contact with odorous products.
Treatment strategies predominantly revolve around avoiding known triggers; hence, minimising the usage of strong-smelling agents becomes an important step toward effectively managing disease conditions (European Respiratory Review). However, it is essential to understand that complete avoidance is impractical given the ubiquitous nature of modern everyday life, so researchers emphasise the necessity of developing safer alternatives with minimised health impacts. Additionally, individuals need to observe any worsening symptoms upon exposure and consult their healthcare professionals accordingly.
5. Vigorous Exercise
Vigorous exercise, as defined by the Centers for Disease Control and Prevention (CDC), refers to activities that require large amounts of energy, causing the heart to beat much faster than normal. Such exercises often include running, cycling at a brisk pace, swimming laps, or participating in competitive sports like soccer, basketball, and volleyball, amongst others.
Interestingly enough, vigorous physical exertion has been identified as one of the key triggers of non-allergic asthma. It induces asthmatic symptoms within certain individuals irrespective of allergen exposure (American Academy Of Allergy Asthma & Immunology). Onset these are characterised by coughing, shortness of breath, and chest tightness/pain closely mirroring those experienced during an actual attack, resulting often being misdiagnosed altogether, especially for those who predominantly experience them only under conditions of increased physical activity known as Exercise-Induced Bronchospasm(EIB) ever more challenging to figure out its exact cause leading towards onset this form 'asthma' unlike other types triggered allergens themselves(Mayo Clinic).
The underlying mechanism isn't entirely clear. However, researchers believe it involves dehydration, airway loss of heat from the lungs, and constructive response blood vessels present inside, perhaps playing a significant role(American College Sports Medicine). Hence, while definitely not suggesting people avoid engaging in such healthy practices, moderation, along with professionally guided medical advice, holds paramount importance in ensuring the safety and well-being of the affected person.
It's indeed a delicate balance that needs to be struck - one where the benefits of vigorous exercise are reaped without inciting an asthmatic episode. Therefore, physicians often recommend warming up before exercising and cooling down afterward as preventative measures (American Lung Association). Using certain medications like short-acting bronchodilators prior to undertaking strenuous activities helps some patients manage their symptoms.
Importantly, planning workouts in an environment with moist, warm air tends to avoid triggering EIB whenever feasible, being mindful of the overall intensity duration of each session, and implementing regular breaks allow the body to recover properly(Asthma UK).
Living with non-allergic asthma presents several challenges, vigorous exercise-induced symptoms among them undoubtedly exacerbating difficulty detection management. This condition, more so given its lack of conventional allergenic stimuli, adds complexities around effective treatment protocols; however, continual scientific research alongside educational efforts geared towards public awareness, integral parts striving to improve patient health outcomes, and increasingly prevalent yet less understood disorder.
6. Dry and Cold Air
Dry and cold air refers to an environmental condition characterised by low temperatures and minimal moisture content in the atmosphere. As per several studies, exposure to such conditions emerges as a common non-allergic trigger for asthma exacerbations(American Journal Of Respiratory Critical Care Medicine).
The process occurs when individuals inhale this type of air; it tends to cause bronchial spasm - sudden constriction within the lungs' muscle layer. Effectively triggering what is commonly referred to as an 'allergy attack', although technically inappropriate in the context of non-allergic variations(Canadian Lung Association).
Further medical research suggests that dry, cold conditions indirectly lead to asthmatic episodes by increasing susceptibility to respiratory tract infections, which act as secondary triggers(National Institutes Health). In essence, during winter months, particularly severe weather changes result in aggravated symptoms among those suffering from intrinsic(non-allergic) types of asthma not due to allergens but rather response exacerbated elements like strong winds dropping mercury levels.
It becomes extremely crucial during these times for patients to take preventative measures to avoid situations where they are exposed to extreme atmospheric shifts to protect against flare-ups (Mayo Clinic).
7. Respiratory Viruses and Infections
Respiratory Viruses and Infections, as the term suggests, comprise a group of viral infections primarily affecting the respiratory system. From common colds caused by rhinoviruses to severe conditions such as pneumonia or bronchiolitis induced by viruses like influenza virus or Respiratory Syncytial Virus (RSV), these afflictions pose significant challenges for public health on a worldwide scale every year (Center for Disease Control).
A crucial piece of information regarding Respiratory Viruses and infections is that they exacerbate non-allergic asthma attacks in many individuals who have this condition (National Heart Lung Blood Institute). While viral-induced inflammation typically results from an immune response toward invading pathogens within healthy individuals, asthmatic people display an over-exaggerated inflammatory reaction, which leads to increased airway hypersensitivity, thus provoking acute symptoms such as coughing, wheezing, and breathlessness, among others.
Studies suggest correlations between resultant inflammations post respiratory infection episodes development worsening existing asthmatics cases, specifically those with intrinsic forms, suggesting, therefore, a potential role played herein triggering disease onset amongst susceptible populations moreover necessitating further investigations in this regard(The Journal Allergy Clinical Immunology).
In terms of preventing and managing complications arising due to respiratory infection, particularly pertaining to patients previously diagnosed with non-allergic type, it becomes critical to seek treatment at the earliest sign of trouble and to ensure they receive vaccines for preventable respiratory diseases. For instance, an annual flu shot aids in reducing risks associated with influenza virus - a known catalyst towards severe asthma attacks (American Lung Association). Additionally, individuals might be advised specific practices like maintaining stringent hand hygiene to lower the chances of germs' transmission.
8. Fumes and Chemicals
Fumes and chemicals refer to gases, smoke, or vapour emanating from substances undergoing combustion or reaction; these often contain particulates suspended within them. The presence of certain molecules in such effluvia—whether organic solvents, sulphur dioxide, nitrogen oxides, or other volatile compounds—is known to affect respiratory health negatively.
A link exists between repeated exposure to fumes/chemicals and the development of non-allergic asthma, with the American Journal Of Respiratory Critical Care Medicine suggesting that both acute chronic inhalation irritants directly induce inflammation within airways, thereby triggering asthmatic symptoms.
Particular occupational groups bear a higher risk due to their constant interaction with various hazardous substances. For example, workers involved in gas production, spray painting, welding, etc., face an elevated chance of developing an intrinsic form of disease (National Institute for Occupational Safety Health).
Additionally, factors like tobacco smoke-perfumed products and cleaning agents contribute towards exacerbating conditions among individuals already prone, even setting the stage to develop previously healthy persons, according to the Centers for Disease Control and Prevention).
In essence, while the direct causal relationship is yet fully established, accumulating evidence corroborates a strong association between chemical/fume exposure onset severity and non-allergic type, underlining the importance of effective preventive measures to protect vulnerable populations.

How can Air pollution cause Non-allergic Asthma?
Air pollution has been identified as a significant trigger for non-allergic asthma. The mechanism behind it involves the inhalation of polluted air, which contains harmful contaminants like particulate matter, nitrogen dioxide, and ozone, among others (World Health Organization). These create severe irritation in the lungs, leading to inflammation - eventually manifesting into full-fledged asthmatic symptoms.
The link between air pollution and non-allergic asthma was highlighted by numerous studies, including one conducted by Annenberg et al., where they observed that long-term exposure to traffic-related pollution significantly increased adult-onset cases, particularly those categorised under intrinsic type since these did not involve an allergic reaction but were rather triggered directly due environmental factors (Environmental Health Perspectives).
Another study published in the European Respiratory Journal pinpointed particulate matter specifically as a potent factor initiating inflammatory responses within respiratory tracts, thereupon causing exacerbations among individuals already diagnosed with asthma irrespective of its atopic nature while increasing chances of new-onset disease development in people without prior history thereof.
These findings provide compelling evidence underscoring the association between poor-quality ambient atmospheres and their harmful effects on human health, especially pertaining to the progression of various diseases such as non-allergic asthma, emphasising urgency initiating measures to control and limit exposure to high-risk demographics.
How do Hormonal changes cause Non-Allergic Asthma?
Non-allergic asthma, despite sharing similar symptoms with its allergic counterpart, arises due to factors other than allergens. Hormonal changes serve as one such factor and contribute significantly towards non-allergic asthma. Fluctuations in hormonal levels directly impact the respiratory system's functioning, leading to bouts of breathlessness or wheezing experienced by asthmatics.
A multitude of research studies indicate that hormones play a crucial role in managing immune responses within the body and influence inflammatory pathways involved in various diseases like asthma (Wang & Cheng, 2018). Several scientific reports highlight that during periods of substantial hormone fluctuations, such as menstruation or pregnancy, females often report aggravated asthmatic symptoms (MacSali et al., 2012).
Let's elaborate on this: In women, particularly, high oestrogen levels are associated with an increased frequency of severe asthmatic episodes. The Journal of Allergy and Clinical Immunology published an article detailing how elevated female hormones upregulate proteins causing inflammation, thereby intensifying airway hyperresponsiveness, a significant feature observed among chronic bronchitis patients, which essentially is narrowed airflow passages resulting from sustained contraction (Tiotiu et al., 2020).
Moreover, there lies clear evidence linking stress-level-related cortisol – a key hormone- alterations triggering flare-ups for individuals who have non-allergic asthma. According to a study in The Journal of Allergy and Clinical Immunology, heightened stress levels foster inadequate cortisol responses, leading directly to inflammation and subsequent asthmatic symptoms (Chen et al., 2018).
In contrast, research on the male hormone testosterone suggests it have anti-inflammatory benefits that shield against developing asthma. A paper published by the American Thoracic Society indicates lower instances of diagnosed adult-onset asthma among males, which might be attributed to the protective effect provided by higher testosterone levels generally present in men than women (Lang et al., 2020).
Therefore, based on rigorous scientific exploration, there lies definite proof regarding hormonal changes being instrumental in causing non-allergic asthma.
Are there certain medications that can cause Non-allergic Asthma?
Yes, certain medications do indeed trigger Non-allergic Asthma.
Just as asthma has unique triggers for each individual, medications sometimes become an unexpected catalyst in setting off non-allergic asthma attacks. Notably among these are aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen; ACE inhibitors used to treat high blood pressure; beta blockers that manage heart conditions or migraines; and some pain relievers.
Between 4% and -20 % of asthmatics experience worsened symptoms after consuming NSAIDs, especially aspirin, according to a study presented at the American Thoracic Society Annual Meeting by Dr Katherine Cahill from Vanderbilt University Medical Center. Echoing this finding comes research published in the "Journal of Allergy and Clinical Immunology" which states: "Aspirin-exacerbated respiratory disease is associated with severe sinusitis with nasal polyposis."
Besides NSAIDs, another group causing concern is beta-blockers, which include both eye drops for glaucoma treatment and oral medicine prescribed mainly for hypertension or cardiovascular issues along with migraine management.
"These substances block receptors on bronchial tubes leading lungs into spasms and thereby induce asthma attack," as explained by Dr Anthony Montanaro from Oregon Health & Science University. The American Academy of Allergy, Asthma & Immunology evidences the same. A paper published by them states: "Beta-blockers cause bronchospasm and precipitate asthma attacks."
In addition to NSAIDs and beta-blockers contradictorily, ACE inhibitors used for hypertension treatment might lead to dry cough - a side effect triggering non-allergic asthma symptoms in certain patients as per research conducted at University College London (UCL) Medicine School. "Around 20% patients undergoing ACE inhibitor therapy have been seen developing persistent dry cough; few among these eventually get diagnosed with new-onset asthma," as stated by Professor Ian Pavord.
Moreover, some pain relievers such as codeine aggravate non-allergic asthmatic conditions, according to an article from the Mayo Clinic stating, "Codeine and other medications containing opioids sometimes worsen breathing difficulties."
What are the Symptoms of Non-Allergic Asthma?
Non-allergic asthma is a chronic respiratory condition that does not result from allergens. It's often misunderstood, as it doesn't exhibit the common triggers associated with typical asthma, such as pollen, dander, or dust mites. Instead, environmental factors like weather changes - especially during colder months - tend to trigger non-allergic asthma attacks.
A term acquainted with this disorder in chilly climates is winter asthma. Notably characterised by symptoms propelled and worsened due to cold air exposure. These signs are typically more pronounced during winter seasons, where dropping temperatures pose a considerable risk for those suffering from non-allergic-related bronchial complications.
Understanding how these winter-associated asthmatic reactions occur begins when someone inhales frigid air into their lungs—this results in inflamed and constricted bronchial tubes, leading to what medical professionals refer to as an 'asthma attack'.
Identifying patterns of these bothersome episodes makes managing them efficiently far easier tasks. Thus, recognising prominent winter asthma signs and symptoms becomes critical for maintaining the quality of life under challenging circumstances.
1.Coughing
Coughing is indeed a major symptom of non-allergic asthma, often persisting for weeks or even months if left unmanaged. It tends to be especially prevalent during the colder winter months - serving as one distinct and frequently reported winter asthma sign.
Coughing refers to repetitive spasms aimed at clearing irritants from the bronchial tubes. In individuals with non-allergic asthma, these persistent bouts of cough are typically triggered by environmental factors such as cold air, smoke exposure, or excessive physical exertion rather than traditional allergens like dust mites or pollen.
Generally speaking, how long each episode lasts varies greatly among sufferers based on several individual health variables, including age and overall respiratory condition before onset. However, usually, symptoms prove prolonged over extended periods unless prompt medical attention intervenes to manage them effectively –– sometimes extending up to six to week intervals, according to some clinical reports.
Successfully managing a relentless cough necessitates a two-pronged approach: preventive strategies alongside symptomatic relief measures once an attack ensues. The former includes:
Avoiding known triggers where feasible, such as limiting outdoor activity during exceptionally chilly weather conditions.
Wearing masks to prevent inhalation of irritating substances like cigarette smoke chemicals found in everyday household cleaners, etc.
Engaging in regular exercise to improve lung function capacity ultimately helps reduce the frequency and severity of asthmatic incidents.
When it comes to symptomatic relief measures during an asthma attack, individuals often benefit from prescribed medication usage like bronchodilators or anti-inflammatory inhalers. Bronchodilators work by relaxing the muscles around the airways, thereby allowing more air to flow into and out of the lungs. Anti-inflammatory inhalers play a role in reducing swelling and mucus production within airways - hence easing breathing difficulties.
High-frequency Chest Wall Oscillation (HFCWO) therapy might be another practical intervention tool for some patients dealing with stubborn coughs owing to non-allergic asthma. It entails donning a fitted inflatable vest that vibrates at high frequency, facilitating loosening and thinning down of phlegm lodged deep within lung passages.
Remember always to seek advice from health professionals when devising any treatment plan as each individual's circumstance requires bespoke attention tailored suited to personal needs well underlying condition limitations and severities involved.
Finally, cultivating open lines of communication between care providers is vital in managing chronic conditions such as non-allergic related asthmatic issues; better understanding the signs and symptoms – including persistent troubling coughing episodes – helps forge ahead towards achieving optimal health outcomes despite these inconvenient respiratory hitches life throws path sometimes, especially midst frosty winter seasons!
2. Shortness of Breath
Shortness of breath, scientifically known as dyspnea, characterises a common yet worrying symptom associated with non-allergic asthma. A description of such an experience often encapsulates inadequate air intake or the sensation of gasping for breath.
Shortness of breath manifests due to bronchial tube inflammation and constriction, reducing airflow in and out from its usual capacity. These compartmental contractions occur during an asthmatic episode leading to oxygen deprivation both at rest and activity levels – a primary contributor towards resultant discomfort.
Understanding duration becomes crucial while dealing with 'shortness-of-breath' episodes linked to non-allergic asthma. Typically, instances aligning with severe attacks might last several minutes up until hours unless promptly addressed by medication intervention.
On other occasions - particularly when symptoms are mild - individuals recuperate within mere moments post-exposure removal or cessation of stress-based triggers; however, longevity varies on a case-to-case basis, making it difficult to set definitive time frames applicable universally.
When managing these concerning occurrences, vigilance needs to be maintained around triggering elements like extreme temperatures signifying winter-related complications or even excessive straining through exercises- all potential exacerbators contributing towards symptomatic 'short-of-breath'.
Emphasising breathable environments helps limit the aggravation greatly, especially indoors where control measures are implemented effectively (warm temperatures, clean air). Asthmatic individuals often get advised to don scarves or masks before exposing themselves to cold outdoor environments as a way of preventing an attack.
Implementing stress management techniques such as relaxation exercises and mindfulness is beneficial during periods of increased anxiety – known contributors towards dyspnea exacerbation.
Specific inhaler medications are long-standing treatment options extending quick relief in instances involving sudden breathlessness bouts. In contrast, continuous daily medication doses intended for symptom control over longer durations ensure stable condition management.
Safety measures warrant reinforcement through continuous doctor consultations advising individual-specific emergency plans tailored around unique health patterns aptly addressing any unexpected severe episodes arising suddenly threatening overall well-being without warning. The plan might encompass steps about when seeking immediate medical help becomes necessary following non-responsive initial treatments.
On a parting note, having a comprehensive understanding plays a vital role in handling issues associated with shortness-of-breath episodes stemming from Non-Allergic Asthma, effectively highlighting the importance of staying aware and informed at all times regarding symptoms, manifestations and astute responses, consequently maintaining the quality of life uninterrupted by these avoidable distresses.
3. Wheezing
An integral symptom of non-allergic asthma, wheezing signifies a high-pitched whistling sound while breathing. It arises as air rushes through narrowed respiratory passages characterised by inflamed bronchial tubes - hallmarks of an asthmatic condition.
Wheezing might occur during inhalation (breathing in), exhalation (breathing out), or both, and it's often clearly audible to the person experiencing this distress as well as others around them. Due to its disruptive nature, frequently impacting sleep and daily activities, prompt recognition is crucial for management purposes.
The duration varies based on individual health status - some experience short sporadic episodes lasting minutes only; meanwhile others endure longer bouts spanning several hours. However, if one notices persistent wheezing that refuses to subside despite medication use – immediate medical attention remains essential because it indicates severely impeded airflow, endangering life itself.
Managing such symptoms embodies two collective fronts: trigger avoidance and efficient treatment plan adherence guided under qualified healthcare providers' surveillance.
Trigger Avoidance entails keeping warm indoors when cold weather presents risk factors alongside ensuring adequate moisture levels are maintained through humidifier usage, especially considering dry heated indoor air compounds winter-related asthma difficulties leading towards increased frequency of wheezy eruptions.
Treatment Plan Adherence revolves around medicines prescribed to aid internal airway inflammation control and bronchial muscle relaxation to restore normal breathing. These medications generally fall under two categories: controllers, used daily for long-term symptom management, and relievers that aid in rapidly settling down emergent flare-ups.
Controller medication examples include corticosteroids - which help reduce internal lung inflammation – taken on regular schedules regardless of whether symptoms manifest or not. They function as preventive measures, reducing overall asthma attack severity frequency over time.
Reliever medicines present immediate relief during asthmatic episodes by quickly relaxing constricted airways, aiding comfortable respiration restoration within minutes post-consumption.
Maintaining compliance regarding medicine timing alongside dosages prescribed significantly contributes toward effective wheezing symptom management, paving pathways toward desired health improvement outcomes.
Learning practical stress-management strategies mustn't get overlooked either because emotional upsurges often lead to aggravated respiratory distress instances inclusive of intensified wheezy episodes observed typically amongst those struggling with non-allergic asthma triggers including the winter-associated variant manifestations thereof.
4. Chest Tightness
Chest tightness is a daunting symptom often linked with non-allergic asthma. It feels like pressure or fullness in the chest, making it challenging to take deep breaths. This feeling emerges due to constriction and inflammation of bronchial tubes that carry air into one's lungs.
The duration of this discomfort varies significantly among individuals, with instances ranging from brief spans lasting only a few minutes to prolonged episodes stretching for hours at end. Winter season particularly exacerbates these manifestations, given that cold-induced stimulation triggers such respiratory responses.
Management strategies are central when coping with chest tightness as part of non-allergic asthma symptoms:
Use prescribed medication: Physicians commonly prescribe quick-relief medicines known as short-acting beta-agonists (SABAs). These inhalers help relax muscles around constricted airways, easing breathing almost immediately.
Avoid Trigger Factors: Stay away from stressors leading up to an attack; Cold weather being prominent during winters, wearing scarves over the mouth and nose assists in warming up incoming chilly winds, thereby reducing irritation caused inside air passages.
Deep Breathing Techniques: Practise regular exercises focusing on slow diaphragmatic respiration, helping expand lung capacity, enhancing controlled release and intake of breath, aiding ease off bouts associated with extreme asthmatic pressures within chests
Regular Physical Activity: Engaging in frequent, moderate forms of exercise supports overall lung health. It helps boost cardio-respiratory fitness, providing resilience against asthma symptoms.
Controlled environment exposure: Sudden changes in temperature often trigger non-allergic asthma attacks. Reducing such exposures by staying indoors during frigid weather protects against sudden chest tightening and its associated discomforts.
Consult a professional promptly when experiencing exacerbations or if one's condition doesn't seem to improve despite following advised measures and medication use; it remains imperative to keep medical professionals abreast, ensuring effective management planning for possible future incidents.
By acknowledging these measures, managing chest tightness as part of non-allergic asthma signs becomes achievable. Remembering everyone is unique with differing levels of symptom severity ensures that strategies discussed herein might require personal refinement under professional guidance over time depending on individual responses towards them - all aimed at successfully navigating inconspicuously challenging terrains posed by this unorthodox breed of asthmatic disorder manifesting especially during winters due to cold climatic impacts upon human respiratory systems.
5. Having Difficulty Breathing
Difficulty breathing is an essential symptom of non-allergic asthma. It refers to the challenge one faces when trying to fill one's lungs with enough air. Occurrences might become frequent or sustained, especially during colder months, as a characteristic of winter asthma signs and symptoms.
The duration of such respiratory difficulty varies greatly among individuals, ranging from intense short episodes that last a few minutes to more prolonged distressing periods for several hours. This severity often mirrors the degree of inflammation and constriction in bronchial tubes.
Indeed, managing these uncomfortable signs becomes imperative for those affected by non-allergic asthma. Here are three strategies:
Proper Medication Management: Having quick-relief medicine like bronchodilators around helps alleviate sudden attacks associated with difficulty breathing.
Avoidance Measures: If cold weather exacerbates breathlessness, then limiting outdoor activities throughout peak winter days benefits health significantly.
Use Breathing Techniques: Certain respiratory exercises designed specifically towards aiding asthmatic patients assist immensely; they help control the rate of inhalation and exhalation, supporting smoother airflow.
Remember that each individual's reaction varies; thus, it is crucial to seek medical advice before incorporating any new management technique into daily routines—especially if severe symptoms manifest persistently.
How is Non-Allergic Asthma Diagnosed?
Diagnosing Non-Allergic Asthma often presents an intricate task, as it lacks those typical allergy-induced triggers. It involves progressive steps sifting through the patient's medical history, symptoms they present, and conclusive tests conducted to affirm the diagnosis.
Firstly, a comprehensive evaluation is done of family background, factoring in aspects of existing respiratory illnesses and asthmatic conditions. Following this initial assessment are evaluations delving into individual health histories with emphasis laid upon recurring chest infections or prevalent constant coughs, especially during colder seasons, that signify winter asthma signs and symptoms.
Subsequently, doctors execute lung function tests designed to gauge responsiveness towards certain medications mitigating inflammation within bronchial tubes, such as Albuterol, taken via inhalation form.
"'A significant improvement after using Albuterol usually indicates presence of reversible obstruction suggestive of asthma.' Thus helping differentiate non-allergic mimics like COPD," echoing words by Dr James Li from Mayo Clinic.
Additionally, diagnostic methodologies include imaging studies utilising high-resolution computed tomography (HRCT). "Employing HRCT scans allows for visual confirmation of structural anomalies typically associated with chronic obstructive diseases, thereby aiding precise differentiation between regular allergic reactions versus persistent non-allergic manifestations, " as per the University Of California San Francisco(UCSF).
Therefore, committing to this systematic diagnostic approach helps isolate non-allergic asthma from its allergic counterpart or other respiratory disorders.
Another essential aspect of the diagnosis process involves identifying any adverse environmental triggers, including exposure to cold air, that exacerbate winter asthma signs and symptoms. Consequently, a series of challenge tests become necessary where doctors introduce certain factors under controlled conditions and then monitor lung function.
Spirometry is another key tool in diagnosing Non-Allergic Asthma as it measures how much air an individual breathes out and at what speed after the deepest inhalation possible. According to Johns Hopkins Medicine, "impaired results on spirometry testing further consolidate the presence of airflow obstruction indicative towards asthmatic complications."
What are tests used to diagnose Non-Allergic Asthma?
Non-allergic asthma often poses a challenge to diagnose due to its non-reliance on typical allergens accurately. However, several tests aid in confirming the presence of this condition:
Pulmonary Function Test (PFT): PFTs are employed widely across medical facilities worldwide as they offer detailed assessments regarding lung functionality. They reveal how effectively an individual breathes out or inhales air and consequently detect any operational anomalies that might indicate asthma.
Spirometry: Considered part of PFTs, spirometry measures how much air the lungs hold and how fast one breathes out after taking a deep breath — vital for diagnosing various respiratory diseases such as chronic obstructive pulmonary disease (COPD), asthma, and other conditions affecting breathing capability.
Peak Flow Tests: This test involves using a hand-held device called a peak flow metre, allowing patients themselves to measure lung function at home by blowing into it with maximum force— helping predict forthcoming attacks while gauging their severity, too.
Bronchial Provocation Tests - These involve inducing asthmatic symptoms through physical exertion or exposure to cold temperatures. They prove exceptionally beneficial when pinpointing triggers for winter-induced non-allergic asthma episodes specifically.
Chest X-rays – Although not a definitive means to diagnose asthma, Chest X-rays assist healthcare professionals in ruling out other lung conditions mimicking similar symptoms like bronchitis or pneumonia.
CT Scans: A detailed image representation of the patient's lungs that checks for structural abnormalities potentially linked to respiratory complications.
Allergy Tests: Non-allergic Asthma does not react to traditional allergens; hence, allergy tests become necessary tools in eliminating allergic causes and bolstering non-allergic diagnosis validity by testing responses against common substances such as pollen, dust mites.
Blood Tests – While there are no specific blood tests identifying asthma presence directly, they play a crucial role in determining if an infectious disease might be inducing these symptoms instead. They help analyse overall health status while investigating underlying factors contributing to irregular breathing patterns experienced by patients.
Complete medical history review - Patient's past ailments or familial predisposition towards certain diseases go a long way towards reducing their current state accurately too.
Are the tests for Non-Allergic Asthma accurate?
Yes, the tests for Non-Allergic Asthma are accurate. Medical advances have paved a reliable path to diagnose this type of asthma effectively using several comprehensive examinations.
Pulmonary function tests (PFTs) play an essential role in diagnosing non-allergic asthma. "Spirometry - part of PFTs measures how much air one breathes out and how quickly which often helps identify respiratory issues like persistent inflammation or constriction in bronchial tubes," as per Dr Michael Grippi from the University of Pennsylvania.
Yet another methodology is the Methacholine challenge test used when initial results appear normal despite symptoms suggesting otherwise."The patient inhales increasing doses of methacholine aerosol mist before and after spirometry; it's extremely sensitive at indicating any lung abnormalities including those symptomatic to asthma," in line with Cleveland Clinic's remarks on its precision.
Additionally, meticulous medical history assessments coupled with physical evaluation provide conclusive insight into condition specifics, assisting healthcare professionals in making informed diagnoses.
Other diagnostic methods include Peak Expiratory Flow rate readings that monitor breathing patterns over time, identifying variances indicative of potentially troubling trends pointing towards a conclusion about the presence or absence of asthmatic implications as put forth by Michigan Medicine—"PEF testing complements spirometry data offering invaluable insights subtle respiratory changes."
Thus, results from these tests have shown exceptional accuracy in diagnosing Non-Allergic Asthma. In fact, "a detailed clinical evaluation supported by objective testing has significantly improved asthma diagnosis and given us critical information about disease severity and control," as affirmed by Dr Elizabeth Matsui at Johns Hopkins University.
Another benefit of such accurate diagnostics is the enhancement they bring to personalised treatment plans for patients. It allows doctors to efficiently tailor interventions based on individual response patterns, which produces more effective therapeutic outcomes.
Therefore, advancements in diagnostic techniques ensure that tests offer a high degree of accuracy when diagnosing non-allergic asthma—facilitating medical practitioners with crucial insights and enabling efficacious management strategies curated around patient-specific needs.
How long does the diagnosis last?
Diagnosing non-allergic asthma largely depends on the individual's medical history, along with specific tests run by healthcare professionals. However, a conclusive diagnosis typically takes between one to six weeks.
"The timeline for diagnosing asthma varies greatly; it heavily relies upon symptom severity and frequency," according to Dr. John Winder from Harvard Medical School. Furthermore, he adds that signs such as shortness of breath or wheezing often lead doctors down an investigative path toward potential lung issues - including various forms of asthma.
A key part of the diagnostic process involves multiple visits, usually spread over several weeks, in order to find answers leading toward definitive diagnoses. Evidence provided through these investigations culminates into accurate conclusions after rigorous examinations and testing periods, which might span anywhere from a week up to approximating a month range – hence the stated 'one-six-week' time frame above cited.
Moreover, according to The American Lung Association's Asthma Clinical Research Centers Network analysis based on real-world data spanning 1999-2002, "the process duration—symptom presentation through physician confirmation—is not set stone but rather leans more fluidly across the generalised spectrum."
So, while exact timelines are hard to pin down given the myriad variables at play (including patient responsiveness treatments), understanding that getting a clear-cut Non-Allergic Asthma Diagnosis does require patience and persistence. The process might feel sluggish, yet it's critical to undergo all necessary steps before reaching a precise diagnosis and, subsequently, the right treatment regimen.
The University of Maryland Medical Center reinforces this perspective by asserting: "Each healthcare encounter provides another piece of the puzzle in diagnosing non-allergic asthma, with special emphasis placed on spirometry tests, peak flow monitoring results or even bronchoprovocation testing."
These clinical examinations aid medical professionals immensely in distinguishing non-allergic asthma from other respiratory conditions such as chronic obstructive pulmonary disease (COPD) or bronchitis. These diagnostic measures ensure an accurate diagnosis that ultimately informs effective management strategies for living with this condition—and hence, their crucial role cannot be overstated.

What are the best Treatments for Non-Allergic Asthma?
Non-allergic asthma brings unique challenges. But, with a variety of options available for non-allergic asthma treatment, effective management is within reach.
Inhalers: Two types exist - rescue inhalers provide quick relief during an attack by opening up airways instantly, while control inhalers are taken daily to decrease inflammation in the lungs over time.
Oral medications: Not commonly used, but some examples include leukotriene modifiers and corticosteroids, which help to reduce lung inflammation and relax the smooth muscles surrounding bronchial tubes, respectively.
Immunomodulators: Used when other treatments aren't successful or symptoms are severe. They alter immune system responses, helping prevent breathing difficulties due to pollutants or viruses triggering attacks.
Bronchial Thermoplasty: A relatively new procedure offering hope for those experiencing persistent severe asthma indications uncontrolled by medication alone; this process uses heat energy via radiofrequency waves emitted through a bronchoscope placed into one's windpipe aiming at reducing excess muscle tissue lining inflamed airway walls causing constriction thus resulting in fewer overall exacerbations.
Lifestyle modifications hold significant potential, too. Regular physical exercise aids lung function enhancement, whereas keeping flu immunisation updated acts as a preventative measure warding off infections, thereby limiting sudden onset episodes likely triggered by such illnesses
Controlled Breathing Techniques: Certain exercises like diaphragmatic and pursed-lip breathing help ease the intensity of breathlessness during an attack, improving overall lung function.
Environmental Measures: Since cold air or pollutants might trigger non-allergic asthma attacks, wearing a scarf over the mouth in winter warm incoming air, while staying indoors on heavily polluted days keeps harmful substances at bay.
Maintenance of Healthy Weight: Extra weight places additional strain on the lungs. Achieving and maintaining a healthy body weight often leads to improved lung capacity and reduced symptom severity.
Mitigate Stress Levels: High levels of stress tend to exacerbate symptoms; incorporating relaxation techniques such as yoga or mindful meditation into daily routines aids stress management, significantly mitigating potential triggers associated with emotional distress.
Together, these strategies shape an effective battle plan for combating this daunting respiratory disorder. Individuals suffering from non-allergic asthma must work closely with healthcare professionals, ensuring optimal therapeutic outcomes and tailoring specific needs unique to their health profiles. Remember, each person is different; thus, what works best varies from individual to individual - always maintain open communication lines with doctors regarding ongoing treatments.
Are there home remedies for treating Non-Allergic Asthma?
Yes, there exist home remedies for managing Non-Allergic Asthma. However, it's crucial to note that these methods do not replace prescribed medications or professional medical advice but rather supplement their effects.
Firstly, a critical step involves maintaining acceptable indoor air quality. Since this asthma type responds largely to environmental factors such as pollution and weather changes, ensuring clean breathing conditions inside homes often helps reduce symptom severity significantly.
Air purifiers effectively remove airborne pollutants while humidifiers maintain optimal humidity levels - two measures worth considering in remedial planning. Furthermore, avoidance of irritative aerosols or strong chemical odours contributes immensely to creating conducive living spaces free from likely triggers.
Secondly, lifestyle modifications present a beneficial impact. Regular exercise improves lung function over time, thus reducing breathlessness episodes, which are classical non-allergic asthma outcomes. Note, though, the need for exemplary pre-warm-up exercises prior to initiating vigorous routines because sudden physical exertion might prove counterproductive by inducing asthmatic attacks.
Healthy diets offer additional advantages, with certain foods having anti-inflammatory properties, thereby assisting in mitigating bronchial inflammation characterising this condition.
Thirdly, stress management techniques like yoga or meditation provide valuable benefits, too, given the connections established between emotional health and asthma intensity; decreasing anxiety leads to calmer respiratory patterns, hence minimising attack likelihood.
Remember, however, that while these home remedies have shown potential benefits in managing the symptoms of non-allergic asthma, it remains paramount for those suffering to continue adherence to prescribed medications. These natural and lifestyle-based interventions serve as supportive measures rather than standalone treatments.
Moreover, regular consultations with healthcare providers are essential for necessary adjustments or changes in treatment plans based on response trends toward management strategies already adopted. With each individual's unique experience with this condition comes varied responses necessitating personalised approaches that take into account specific symptom patterns and triggers.
In conclusion, certain at-home procedures do offer significant assistance when dealing with non-allergic asthma, from maintaining optimal indoor air quality, leading an active lifestyle balanced by a healthy diet, to practising stress reduction techniques – all contribute towards more effective disease control. However, relying solely on them without professional medical counsel isn't advisable due primarily to the complex nature underlying this particular form of asthmatic disorder.
Always bear in mind, though, that every person is different. What works well for one might not necessarily suit another, making continual health monitoring important alongside consistent open lines maintained between patient and provider, facilitating any needed tactical reshuffles toward better long-term health outcomes.
Is Non-Allergic Asthma curable?
No, non-Allergic Asthma is not curable. However, it's crucial to understand that while a complete cure remains elusive in the medical world today, management and control of this long-term respiratory condition have proven highly successful with current treatment strategies.
Several studies confirm asthma as chronic; its presence persists throughout life once established. Regardless of type—whether allergic or non-allergic—the same underlying inflammation exists within the airways, leading to characteristic symptoms, including coughing, wheezing, and shortness of breath, amongst others.
Yet despite lacking outright cure options for Non-Allergic Asthma presently in existence, hope must not be lost—for numerous approaches exist aimed at controlling these symptoms effectively, thus improving quality of life substantially over time:
Of particular interest – medication plays a pivotal role in managing flare-ups by reducing lung inflammation while relieving narrowed bronchial passages. Bronchodilators are common agents used during acute symptom periods, though continual usage might warrant anti-inflammatory prescription drugs.
Lifestyle alterations equally bear a significant impact upon severity and frequency of attacks experienced—with weight loss and smoking cessation constituting key areas focus prevention-wise besides adhering strictly towards prescribed medication regimes, always consulting healthcare professional changes noticed whatsoever.




















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews