11 Types of Asthma You Should Know About: Its Causes, Symptoms and Treatment

Related products
Types of Asthma
A chronic respiratory condition that affects people of all ages is asthma. Respiration becomes difficult by narrowing the airways brought on by inflammation and muscle strain. Asthma is no longer seen as a single illness currently. Various classifications are routinely used to categorize asthma. Allergic asthma, Aspirin-induced asthma, Cough-variant asthma, Exercise-induced asthma, Nighttime asthma, Steroid-resistant asthma, and Occupational asthma are some of the many forms of asthma. Numerous management techniques and therapy methods are available to address asthma, depending on its unique form.
1. Allergic asthma
In the lives of many people, allergies play a crucial role. The products a person chooses to use, how they eat, and how they breathe are all affected by allergic responses. The combination of allergens and asthma is referred to as allergic asthma. When exposed to allergens by inhalation, the airways narrow, causing allergic asthma, a kind of asthma. An airborne material, such as pollen, dander, or mold spores, is often the cause of this phenomenon. Because they start asthma symptoms, allergens are often referred to as triggers. Since not all people will respond similarly to the same stimulus, different people will display different reactions.
When an allergen is present, people with allergies have an immune system reaction that sets off a chain of events. The organism activates all its defensive mechanisms to combat potential threats. The immune system executes this process. The immune system is responsible for safeguarding the body against various illnesses. Upon perceiving a potential threat, the immune system initiates the secretion of an immunoglobulin E (IgE) chemical. IgE is intended to exhibit defensive properties and safeguard the human body. Elevated levels of IgE result in bronchoconstriction, leading to respiratory distress.
Asthma is a pulmonary ailment characterised by the constriction of the airways, leading to:
- Inflammation occurs in the airway linings, resulting in swelling and irritation.
- Exhibit excessive production of viscous mucus.
- The airways become constricted due to the contraction of the surrounding muscles.
When does allergic asthma occur?
Most asthmatics have allergic asthma. It is the most prevalent kind of asthma. There are around 25 million asthmatics in the US. In that group, asthma brought on by allergens affects around 60% of the population.
Causes of allergic asthma
Individuals who suffer from allergic asthma experience symptoms triggered by allergens. Allergic asthma is distinguished from other asthma forms by inhaling allergens that elicit asthma symptoms. An asthma attack is the term used to describe severe asthma symptoms.
Which typical allergens cause allergic asthma?
A variety of common allergens frequently trigger allergic asthma. These allergens include pollen, dust mites, mold spores, pet dander, and cockroach droppings. When these allergens are inhaled, the airways become inflamed and narrow, leading to symptoms such as wheezing and coughing.
Allergens are everywhere and have been found in various environments. Indoor and outdoor environments retain these elements. Individuals with allergic asthma get symptom flare-ups upon inhaling allergens that trigger their condition. Understanding the triggers exacerbating asthma symptoms is crucial for effectively managing the condition.
Allergic asthma is often triggered by a variety of allergens, such as:
Dander: Dander, or skin flakes, is commonly shed by pets. Hair is frequently categorised as a prevalent allergen, along with dander.
Pollen: Pollen, a fine powder-like substance, is derived from plants. Grass and weed pollen are the most prevalent allergens that induce asthmatic symptoms in individuals with allergic asthma.
Mold: Mold, a type of fungus, is commonly found in damp environments such as basements. It releases tiny spores into the air, potentially exacerbating asthma symptoms.
Dust mites: Dust mites are tiny creatures that are commonly found in household dust. These microscopic organisms are a type of arachnid and are not.
Dust mites, which are minuscule and resemble arachnids, are commonly found inhabiting the plush surfaces of residential dwellings, such as carpets, upholstery, and clothing. Dermatophagia, a typical behaviour among certain species of organisms, involves consuming skin flakes that individuals naturally shed regularly. The allergenic properties of mites are attributed to both their excrement and their bodies.
Cockroaches: Common household pets are prevalent in various residential and commercial structures. Cockroach feces, saliva, and other body parts trigger asthma.
Seasonal allergies are a common affliction experienced by many individuals. Seasonal allergies are a type of allergic reaction that occurs during specific times of the year. The phenomenon of seasonal allergies is frequently associated with the arrival of spring, owing to the proliferation of numerous plant species. During the spring and summer months, the pollen concentration in the atmosphere tends to be higher than in the fall or winter seasons.
What signs do allergic asthmatics experience?
Many of the symptoms of other forms of asthma are present in allergic asthma patients. These signs manifest as:
- Having difficulty breathing.
- Regularly coughing, especially at night.
- Wheezing (breathing that makes a whistling sound).
- Chest constriction (the sensation that something is pushing on or compressing the chest).
Guidelines for Managing Allergens
Avoid inhaling allergens to manage allergic asthma. Following are some tips:
When pollen levels are high, stay inside. Close all the windows. Use an air conditioner with a clean air filter if it is hot outside. If an old air conditioner smells musty or mold-like, avoid using it. Avoid using evaporative coolers, sometimes referred to as swamp coolers.
To avoid dust mites. These little creatures are found in carpets and clothing. Put allergen-proof coverings on pillows, mattresses, and box springs. Once a week, wash sheets and other linens in hot water. Take off the wall-to-wall carpeting.
Manage the humidity indoors. Use a cheap meter to check. Use a dehumidifier or an air conditioner if the humidity level in the house is greater than 40%. As a result, the air becomes drier, and the development of mold, cockroaches, and house dust mites is slowed. Hire a professional to fix any roof or plumbing leaks.
Check for allergies to pets. Get tested if someone has pets to determine whether they are the source of the issue. Keep them outside or give them to someone else. Eliminate any pets from the bedroom, at the very least. Even after cats no longer reside in a house or apartment, high levels of cat allergies persist there for several months. Cats and dogs are not hypoallergenic. The efficacy of dust or sprays that promise to lessen pet allergies has yet to be established.
Keep the bathroom and kitchen clean and dry to avoid mold and insects. Contact a pest control firm if someone notices cockroach indicators in the house or has allergies. Spraying with insect repellent does not work. One must remove all traces of food from the house, even tiny crumbs on the carpet and oil marks next to the stove. To reduce the humidity in the space, use the exhaust fan when cooking or taking a shower.
Select air filters carefully. Large HEPA room air filters only work while the fan is running to remove smoke and other tiny particles (such as pollen) from a room. They do not minimise dust mites or humidity. Electronic air purifiers produce ozone, which irritates the airways.
When working outside, use caution. Raking and gardening spread mold and pollen. When outside, put on a HEPA filter mask to lessen the number of pollen and mold spores that enter the lungs.
2. Severe Asthma
A kind of severe asthma does not react well to conventional asthma medications. The symptoms are more severe than typical asthmatic symptoms and linger for a long time. Those who have severe asthma frequently have chronic and challenging symptoms.
Severe asthma significantly impacts daily routines, employment, and social life. It affects anyone at any age, including both children and adults. Less than 10% of people have it, which makes it far less prevalent than a typical diagnosis of asthma.
It is efficiently controlled, although it is challenging to deal with, and it takes some time to locate the correct treatment options. One must take good care of themselves by taking medicine as directed, getting frequent asthma reviews, being aware of asthma triggers, and keeping the healthcare team informed. Hence, they alter medication schedules as necessary.
What distinguishes severe asthma from chronic asthma?
All forms of asthma are chronic, long-term diseases, regardless of how mild, moderate, or severe they are. The fact that severe chronic asthma does not improve with standard asthma therapies and drugs defines the condition.
What exactly is severe bronchial asthma?
Another name for severe asthma is severe bronchial asthma. The chronic inflammatory illness of the airways, which is often characterised by bronchial hyperactivity, is referred to by both words.
Signs and symptoms of severe asthma
The signs consist of the following:
- Coughing
- Wheezing
- breathing difficulty
- chest tightness
The signs and symptoms occur both during the day and at night. They impact people's daily activities and capacity for performing typical duties. If severe asthma symptoms are not successfully managed, they become crippling.
Signs of a severe asthma attack
Following are the signs and symptoms of sudden severe asthma attack:
- Having blue-tinged lips, skin, or fingernails
- needing to sit or stand to attempt to breathe more comfortably.
- being perplexed or disturbed
- not being able to form whole sentences.
- being unable to properly breathe in or out due to severe shortness of breath.
- quickly breathing
- symptoms that persist even after being treated with a relief inhaler.
The typical asthma symptoms of wheezing or coughing does not worse during a lousy asthma episode. It occurs because the airways are severely impacted, and one does not breathe deeply enough to produce coughing or wheezing noises in the lungs.
Airway remodelling: Airway remodelling is a plausible long-term consequence of severe asthma, particularly when inadequately managed.
In cases where an individual experiences recurrent severe asthma attacks or persistent unmanageable asthma symptoms, the airways undergo a process of thickening, inflammation, and scarring over a prolonged period. Consequently, the constriction of the airway results in a reduction of its diameter, leading to increased difficulty in respiration and exacerbation of the associated symptoms.
Effectively managing asthma is crucial, even if it appears arduous in cases of severe asthma. Effective management strategies mitigate the likelihood of airway remodelling.
Treatment and management
There is no singular therapeutic intervention or pharmacological remedy. Individuals exhibit varying responses, and an intervention that proves efficacious for one individual does not yield any discernible impact on another. Similar pharmacological agents are sometimes recommended for individuals with less severe asthma, albeit at significantly elevated dosages.
The management of severe asthma is centred on the goal of symptom control. Patients are recommended to minimize their exposure to asthma triggers to decrease the likelihood of experiencing a severe asthma attack.
As an initial measure, individuals diagnosed with asthma are typically prescribed:
The reliever inhaler, typically distinguished by its blue colour, alleviates symptoms as needed and is recommended to be always kept on one’s person.In the event of a diagnosis of severe asthma, it is advisable to consult with a medical practitioner regarding the possibility of obtaining a referral to a specialised clinic. Specific primary care clinics provide specialised support through asthma nurses dedicated to managing this condition.
3. Seasonal Asthma
Seasonal asthma is a variant of allergic asthma wherein the manifestation of symptoms is instigated by allergens that emerge during distinct periods of the year.
Many individuals diagnosed with asthma have allergic asthma. It implies that asthma is induced by allergens present in the surroundings. A significant proportion of individuals diagnosed with asthma concurrently experience allergies, with estimates indicating that this comorbidity affects up to 80% of cases. The relationship between these two conditions is multifaceted and intricate.
Factors that trigger seasonal asthma
Seasonal asthma occurs because of allergenic triggers, such as:
- From August to March or May, individuals experience asthma symptoms due to pollens originating from trees or grasses.
- Mold and mildew are two distinct types of fungi with various variations. Certain molds exhibit a greater propensity for proliferation and dissemination in arid and breezy climatic conditions, whereas others thrive and propagate in moist and humid environments. Individuals who engage in rainforest hikes encounter certain varieties of mold, whereas those who remain indoors during the winter season are exposed to distinct types of fungi within their households.
The impact of weather on human behaviour:
- The inhalation of cold and arid air has the potential to cause irritation to the respiratory tract and trigger the secretion of histamine. Histamine is known to exacerbate allergic reactions.
- The inhalation of hot air, regardless of its humidity level, elicits an asthmatic response.
- The entrapment of pollutants in the atmosphere is exacerbated by heat, thereby elevating the likelihood of allergies and asthma.
Symptoms of Seasonal Asthma
There are several symptoms that people with asthma encounter. These comprise:
- chest tightness or soreness
- shortness of breath
Treatment: The doctor develops a treatment strategy for seasonal asthma that focuses on preventing and managing allergic asthma episodes.
Combinations of over the counter (OTC) and prescription medicines are utilised as part of the treatment plan:
Steroids that are inhaled: Inhaled steroids reduce inflammation in the airways. They reduce symptoms and frequently halt flare-ups before they begin when used regularly to treat allergic asthma.Multipurpose inhaler: Long-acting beta-agonists that lessen oedema and open airways are used in asthma combination inhalers and corticosteroids.
Medication for immediate relief (rescue): If someone experiences an asthma attack, their doctor recommends taking one of several medicines. Inhalable bronchodilators and, when necessary, oral corticosteroids are among them.
Moderator of leukotriene: Cysteinyl leukotrienes, often known as CysLTs, are substances active in the airways and blocked by leukotriene modifiers. Breathing becomes difficult due to the inflammation and constriction brought on by untreated CysLTs.
Mast cell stabilisers: Mast cell stabilising drugs are another class of medications used to treat allergic responses.
Immunotherapy: Immunotherapy is used for moderate to severe allergic asthma, allergy injections are advised. They function by gradually lessening the allergic reaction of immune system.
Occupational Asthma: Occupational asthma has emerged as the most prevalent lung disease in developed nations associated with work-related activities. The precise quantity of newly identified instances of asthma in adults caused by occupational exposure remains uncertain. It has been reported that a proportion of asthma cases in the United Kingdom, amounting to approximately 15%, are attributed to occupational factors.
The cause of occupational asthma is attributed to the inhalation of noxious particles, such as fumes, gases, dust, or other hazardous substances, during work-related activities. Frequently, symptoms tend to exacerbate during workdays or work nights, ameliorate during leisure periods, and subsequently recur upon resumption of work.
It is logical that an individual has exhibited good health previously and is currently experiencing asthma symptoms for the first time. Alternatively, one has experienced asthma during childhood and is currently experiencing a recurrence. Individuals with pre-existing asthma experience exacerbation of their symptoms upon exposure to specific substances in their workplace.
Individuals with a familial predisposition to allergies exhibit a heightened susceptibility to the onset of occupational asthma, particularly in response to specific agents such as flour, animals, and latex.
Individuals with a familial predisposition to a particular disease are still susceptible to its development upon exposure to environmental factors that trigger its onset. Moreover, individuals who engage in smoking behaviour are at an increased likelihood of developing asthma.
Symptoms of Occupational Asthma
- Conjunctivitis (commonly known as a condition characterized by itchy, red, and inflamed eyes)
- Rhinitis (a medical condition characterized by inflammation of the nasal cavity, resulting in symptoms such as nasal congestion, rhinorrhoea, and pruritus)
The manifestation of occupational asthma symptoms depends on the nature of the substance to which an individual is exposed, the duration and frequency of exposure, and various other factors. The presented symptoms potentially include:
- The symptoms tend to worsen as the workweek advances, diminish during weekends and vacations, and recur upon resuming work.
- Manifest in both occupational and non-occupational settings.
- One initiates asthma management either upon initial exposure to an asthma-inducing substance in the workplace or following a sustained exposure period.
- Sustained effects persist even after cessation of exposure. Prolonged exposure to the causative agent of asthma increases the likelihood of persistent or irreversible asthma manifestations.
Causes of Occupational Asthma
Even though new compounds that cause occupational asthma develop every day, some recognized airborne irritants in the workplace include:
|
Irritant |
Example |
Type of occupation |
|
Chemical fumes and dusts |
phthalic anhydride, trimellitic anhydride, and isocyanates |
manufacturers of polyurethane paint, insulation, packaging products, plasticizers, and foam mattresses and upholstery |
|
Animal products |
Protein dusts, bacterial dusts, dander, hair, mites, and tiny insects |
farmers, kennel workers, jockeys, animal handlers, and vets |
|
Organic dust |
Coffee, cereals, grains, flour, and tea |
Bakers, millers, and more food processors |
Treatment for work-related asthma
Avoiding the material that sets off an asthma attack or other symptoms is typically the first line of treatment for occupational asthma. People with occupational asthma must refrain from breathing chemicals like chlorine, nitrogen dioxide, and sulphur dioxide since they exacerbate asthma symptoms. Medication to manage asthma is another kind of therapy. Treatment options for advanced occupational asthma include:
- Medications
- Physical exercise
- Breathing aids
5. Exercise-induced Asthma
Exercise-induced bronchoconstriction (EIB), known as exercise-induced asthma, is a condition characterised by the narrowing of airways during physical activity. Experiencing asthma due to physical activity such as sports or exercise leads to respiratory difficulties. Individuals experience asthma symptoms such as coughing, wheezing, and shortness of breath either during or after engaging in physical activity.
Asthma symptoms occur concomitantly with the constriction or narrowing of the airways during physical exertion. Exacerbation of symptoms is observed in conditions of low temperature and humidity and in instances of elevated pollution levels and pollen concentrations.
Individuals who experience exercise-induced asthma are advised to engage in a warm-up routine before physical activity. Utilising inhalers and other pharmacological interventions has been shown to effectively mitigate the occurrence of exercise-induced bronchoconstriction (EIB) and facilitate bronchodilation.
Is exercise-induced bronchoconstriction a common condition?
Yes. Exercise-induced asthma is a prevalent condition. Approximately 90% of individuals diagnosed with asthma experience symptoms of the condition during or after physical exertion. Individuals without asthma are susceptible to experiencing exercise-induced bronchoconstriction. Exercise-induced asthma is observed in approximately 10% of individuals without a prior asthma diagnosis.
Exercise-induced asthma affects individuals of all ages, including both children and adults. Individuals with asthma and allergies exhibit a higher propensity to develop the medical condition. The prevalence of asthma induced by sports is higher among high-level athletes, such as those who participate in the Olympics and those who play professional football, soccer, and hockey.
Symptoms of asthma induced by physical activity:
The severity of symptoms varies from mild to severe. The onset of these symptoms manifests within a few minutes of commencing physical activity or upon completion of a workout. The amelioration of symptoms typically commences after approximately 30 minutes of rest.
Exertion-induced asthma is characterised by a range of symptoms elicited by physical activity.
- Experiencing coughing following physical activity such as running or exercising. For specific individuals, coughing represents the sole manifestation of their condition.
Causes of exercise-induced asthma:
Exercise-induced asthma is triggered by intense physical activity and cold and dry air exposure. During periods of rest, individuals typically respire through their nasal passages. The nasal cavity performs the function of heating and humidifying the inhaled air as it passes through the nostrils.
The severity of asthma symptoms triggered by physical exercise is exacerbated under certain circumstances.
- The atmospheric conditions are characterized by low temperature and low humidity.
- The levels of pollen are currently elevated.
- Elevated pollution levels have resulted in suboptimal air quality.
- The individual is in the process of recuperating from a cold or respiratory ailment.
- The smoke, chemicals, or fumes emanating from paint or cleaning supplies has been inhaled.
Strategies for the Prevention and Management of Exercise-Induced Asthma
- It is recommended to utilise pre-exercise inhaled medications consistently.
- Engaging in warm-up exercises prior to physical activity and incorporating a cool-down period following exercise is recommended.
- In the event of cold weather, engaging in indoor exercise or utilizing a mask or scarf to cover the nose and mouth is advisable.
- It is advisable to refrain from engaging in outdoor physical activities during periods of high pollen counts, mainly if one is susceptible to allergies. Additionally, it is recommended to avoid outdoor exercise during periods of elevated air pollution.
- It is advisable to restrict physical activity during a viral infection.
- Engaging in physical activity at a suitable intensity level commensurate with one's individual fitness level is advisable.
It is important to note that asthma must not be utilised as a justification for abstaining from physical activity.
6. Nighttime Asthma (Nocturnal Asthma)
About 75% of asthmatics experience nocturnal symptoms at least once a week, a regular occurrence. An individual is more prone to develop nighttime symptoms if they have either more severe or poorly managed asthma.
Although the reasons why asthma symptoms worsen at night are not entirely known, they are linked to the typical hormonal changes that occur in the evening. Numerous hormones exhibit circadian rhythms, which are 24-hour cycles linked to the body's internal clock, such as epinephrine, cortisol, and melatonin. The likelihood of nocturnal asthma symptoms rises due to changes in these hormones that take place in the evening. Pregnancy hormone changes have an impact on asthma symptoms.
Additionally, obesity makes it more challenging to control asthma and raises the risk of nocturnal asthma. Researchers have proposed that higher systemic inflammation and extra body fat in the neck region factors in nocturnal asthma in obese individuals, even if the connection between the two is not entirely understood.
The medical condition known as acid reflux, known as gastroesophageal reflux disease (GERD), is another one that is frequently linked to nocturnal asthma. Up to 80% of those with asthma have GERD symptoms, such as heartburn and regurgitation.
Symptoms of nocturnal asthma
While the symptoms of both types of asthma are the same, some of the nocturnal asthma symptoms, such as:
- breathing difficulty
- chest constriction
Additionally, people, particularly youngsters, acquire other sleep difficulties, such as:
- excessive sleep during the day
- maintainable insomnia
- breathing problems during sleep, such as sleep apnoea.
- sleep disorders such as sleepwalking
Nocturnal Asthma Triggers: Environmental factors cause nocturnal asthma and obesity, GERD, and circadian hormonal abnormalities.
Tobacco smoke: Smoking and exposure to second-hand smoke irritate the airways and impair lung function.
Allergens in the bedroom: Many persons with asthma are susceptible to dust mites, animal dander, mildew, pollen, and droppings from pests like cockroaches and mice. Even if a person is exposed to specific allergens during the day, a delayed allergic reaction does still cause asthma to flare up at night.
Diet: Sulphites, present in foods and drinks such as beer, wine, dried fruit, processed potatoes, and shrimp, cause sensitivity in certain asthmatics. These foods cause nocturnal asthma if they are ingested too soon to bedtime.
Medication: When taken too close to sleep, several drugs, such as aspirin, cold treatments, vitamins, and even eye drops, cause nocturnal asthma.
Cold air: A typical daytime trigger, cold air cause symptoms at night if the bedroom is freezing or a window is left open.
Other medical conditions: Some of the most frequent causes of nocturnal asthma episodes include viral illnesses such as the flu, the common cold, and sinus infections.
7. Cough-variant Asthma
Cough-variant asthma is one in which the main symptom is a dry, unproductive cough. (An unproductive cough does not remove mucus from the respiratory system.) Other asthma symptoms, such as wheezing or shortness of breath, are often absent in people with cough-variant asthma.
Chronic coughs last longer than 6–8 weeks, and cough-variant asthma is one of the most common causes of these coughs. Coughing throughout the day and at night are both signs of asthma. If one has nocturnal asthma, sleep disturbances may occur.
Causes of cough variant asthma
Although the origins of CVA are not fully known, the following triggers frequently result in an asthmatic cough:
- Exposure to irritants or allergens
- an upper respiratory illness, such as sinusitis or a cold
- taking drugs
- exercise
- variations in the climate
Asthma and allergies unquestionably go together. It is estimated that 80 percent of patients with asthma have nasal allergies. When the immune system overreacts to something that ordinarily does not trigger a reaction, allergies result. It shows that CVA and the immune system are related.
Symptoms of cough variant asthma
CVA features a persistent cough without mucous. Frequently, this is the only symptom. Any cough that lasts longer than 8 weeks in adults and more than 4 weeks in children is considered persistent.
Steps to reduce the risk of cough variant asthma:
Asthma attacks and exposure to smoke increase the risk of developing CVA. To reduce the risk, avoid smoking in public areas and ask friends and loved ones not to smoke in common areas. Pregnant women must avoid smoking as it increases the risk of developing asthma. Obesity is linked to more asthma attacks than leaner patients, so managing extra body weight reduces the chances of developing CVA. Exposure to allergens, such as hay fever and dermatitis, increases the risk of developing CVA.
Children who develop wheezing and other viral infections in the breathing tract develop CVA later. Following these lifestyle changes reduces the risk of developing CVA and maintaining a healthy lifestyle.
8. Non-Allergic Asthma
Is there a correlation between extreme weather conditions, such as the high temperatures of summer or the low temperatures of winter, and the exacerbation of asthma symptoms? Is there a correlation between illness and the likelihood of experiencing an asthma exacerbation? Is there a correlation between stress and the onset of respiratory issues? If such is the scenario, it is plausible that the individual is experiencing non-allergic asthma.
Causes of non-allergic asthma
Nonallergic asthma occurs when something other than an allergen prompts the immune system to react by producing antibodies that lead to inflammation.
Asthma that is intrinsic or nonallergic is brought on by:
- dry or chilly air
- humidity and heat
- air toxicity
- smoke
- fumes and chemicals
- fragrances
- stress
- anxiety
- difficult exercise
- viruses or respiratory illnesses
- hormone adjustments
- several medicines
Uncertainty exists regarding the fundamental causes of nonallergic asthma development. The interaction of genetic and environmental factors that contribute to the development of asthma is still being researched.
Lifestyle changes to reduce non-allergic asthma:
Changes in lifestyle help with asthma symptoms and asthma attacks. Several recommendations are.
- Reduce tension.
- Avoid smoking.
- Avoid pollutants, smog, and second-hand smoke.
- Avoid using cleaning chemicals with strong odours.
- Keep a healthy weight.
- Obtain a flu shot.
- Maintain hygienic practices to lower the risk of infection.
9. Asthma COPD Overlap
The condition is deemed severe when asthma symptoms are challenging to treat and control.
A group of lung conditions known collectively as chronic obstructive pulmonary disease (COPD) impair airflow and lead to breathing difficulties. Emphysema, chronic bronchitis, and refractory (severe) asthma are some of the illnesses in this category.
Most asthmatics do not go on to develop COPD, and many asthmatics do not have COPD. It is feasible to have both, however. When both conditions are present simultaneously, it is known as the asthma-COPD overlap syndrome (ACOS).
Signs and symptoms
ACOS symptoms include:
- repeated coughing
- excessive mucus
- Being worn out
- inadequate physical capacity for exercise
- Having trouble breathing while performing everyday tasks
Triggers
Allergens like pollen, dust mites, cockroaches, mold, and animal dander are frequently asthma triggers. Allergens exacerbate the symptoms of COPD. Additionally, untreated allergies and asthma in some people increase their risk of developing COPD. However, COPD is not the same as asthma, nor is it brought on by allergies or asthma. COPD is a group of lung conditions. Asthma is included in the collection on occasion, but only sometimes.
The most significant risk factor for developing COPD is smoking. Smoking is a risky exacerbate of all respiratory conditions. It shortens life expectancy and obstructs medical treatment. Quitting smoking is the most crucial thing one must do for one’s health.
Therapy Alternatives
Although there is not a single drug that treats ACOS, three different classes of medications lessen symptoms. These consist of the following:
Inhaled corticosteroids at low doses: A typical asthma medication used for long-term management that addresses lingering airway irritation.
LABA, or long-acting bronchodilator: A medication for long-term asthma treatment that keeps the airways open for longer (12–24 hours). Combining this medication with another anti-inflammatory drug is recommended rather than taking it alone.
LAMA, long-acting muscarinic agonist: A typical medication for the management of COPD symptoms. It prevents mucus production and airway constriction.
10. Aspirin Induced Asthma
A form of asthma brought on by aspirin is known as aspirin-induced asthma. Non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen, are additionally known to trigger it. Aspirin-exacerbated respiratory disease (AERD) is another name for asthma brought on by aspirin.
Approximately 10% of people with asthma are NSAID-sensitive. For those with severe asthma, this rate is twice as high. Approximately 30 to 40% of people with nasal polyps and asthma are sensitive to NSAIDs.
Signs and Symptoms
The following list of symptoms indicate an aspirin-induced reaction:
- Runny or stuffed nose
- itching, swollen, or watery eyes
- facial and neck redness
Many persons who have aspirin-induced asthma experience modest alcohol responses. The list of potential aspirin-induced reactions symptoms is not exhaustive. People with severe asthma experience more severe symptoms.
Causes of aspirin induced asthma
There are two distinct issues with the airways that contribute to asthma symptoms.
- One issue is that the airway muscles constrict, resulting in wheezing and a tightening sensation in the chest.
- The other issue is swelling, itchiness, and excessive mucus buildup in the airways. When someone has asthma, the signs frequently begin after a trigger exposure.
How Aspirin induced asthma is treated?
AIA is treated with three types of drugs, like other types of asthma: steroids, long-term control medications, and quick-relief therapies. While long-term control drugs are used daily to prevent symptoms, quick-relief treatments are used just when an asthma attack occurs. Steroid drugs, often known as asthma controller medications, help with symptom management by blocking chemicals that irritate and inflame the airways. Even when no symptoms are present, these drugs must be taken daily since they do not successfully halt wheezing during severe asthma attacks.
Aspirin desensitization is a treatment strategy for some people that involves taking a low dose of aspirin in a hospital setting with emergency help. The dosage is gradually raised until a usual quantity is consumed without causing symptoms. A certified healthcare practitioner must oversee this process. When a usual dose is taken without symptoms, asthma drugs are not needed as often, boosting asthma control.
11. Steroid-resistant Asthma
Asthma resistant to treatment with corticosteroids, frequently used to manage and control asthma symptoms, is referred to as steroid-resistant asthma, sometimes known as corticosteroid-resistant asthma. It is challenging to manage the inflammation and symptoms of asthma in this disease because the airways in the lungs are less receptive to the anti-inflammatory actions of steroids.
Causes of steroid resistance asthma
Determinants of steroid-resistant asthma:
- genetic influences
- allergens in the environment
- Workplace exposures
- Smoking
- breathing infections
- Obesity
- air toxicity
- Medications
- treatment noncompliance
- reworking the airways
Signs and symptoms
Signs and symptoms of asthma caused by steroid resistance:
- breathing difficulty
- persistent cough
- breathlessness becoming worse with exercise.
- recurring asthma attacks or flare-ups
- limited effectiveness of common asthma medicines, such as corticosteroids
- Despite therapy, airway inflammation persists.
- reduced lung capacity as shown by spirometry testing.
How to know what type of asthma I have?
To figure out how to know the type of asthma a person has it is helpful to consult with a doctor. Identifying the specific type of asthma necessitates a thorough assessment by a qualified healthcare practitioner. A doctor is able to use various diagnostic methods to identify and confirm the presence of asthma in patients.
The process of determining the classification of asthma involves the following steps:
The individual's personal and medical background: The physician inquiries about the patient's symptoms and underlying causes to gain a comprehensive understanding. It is advisable to bring the relevant notes to respond to inquiries posed by one's healthcare provider. Prepare oneself to respond to inquiries regarding one's familial background of asthma and allergies, the pharmaceutical substances one consumes, and overall way of life. Please ensure that one is prepared to discuss any existing physical issues, conditions, or concerns that one is experiencing.For instance, individuals with a documented medical history of allergies or eczema are more likely to develop asthma. Moreover, a familial background characterised by a history of asthma, allergies, or eczema augments an individual's likelihood of developing asthma. The above information is helpful for medical professionals in formulating a diagnosis.
It is imperative to inform one's healthcare provider regarding any instances of exposure to environmental factors within the home or workplace that potentially worsen asthma symptoms. For instance, potential allergens encompass pet dander, pollen, dust mites, mold, cockroaches, and certain food items in specific individuals. Asthma is often induced by the environmental irritants such as cleaning chemicals and tobacco smoke.
The physician asks about chest symptoms during instances when individuals,
- Acquire a common cold.
- Exercise
- Utilise pharmacological agents with specific properties, such as non-steroidal anti-inflammatory drugs (NSAIDs).
- Individuals are experiencing heightened levels of stress.
Physical examination: The physician performs a comprehensive physical examination to identify indications of asthma or other associated medical conditions. The healthcare professional thoroughly examines various physiological indicators, including the auditory apparatus, ocular structures, nasal passages, oropharyngeal region, and integumentary system, and auscultates the thoracic cavity and assesses pulmonary function. To evaluate an individual's overall health, healthcare professionals commonly employ measurements of height and weight, which are subsequently utilised in conjunction with lung function tests. In addition, a device known as a pulse oximeter is utilised. The device is worn on the finger and quantifies the oxygen saturation level in the bloodstream. In addition, it is sometimes necessary to undergo radiographic imaging, such as an X-ray, to assess the condition of pulmonary or sinus regions.
Lung function tests: Lung function tests ascertain the efficacy of inhalation and exhalation of air from the pulmonary system. To establish a diagnosis of asthma, medical professionals administer one or multiple pulmonary function tests designed to assess respiratory function. Lung function tests are alternatively referred to as pulmonary function tests. These assessments evaluate respiratory function.
Lung function assessments are frequently conducted both before and after administering a medication referred to as a bronchodilator. If there is a significant improvement in lung function following the administration of a bronchodilator, it is likely indicative of the presence of asthma. The physician recommends a therapeutic trial of asthma medication to assess its efficacy.
Several commonly employed lung function tests are utilised to evaluate the condition of an individual's airways.
Spirometry: Spirometry is a pulmonary function test that assesses both the volume of air inhaled and exhaled and the rate of exhalation.FeNO test: The FeNO test, known as the exhaled nitric oxide test, is a diagnostic tool used in clinical settings to measure nitric oxide levels in a person's exhaled breath.
A diagnostic tool was utilised to evaluate inflammation within the respiratory passages.
Bronchial provocation or "trigger" tests: These are diagnostic procedures used to assess the sensitivity and responsiveness of the bronchial airways.
Allergy Tests: Seeking consultation with an allergy specialist is advantageous. Most individuals diagnosed with asthma experience allergies that serve as triggers or exacerbate their asthmatic symptoms.
Blood tests: Blood tests are a diagnostic tool commonly used in medical practice to assess various aspects of a patient's health.
Blood tests are requested by medical professionals to assess the functionality of immune system. The levels of eosinophils, a type of white blood cell, and immunoglobulin E (IgE), an antibody, are assessed. Elevated levels of this nature potentially indicate the presence of severe asthma.
Is it within the scope of medical practice for physicians to conduct tests for conditions other than asthma?
If a medical professional suspects a condition other than asthma or one associated with asthma, additional diagnostic examinations are conducted. Diagnostic procedures encompass a chest radiograph, acid reflux assessment, sinus radiography, or other pertinent specialised examinations. In addition, medical professionals conduct allergy tests, which include blood or skin tests. Allergy tests are not employed to ascertain the presence of asthma. However, individuals who experience allergies potentially elicit the onset of asthma symptoms.
There exist additional medical conditions that exhibit comparable symptoms to asthma. The healthcare provider conducts an assessment to determine the presence of various conditions, including:
- The presence of atypical or deviant air passages.
- Gastroesophageal reflux disease (GERD)
- Allergies
- Cystic fibrosis, typically identified during infancy or early childhood,
- Chronic obstructive pulmonary disease (COPD), a condition typically diagnosed in adults,
- The two respiratory conditions under consideration are pneumonia and bronchitis.
- Immune disorders are medical conditions characterised by dysregulation or malfunctioning of the immune system.
- Nasal polyps are the benign growths in the nasal cavity and paranasal sinuses.
Classifications of asthma.
Asthma is classified into four levels, determined by the severity of the condition. The frequency of symptom occurrence and the measurement of lung function are critical determinants of an individual's asthma severity. The physician inquiries about various aspects, including:
- What is the frequency of the symptom manifestation?
- What is the frequency of nocturnal awakenings due to coughing?
- What is the frequency of respiratory difficulties?
- Do individuals encounter difficulties in performing their routine activities, including physical exercise?
- What is the frequency of using a quick-relief (rescue) inhaler?
- What is the frequency of visits to the emergency room or hospitalisation to manage symptoms associated with asthma?
The responses to these inquiries aid in determining the extent of one's asthma condition. Various treatment modalities are available for individuals with intermittent or persistent asthma.
What is the most serious type of asthma?
The most serious type of asthma is Status asthmaticus.
- Status asthmaticus is a state of respiratory failure associated with the most severe manifestation of severe acute asthma, commonly known as an asthma attack. In a rapid onset attack that proves unresponsive to conventional treatment, the potential consequence is the development of status asthmaticus. In such cases, hospitalisation is necessary to administer the appropriate medical intervention. In the event of a severe asthma exacerbation where the efficacy of both the rescue inhaler and nebuliser is insufficient, prompt medical attention is imperative.
If an individual possesses a steroid medication, such as prednisone, it is advisable to administer a dosage prior to proceeding to the emergency room.
Asthma is a prevalent condition among a significant portion of the population. There exist Numerous therapeutic interventions to manage the condition effectively. Adherence to the asthma action plan devised in consultation with a healthcare professional, avoidance of triggers, consistent medication usage, and regular attendance of medical appointments are crucial components for effective asthma management.
However, it is essential to note that asthma attacks occur, and specific severe episodes are classified as emergencies.
What is the most common type of asthma?
Based on data from the Centres for Disease Control and Prevention (CDC), it is estimated that approximately 1 in 13 individuals in the United Kingdom are affected by asthma, making it the prevailing chronic condition among children. Like numerous medical conditions, asthma exhibits varying effects on individuals — whereas some individuals experience only mild symptoms of the disease, others endure frequent and potentially life-threatening asthma attacks.
Some common types of asthma
- Allergic asthma
Allergic asthma is widely recognised as the predominant variant of asthma, with a global prevalence estimated to impact approximately 16 million individuals. Individuals diagnosed with allergic asthma do not encounter an asthma attack unless exposed to substances that elicit an allergic response, such as dust particles, animal dander, mold spores, or pollen grains.
- Adult-onset asthma
While it is commonly believed that asthma primarily develops during childhood, this assumption does not always hold. A considerable number of individuals encounter the initiation of asthma during their third and fourth decades of life. The causation of adult-onset asthma still needs to be fully comprehended. However, it is widely recognised that different airway irritants, such as smoke and mould, possess the capability to serve as triggers for this condition.
It is noteworthy to mention that the mortality rate linked to adult-onset asthma is considerably higher compared to that of childhood asthma. The observed discrepancy is commonly attributed to the inclination of adults to disregard their symptoms or misconstrue them as outcomes of increased body mass and the natural ageing process.
- Childhood asthma
Childhood asthma is a widely observed respiratory ailment that impacts a substantial population of children globally. A persistent and long-lasting nature characterises the condition.
Although childhood asthma is not classified as a separate condition from adult-onset asthma, children face unique challenges due to the constriction of their airways. Childhood asthma is a chronic condition that lacks a definitive cure. However, effective management strategies exist to control the symptoms associated with this condition, commonly manifest as recurrent coughing, difficulty breathing, and chest congestion.
If indications suggest the potential development of asthma in a child, it is imperative to seek the expertise of a specialist promptly. Timely intervention is crucial as it offers the most favourable opportunity for mitigating the risk of an asthma attack.
What is the most severe age for asthma?
Children and adolescents are especially susceptible to asthma due to the severity of its effects on this age group. Numerous studies consistently emphasise that childhood asthma is a significant health issue. Based on data from the Centres for Disease Control and Prevention (CDC), it is evident that asthma has a prevalence rate of approximately 7.7% among children in the United States, thereby establishing it as the most prevalent chronic ailment in this demographic. Various factors, including genetics, early-life exposures such as allergens and pollutants, respiratory infections, and a familial predisposition to asthma, contribute to the elevated prevalence observed within this age group.
(Individuals who are typically between the ages of 18)
The prevalence of asthma tends to decline during the late adolescent and early adult stages. Multiple studies have documented a reduction in the manifestation of asthma symptoms and a decline in the overall incidence of asthma within this age. Various factors, such as hormonal fluctuations, lifestyle decisions, exposure to allergens or irritants, and adherence to medication regimens, impact the continuity or cessation of asthma symptoms during this phase.
Asthma manifests at any stage of life, and many individuals encounter their initial asthma symptoms during adulthood. Available research suggests a notable prevalence of adult-onset asthma among individuals diagnosed with asthma. The prevalence of asthma in adults is attributed to various factors, including genetic predisposition, occupational exposures, environmental factors, obesity, and comorbidities such as allergies and respiratory infections. Additionally, it must be noted that hormonal fluctuations in females, specifically during the stages of pregnancy and menopause, have the potential to impact the onset or worsening of asthma symptoms during adulthood.
Although asthma is frequently linked to children and young adults, it is crucial to acknowledge its effects on the elderly demographic. The prevalence of asthma among the elderly exhibits’ variation across different studies; however, available evidence indicates that asthma persists or emerges de novo within this age demographic. Implementing accurate diagnosis and effective management strategies is paramount in mitigating potential complications and promoting a high standard of living among elderly individuals with asthma.
Asthma has the potential to impact individuals of all age cohorts, although its occurrence and attributes exhibit substantial variation. Asthma poses a significant health concern in paediatric populations, as children and adolescents exhibit the highest prevalence rates. As individuals progress into adulthood, there is a general trend of decreased prevalence of asthma. However, it is essential to note that asthma in adults, which emerges later in life, is a significant phenomenon. It is imperative to acknowledge the significance of the elderly population, given the potential for the persistence or emergence of asthma within this demographic. Various factors, including genetic predisposition, environmental exposures, lifestyle choices, and other medical conditions, influence asthma prevalence in various age groups. Comprehending these age-specific patterns is crucial for developing customized management strategies, timely intervention, and enhanced overall outcomes for individuals diagnosed with asthma.
What is the common medication for asthma?
The selection of appropriate medications is contingent upon various factors, including but not limited to age, symptoms, asthma triggers, and the most effective means of managing asthma symptoms.
Preventive medications with long-term efficacy aim to mitigate inflammation in the airways, thereby alleviating associated symptoms. Bronchodilators, commonly known as quick-relief inhalers, rapidly alleviate the constriction of airways, thereby facilitating improved respiratory function. In certain instances, the administration of allergy medications becomes imperative.
Long-term control medications for asthma
Long-term control medications for asthma, typically administered daily, serve as the fundamental basis for treating asthma. These pharmaceutical interventions effectively manage asthma symptoms daily and reduce the likelihood of experiencing asthma exacerbation. There exist various categories of long-term control medications.
It is necessary to administer these medications over an extended period, ranging from several days to weeks, to achieve their optimal therapeutic effects. In contrast to oral corticosteroids, the administration of inhaled corticosteroids is associated with a comparatively diminished likelihood of encountering severe adverse effects.
Leukotriene modifiers are a class of pharmaceutical agents that are used to modulate the activity of leukotrienes. These oral medications are effective in alleviating symptoms associated with asthma.
The utilisation of Montelukast has been linked to various psychological responses, such as agitation, delusions, depression, and self-harm. It is crucial to quickly seek medical consultation if an individual experiences any of the abovementioned reactions.
These pharmaceutical preparations consist of a combination of a long-acting beta-agonist and a corticosteroid. Theophylline is an oral medication administered daily, which exerts its therapeutic effect by inducing relaxation of the smooth muscles surrounding the airways, thereby facilitating airway patency. Combination inhaler is less frequently utilised than other treatments for asthma and necessitates regular blood tests.
Quick-relief medications
Quick-relief (rescue) medications are administered as needed to provide a prompt and temporary alleviation of symptoms during an asthma episode. They are utilised before physical activity if a medical professional advises them. Various categories of quick-relief medications are available to manage certain medical conditions.
- Short-acting beta-agonists
Short-acting beta-agonists (SABAs) are a pharmacological category frequently employed for managing respiratory disorders, notably asthma.
Inhaled bronchodilators offer prompt relief within a matter of minutes by mitigating symptoms during an episode of asthma.
Short-acting beta-agonists are typically administered using a portable, handheld inhaler or a nebuliser. The inhaler is a compact device that allows for the direct delivery of asthma medications. At the same time, the nebuliser is a specialised apparatus that converts these medications into a fine mist for inhalation. These substances are administered through inhalation using either a facial mask or a mouthpiece.
Anticholinergic agents refer to a class of medications that inhibit the action of acetylcholine.
Like other bronchodilators, ipratropium and tiotropium exhibit rapid onset of action, promptly inducing relaxation of the airway smooth muscles, thereby facilitating improved respiratory function. Corticosteroids are primarily employed in managing emphysema and chronic bronchitis, although they are utilised to treat asthma.
- In the event of asthma exacerbation, the prompt administration of a quick-relief inhaler promptly alleviates symptoms. However, the frequency of reliance on quick-relief inhalers must ideally be minimised when long-term control medications effectively manage the condition.
- Maintaining a log of the number of inhalations administered every week is advisable. If an individual finds themselves utilising their quick-relief inhaler more frequently than advised by their healthcare provider, it is advisable to schedule an appointment with said healthcare provider. It is advisable to consider modifying the long-term control medication.
Bronchial thermoplasty
Bronchial thermoplasty is a medical procedure that involves the application of thermal energy to the airway walls.
Bronchial thermoplasty is indicated for cases of severe asthma that exhibit an inadequate response to inhaled corticosteroids or alternative long-term asthma pharmacotherapies. The availability of this product is limited, and its suitability varies among individuals.
Bronchial thermoplasty is a medical procedure in which a healthcare provider uses an electrode to apply thermal energy to the inner linings of the pulmonary airways. The application of heat results in a reduction in the contractile ability of the smooth muscle situated in the airways. It hinders the ability of the respiratory passages to narrow, thus aiding respiration and potentially reducing the likelihood of asthma exacerbations. The therapeutic intervention generally comprises three sessions conducted on an outpatient basis.
Stepwise approach to treatment based on the severity of the condition.
The recommended approach to treatment must be adaptable and responsive to fluctuations in one's symptoms. The attending physician must inquire about the patient's symptoms during every consultation. A doctor modifies treatment based on the signs and symptoms present.
For instance, in cases where an individual's asthma is effectively managed, a healthcare professional opts to reduce the prescribed medication dosage. If an individual's asthma is not effectively managed or is deteriorating, medical practitioners augment the prescribed medication regimen and advise more frequent consultations.
Asthma action plan.
Collaborate with a doctor to establish an asthma action plan that entails documenting the appropriate medication administration timing and the circumstances under which dosage adjustments must be made in response to symptomatology. Additionally, it is essential to provide a comprehensive compilation of the triggers that elicit a negative response and the corresponding measures that must be undertaken to prevent their occurrence.
In addition, a doctor suggests monitoring asthma symptoms or employing a peak flow meter at regular intervals to assess asthma management's efficacy.
How can a GP consultation identify what type of asthma a person has?
The distinct types of asthma share a range of similar symptoms that contributes to making the confirmed diagnosis of asthma. This is challenging at times when the doctor needs to know about the specific type of asthma a person has with the help of limited knowledge about the occurring symptoms and complaints of that patient.
General Practitioners (GPs) are doctors who treat common and chronic illnesses in a specific region and refer complicated cases to hospitals. Asthma is a common health disorder whose prevalence depends on the extent of exacerbating factors in that area. GPs play a significant role in determining and identifying the type of asthma by the following methods:
Patient Medical History: A comprehensive medical history is of utmost importance in diagnosing and treating any sort of health condition. A GP must inquire and formulate a complete medical history of the respective patient. A medical history includes records of previous illnesses, symptoms onset of the current illness, the severity of symptoms and the factors that caused it. Moreover, detailed knowledge of family history is also important to understand the pattern of the possible health condition. A detailed and accurate medical history is enough to hint to the GP with a diagnosis which is later confirmed by following the protocols.
Symptoms Consideration: However slight, differences persist between the distinct types of asthma. These differences are due to the extent of symptoms and how they occurred in the first place. Allergic asthma is due to different potent agents such as dust, mites, pollen, etc., whereas exercise-induced asthma occurs after excessing physical exertion. This discussion indicates that inquiry and knowledge of symptomatology are mandatory for GP to reach the final diagnosis and treat accordingly.
Physical Examination: A thorough physical examination helps diagnose asthma. The chest examination is significant in the overall general physical assessment. The GP uses a stethoscope to carefully listen to and assess the lung sounds. A wheezing chest is the characteristic finding of asthma along with other clinical features. Similarly, atopic facies and recent eczema on skin clues towards allergic associations.
Treatment Outcome: In the diagnosed cases of asthma, treatment outcome holds charge of determining the type of asthma. Short-acting and long-acting bronchodilators act by targeting specific goals. The GP prescribes medication based on acute symptoms. Short-acting bronchodilators are a group of medications for asthma that alleviates acute symptoms and shows evident improvement if the asthma is easily reversible.
However, if the symptoms do not improve by following the short course, the GP advises long-acting bronchodilators along with corticosteroids to treat the advanced forms of asthma. These treatment plans help with identifying the type of asthma and finalising a drug regimen that must be followed till the recommended time. Once the asthma is treated, the drugs are gradually tapered and then eventually terminated.
General practitioners are quite capable of determining the distinct types of asthma and treating them accordingly. This is possible only with the patient’s cooperation by revealing their accurate medical history and precise symptoms of the current illness. Regular follow-up with the GP has proven to show adequate health improvement as the treatment plan is modified according to the health status.
What kind of health test is made to diagnose asthma?
Asthma is a chronic health condition that is characterised by the narrowing of the airways due to persistent irritation. Symptoms of asthma include coughing, wheezing chest, shortness of breath, fever, and fatigue. Diagnosing asthma is a step-by-step procedure that includes the patient’s medical history, family history, symptoms evaluation and physical examinations. Even though the mentioned protocols are sufficient to diagnose asthma, health tests are still conducted to exclude the differentials. In the article below, well-designed health tests for the diagnosis of asthma are mentioned.
Spirometry: Spirometry is the standard procedure followed by health professionals to diagnose various lung conditions that include asthma as well. Spirometry involves a device called a spirometer that assesses lung function. The patient is required to attach the mouthpiece to their mouth, take a deep inhalation and then exhale as if emptying their lungs. The device records the values of forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and the ratio of both that is FEV1: FVC. Once recorded, the doctor observes the values and makes the diagnosis accordingly.
Spirometry is a useful technique in diagnosing asthma that examines the capacity of the lung to breathe in and out, obstruction to the airflow (if any) and the extent of damages done to try for reversibility in the treatment plan.
Peak Expiratory Flow Monitoring: Peak Expiratory Flow (PEF) is a parameter to assess the lungs’ sufficient capability and speed of breathing in and out. PEF monitoring involves a portable device called a peak flow meter that is used to measure the speed of exhaled air. The patient is required to deeply inhale air and then blow it out into the mouthpiece of the peak flow meter. The values given by the peak flow meter are recorded at many specific times within a day. These values help with assessing lung function at different hours of the day and help in determining if there is a certain factor that specifically affects lung function during that specific time.
Methacholine Test: The methacholine test, also known as the methacholine challenge test, is an investigation conducted by a health specialist to assess airway obstruction in the lungs.
Methacholine is a drug compound that causes temporary narrowing of the lung airways upon inhalation. The doctor challenges the patient to inhale methacholine several times and wait for its constrictive effects. Lung functions are monitored every time before the further inhalation of methacholine and experiencing further constriction of lung airways.
The patient is monitored carefully by the health expert, as in cases of remarkable loss of lung function, the patient gets breathless which strongly suggests asthma.
Allergy Testing: Allergy testing includes various methods to identify potent allergens such as pet dander, mites, dust, pollen, and certain edibles. It helps in the identification of various routine items and elements that exacerbates the symptoms of lung airway obstruction. Allergy testing includes blood tests to determine immunoglobulin E (IgE) levels upon exposure to what could have caused asthma. Once detected, the doctor enlists certain dos and don’ts for personal safety along with a prescription of antiallergic medication to avoid serious allergy reactions or complications in the future.
Fractional Exhaled Nitric Oxide Test: Fractional Exhaled Nitric Oxide (FeNO) test is used to record the amount of nitric oxide in the patient’s exhaled breath. Nitric oxide is a compound released in breath when there is ongoing inflammation in the lungs. It is a biomarker to diagnose asthma thus elevated levels of nitric oxide help with diagnosis.
Radiography: Radiography is conducted to grossly interpret the lung condition. Asthma is a respiratory condition that affects the airways which is not shown in CT scans or chest X-rays. The purpose of radiography in diagnosing asthma is to rule out other lung conditions such as pneumonia, tuberculosis, or lung fibrosis by looking for consolidations, lesions, shadowing, and opacifications.
The above-mentioned diagnostic tests help with diagnosing asthma by following careful monitoring and evaluation. These tests have the sole purpose to reach an accurate diagnosis and designing a point treatment plan for speedy recovery. It is highly encouraged to visit a healthcare specialist if the symptoms of asthma are experienced. The doctors are trained to advise the much-needed diagnostic test out of the many, based on the patient’s symptoms and health complaints.
Can asthma be prevented?
Yes, asthma is a preventable respiratory condition. Before starting on prevention, it is important to understand asthma, its causative agents and risk factors. Asthma is a common and chronic lung condition that involves narrowing and inflammation in the lung airways. Due to persistent irritation, the patient complaints of coughing, wheezing chest, and difficulty in breathing.
Genetic and environmental factors play a major part in causing asthma. Certain individuals experience increased physical sensitivity to certain environmental triggers, called allergens. Allergens for asthma include dust, mites, pet dander and pollen. These allergens are known to cause local irritation in the lung airways once they are inhaled. Inflammation sets in, causing abnormalities in the airways and shortness of breath.
To date, healthcare experts are trying their best to find a permanent cure for asthma. Doctors advise following prevention strategies to combat asthma instead of relying on long-term medications that include steroid intake as well. In the article below, we discuss prevention strategies and lifestyle adaptations to avoid serious attacks of asthma.
Know the allergens and avoid them: Allergens play a significant role in triggering asthma. Avoiding allergens is the key to avoiding allergic asthma. Commonly known allergens are easy to avoid by minimising the use of carpets as they hold onto a great deal of dust, keeping hairy pets at a safe distance from oneself, cleaning the living place frequently, spraying mites-repellent on the bedding and practising better hygiene. Allergic asthma requires utmost care as a single allergen exacerbates the acute onset of severe asthmatic reaction.
Quit smoking: Cigarettes and tobacco include ingredients that potentially harm the lung airways. These toxic ingredients are frequently found to kickstart inflammation or worsen ongoing inflammation. Both active and passive smokers of cigarettes and tobacco are at risk of developing asthma and compromise their lung health. Quitting smoking is a lifestyle choice towards better health, not only in terms of lungs but the general physical health status as well. Creating a smoke-free environment offers a major contribution towards minimal lung health risks.
Vaccination and Prevention: Vaccination against common respiratory pathogens such as influenza virus helps with immunity boosting and fighting off the infection. Respiratory pathogens compromise lung health which gives an opportunistic chance to the minor inconvenience that later takes its toll on the respiratory functions of the lungs. Vaccination in early childhood against such pathogens significantly contributes towards the prevention of various pulmonary conditions, including asthma.
Encourage Breastfeeding during infancy: Breastmilk includes immunity factors that help the baby fight off infections while their body is still growing. These immunity factors include immunoglobulins for resistance against allergens as well. Infants that rely on breastmilk instead of a milk formula are observed to do much better in health and physical buildup as they rarely fall severely ill. Researchers now prove and educate the masses on the benefits of breastfeeding and its role in the child’s healthy future. Breastfeeding the child must reduce and avoid their chances of falling prey to health conditions that include asthma as well.
Environmental triggers: Air pollutants that are emitted from vehicles, factories, house chimneys, industries and furnaces contain potent irritants. Ozone gas, nitrogen dioxide, sulphur dioxide, toxic smoke and respirable particulate matter from various sources impairs lung health. These pollutants tend to deposit in the lung airways, causing local irritation or blockage in the lungs. Asthma prevention relies on a well-planned government scheme that focuses on the respiratory health of its people. The establishment of industries away from communities, taking a walk around the block instead of going by car, promoting plantation drive, and avoiding going outside when the air seems heavily polluted are useful preventive strategies against environmental triggers of asthma.
Asthma is not entirely preventable as complete reversibility is hard to achieve. The above prevention strategies, however, work for most asthmatics and are found to avoid their chances of experiencing severe asthma attacks. Antiallergy medications are often recommended for patients with asthma only when an allergic reaction due to an unknown allergen is suspected. A major reduction in respiratory illnesses is achievable by creating a healthy environment and adding cleaner air.
Does asthma have a cure?
No, asthma has no cure. A class of medications along with steroids are formulated to ease airway inflammation for symptomatic treatment of asthma. Medical researchers are focusing their best efforts on finding a curative treatment for asthma or expanding to advance the symptomatic treatment.
Asthma is a complex respiratory condition that has multiple influencing factors. Genetic predisposition and environmental triggers affect the onset and course of asthma. Individuals with a family history of increased susceptibility and sensitivity to certain triggers like dust, pollen and mites are prone to be asthmatic. The allergens set in a severe form of allergic reaction that is life-threatening at times. The symptoms of asthmatic reaction include coughing, wheezing and shortness of breath.
While asthma lacks a definitive cure, treatment approaches are still preferred to alleviate the harshness of disease progression. The treatment plan aims to reduce the ongoing inflammation and lower the episodes of possible asthmatic attacks in the future. Treatment of asthma includes bronchodilators that provide short-term but quick relief from an acute asthma attack and corticosteroids that always works in the background to keep the inflammatory mediators at their lowest. These medications are taken on a doctor’s prescription for a limited or extended period, depending on the form and severity of the disease.
We do understand now that there is no definitive cure to asthma and treatment approaches are focusing on relieving the symptoms of asthma only. However, ongoing research and promising advancements made to cure asthma are rays of hope for the future. In the discussion below, we discuss the various advancements in the field of research towards finding a cure for asthma.
Biological therapy is designed to target specific molecules and mediators that have been aiding in inflammation all along. These therapies have shown significant improvement in lowering the exacerbation and severity of disease symptoms. This advancement does not pose a definitive cure, however, further modifications and experimenting in this study anticipate doing much better in the future.
Similarly, genetic therapy has always been working on diseases with familial patterns. Gene therapy to cure asthma believes that if modifications are brought to the DNA level, then asthma must eradicate from the family and terminate passing on to future generations. Gene therapy requires a huge sum of financial investment with unpredictable outcomes thus the success progression is slower in this regard.
Medications that help to alleviate the symptoms of asthma and reduce the inflammatory cascade are tailored according to the individual’s disease condition. People with allergic asthma are capable of altogether avoiding asthma by taking care of their lifestyle such as avoiding allergens and always keeping antiallergic medications with them. Similarly, individuals with seasonal asthma must take anti-asthmatic medications only when it is that time of the year. This proves that the medicinal approach towards treating asthma was made with great care and concern to ensure the safety of the patient. The medical research to treat the symptoms is advancing further forward and focusing on medicinal cures for asthma that everyone affords.
Asthma is a chronic health condition with a complex and unpredictable onset and disease course. There is no cure for asthma to date, but modern technologies and advancements are dependable enough to find the cure for asthma through them.
Can you train asthma away?
No, you cannot train asthma away. Asthma is a complex and chronic respiratory health condition with no cure yet. This does not mean that people with asthma have a high morbidity and mortality rate. The symptoms and disease pattern of asthma are possible to control by adapting to daily life modifications to lower the exacerbation of the disease, authorise the symptoms and minimise its disturbing effects on daily tasks.
Medical guidelines and statements from well-reputed health organisations such as the National Institute of Health (NIH) and the Global Initiative for Asthma (GINA) establish that asthma is a chronic respiratory illness that requires long-term or even lifetime treatment. The importance of sticking to medical treatment, avoiding the allergens that trigger asthma and potentiating their symptoms and regular medical checkups is evident from the positive outcomes.
Medical treatment of asthma includes corticosteroids and inhaled bronchodilators. Bronchodilators act on the lung airways to make room for breathing in acute asthma attacks. Bronchodilators are efficient and used to provide temporary relief at times of asthma attack distress and breathlessness. Corticosteroids, on the other hand, belong to the class of steroid medications that work on inflammatory mediators and inhibit them. Corticosteroids play the role of controller medications in the treatment of asthma which means that they act to avoid the emergence of inflammation in the airways and resultant airway constriction. Regular intake of prescribed medications for asthma is bound to show improvement in health and quality of life.
Regular exercise and achieving physical fitness are important for general health. Physical exercise increases the efficiency of the cardiovascular system, improves lung functions, and strengthens respiratory muscles. These positive effects increase lung capacity as well as mediate breathing. Doctors advise patients with well-controlled asthma to take part in activities that lead to physical fitness as it strengthens the respiratory system. Patients with uncontrolled, severe or exercise-induced asthma need supervision and proper consultation with a healthcare expert before going in for intense exercises and cardio.
Breathing Exercises to Navigate Asthma:
Breathing exercises do not treat or alleviate asthma, they are effective in providing symptomatic relief while experiencing acute asthma. in the discussion below, we discuss a few effective breathing exercises that help to an extent with asthma. Breathing exercises training to shoo away acute asthma include diaphragmatic breathing, pursed lips breathing and Buteyko breathing.
Diaphragmatic Breathing, also known as belly breathing, is a breathing technique that focuses on the diaphragm muscle. Diaphragmatic breathing includes the diaphragm muscle in respiration instead of the usual chest muscles. This muscle is located below the lungs and above the stomach which helps with respiration. This breathing technique aims to reduce chest tightness and mediate breathing during an asthma attack by putting an accessory muscle to work to provide temporary symptomatic relief.
Diaphragmatic breathing is easy to practice. Find a quiet place to sit or lie down. Place one hand on top of the belly and breath in while remaining conscious of keeping the chest still. Hold the breath in for a while and then exhale while the abdominal muscles are in a contracted state. Regular practising the diaphragmatic breathing technique is conducive to improving symptoms of asthma.
Pursed Lips Breathing is an effective technique to help with breathing, especially during episodes of shortness of breath. The principle of this technique is to prolong the exhalation than inhalation by two times. Prolonged exhalation causes relaxation that is of significance during chest tightness and breathlessness experienced with asthma attacks.
The professionals suggest patients practice purse lip breathing by sitting in a comfortable space and relaxing their tense shoulders. Take a deep breath in through the nose and count to two. Hold your breath in for a while. Next, pucker the lips as if intending to blow into a balloon, and exhale slowly while counting to four.
This breathing technique is easy to perform anywhere, be it at rest or in a stressful state of asthmatic attack. Regular practice is bound to bring out positive results and improve the relaxation of chest muscles.
Buteyko Breathing works on the principle of reducing hyperventilation, which is a causative factor of asthma. This breathing technique is just like normal breathing, except for the variations in durations and intervals between each breath.
The Buteyko breathing technique focuses on normalising the pattern of breathing, increasing the concentration of carbon dioxide in the blood, and improving lung functions. This technique also requires the patient to stay relaxed and find a comfortable spot to practice breathing.
To practice Buteyko breathing, take a gentle diaphragmatic inhalation through the nose. Then, exhale completely through the nose. Take a break, not a breath, for a while and mildly increase the body’s drive to get that air. Now, take another diaphragmatic inhalation through the nose and exhale through the same path. This increases air hunger and reduces hyperventilation while the patient is in charge. Apart from asthma, doctors recommend Buteyko breathing for patients with panic disorders that experience hyperventilation in distressing situations.
Breathing exercises to strengthen respiratory muscles and increase lung capacity is a routine adaptation. Individuals who practice breathing tend to manage asthmatic attacks in a better way and control their symptoms until the medications start to work for them. It is however important to understand that breathing exercises must not replace the medical treatment of asthma. medicine intake on doctor’s prescription and breathing exercise goes hand in hand to treat asthma and improve the quality of everyday life.
Conclusion:
Asthma is a chronic respiratory condition affecting people of all ages, causing inflammation and muscle strain. It can be classified into various forms, including allergic asthma, aspirin-induced asthma, cough-variant asthma, exercise-induced asthma, nighttime asthma, steroid-resistant asthma, and occupational asthma. Allergic asthma is the most prevalent form.
Asthma is a common chronic condition affecting around 1 in 13 people in the UK, with common types including allergic asthma, adult-onset asthma, childhood asthma, and adult-onset asthma in the country. The most severe type is Status asthmaticus, a state of respiratory failure associated with severe acute asthma.
Treatment modalities include symptom manifestation, nocturnal awakenings, respiratory difficulties, and emergency room visits. The most severe age for asthma in children and adolescents, with a prevalence rate of approximately 7.7%.
Treatment for allergic asthma involves avoiding allergens, closing windows, and using air conditioners and dehumidifiers. Severe asthma is a chronic, long-term disease affecting daily routines, employment, and social life. Treatment for occupational asthma focuses on preventing and managing episodes, using inhaled steroids, multipurpose inhalers, immediate relief medications, mast cell stabilisers, and immunotherapy. Non-allergic asthma is caused by dry or chilly air, humidity, heat, air toxicity, smoke, fumes, chemicals, fragrances, stress, anxiety, challenging exercise, viruses, or respiratory illnesses. Steroid-resistant asthma is resistant to treatment, while airway constrictions, swelling, and mucus buildup cause aspirin-induced asthma. Treatment options include steroids, long-term control medications, and quick-relief therapies.
Asthma manifests at any stage of life, and many individuals encounter their initial asthma symptoms during adulthood. The prevalence of asthma among adults is significant, and accurate diagnosis and effective management strategies are crucial for mitigating potential complications and promoting a high standard of living among individuals with asthma. Common medications for asthma include preventive medications, long-term control medications, quick-relief medications, and short-acting beta-agonists. A stepwise approach to treatment is recommended, with a doctor modifying treatment based on symptoms. An asthma action plan should be established, including medication administration timing, triggers, and regular monitoring.
Asthma is a treatable respiratory condition but not curable. Researchers now aim to focus more on the treating options and design target medications that act on distinct mediators of asthma progression. Practicing various breathing techniques, improving hygiene, cleaning the living area regularly and avoiding potent allergens is found to significantly improve the quality of life in asthmatics.



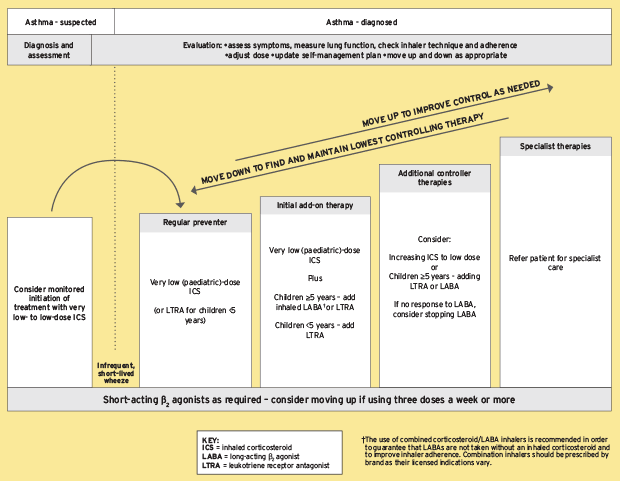






 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews