Cough-Variant Asthma: Causes, Symptoms, Risk Factors, Diagnosis, and Treatment


Related products
Cough-Variant Asthma Overview
Cough-variant asthma (CVA) primarily manifests as a persistent cough as its main symptom, making it different from classic asthma, which often presents with wheezing and breathlessness.
One of the most frequent causes of chronic cough, which is a cough that lasts longer than 6–8 weeks, is cough-variant asthma, as explained by Dr Sabrina Felson, MD board-certified in internal medicine. Asthma coughing happens both day and night. Sleep disruptions may occur if you have night-time asthma. Exercise-induced asthma, which is common in those with the cough-variant of asthma, causes coughing to get worse. When they are exposed to asthma triggers, allergy-inducing items like dust or potent smells, or when they are in cold air, coughing gets worse.
Anyone develop cough-variant asthma at any time, although young children with childhood asthma are more likely to do so. The "classic" form of asthma, characterised by wheezing and shortness of breath, results from cough-variant asthma.
Nobody fully understands the underlying causes of cough-variant asthma, just as "classic" or "typical" asthma. However, people begin coughing after being exposed to allergens or when inhaling cold air. An upper respiratory infection is accompanied by coughing. For instance, it's common to have asthma and sinusitis.
Additionally, cough-variant asthma is more likely to be the cause of a cough that appears after a person starts using beta-blockers. Beta-blockers are medications that are used to treat a variety of illnesses, including high blood pressure, cardiac disease, heart failure, migraines, and palpitations. Additionally, glaucoma and other eye conditions are treated using beta-blockers in eye drops. These eye drops may trigger coughing attacks and other asthmatic symptoms.
Asthma is characterised by inflammation, which is most prominent in CVA and makes the bronchial passages hyperresponsive. Coughing results from the airways' increased sensitivity to triggers and irritants.
The symptoms of asthma, including CVA, are frequently brought on by allergens. Common allergens that aggravate coughing in people with CVA include dust mites, pollen, pet dander, and mould.
Colds and other viral respiratory infections make CVA symptoms worse. Infections worsen the inflammation in the airways, which makes coughing more frequent.
CVA sufferers occasionally cough, particularly at night or in response to stimuli like cold air, exercise, or respiratory illnesses. Without a good assessment, it is difficult to diagnose this cough because it lasts for weeks or even months. Subtle indications of airway inflammation, such as a slight tightness in the chest or sporadic shortness of breath, are present in some CVA patients.
It's important to recognise these symptoms because, if left untreated, CVA eventually result in the emergence of symptoms which are comparable to those of asthma. For this reason, prompt diagnosis and treatment are key. Consult a healthcare provider for an accurate assessment and recommendations if you experience CVA symptoms or prolonged coughing.
When diagnosing cough variant asthma (CVA), it is necessary to thoroughly examine a persistent cough that may not be accompanied by the typical wheezing or breathlessness that characterises traditional asthma. Healthcare professionals frequently take a CVA into consideration as a possible underlying cause when a patient appears with a chronic cough lasting eight weeks or more. In order to rule out other potential reasons for the cough, such as postnasal drip, gastroesophageal reflux disease (GERD), or chronic bronchitis, the diagnostic process normally starts with a thorough medical history and physical examination.
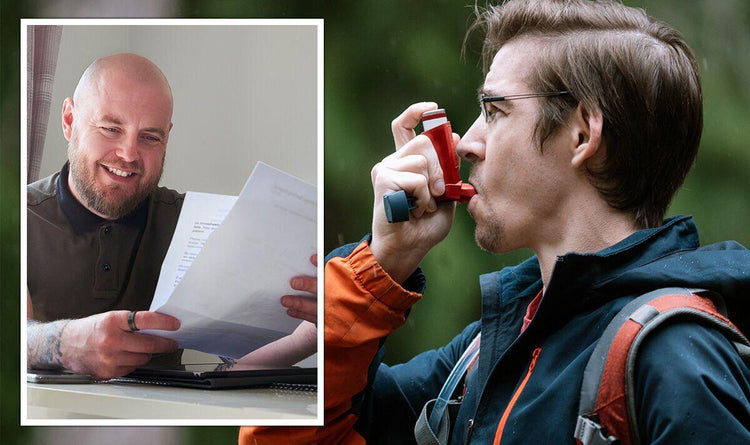
Physicians perform pulmonary function testing, notably spirometry and bronchoprovocation studies, to confirm a CVA diagnosis. Inhaling chemicals like methacholine during bronchoprovocation testing assesses airway responsiveness whereas spirometry measures lung function and reveals airflow limitation. When these tests reveal bronchial hyperresponsiveness and the cough subsides upon using asthma drugs like inhaled corticosteroids or bronchodilators, cough variant asthma is diagnosed. Once symptoms are under control, effective care and treatment are started to enhance the patient's quality of life.
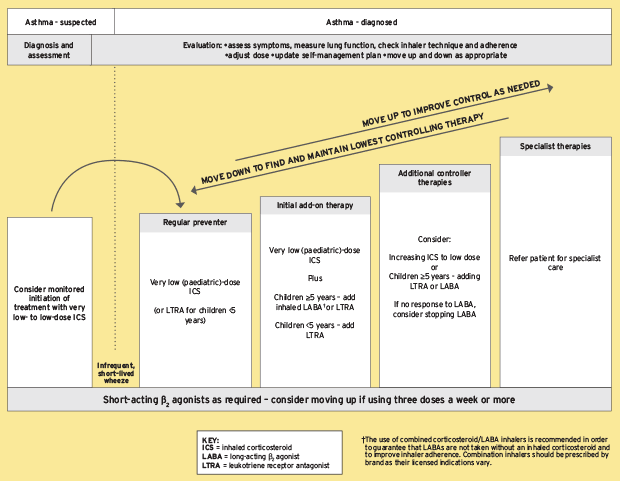
Inhaled corticosteroids (ICS), such as beclomethasone or fluticasone, are a mainstay of CVA treatment. These drugs aid in reducing the airway inflammation that is a key component of asthma. Even when wheezing or shortness are not obvious, ICS can successfully treat this inflammation and reduce the coughing brought on by CVA. Typically, these drugs are delivered directly to the affected airway via a metered-dose inhaler or a dry powder inhaler.
In addition to ICS, bronchodilators are another essential component of CVA management. Albuterol and other short-acting beta-agonists (SABA) reduce coughing and improve airflow by calming the muscles that surround the airways. When someone has a severe coughing attack, these drugs are frequently utilised as rescue inhalers. For people with more severe CVA, long-acting beta-agonists (LABA) are taken alongside ICS in order to provide long-lasting relief and minimise symptom exacerbations.
Leukotriene modifiers, like montelukast, are included in the therapy plan for people who have chronic or resistant symptoms. These drugs aid in the blocking of leukotrienes' actions, which further lessens airway inflammation and coughing. Leukotrienes are inflammatory chemicals that contribute to asthma.
What is cough variant asthma?
Cough variant asthma (CVA) is a unique and often misunderstood variant of asthma, characterized by a persistent cough as its primary symptom, rather than the classic wheezing and shortness of breath commonly associated with asthma. The diagnosis of this ailment can be difficult, and it has a big effect on the way someone lives. In this comprehensive review, we'll look into the key elements of cough variant asthma, such as its clinical manifestation, diagnosis, course of treatment, and management techniques.
Due to its unusual symptoms, cough variant asthma poses a diagnostic challenge. Contrary to conventional asthma, where wheezing and shortness of breath are the most prominent symptoms, CVA is largely distinguished by a persistent, non-productive cough. It is challenging for both patients and medical professionals to connect this persistent cough to an asthma issue because it is dry or comes with little mucus production. The cough is brought on by a number of things, such as cold air, exercise, allergies, respiratory illnesses, and exposure to irritants. It is frequently worse at night or in the morning.
The absence of obvious respiratory distress is a defining characteristic of CVA. Asthma symptoms such as wheezing or laboured breathing are not present in patients with CVA, which results in a delayed or incorrect diagnosis. The more well-known symptoms of wheezing and shortness of breath develop from CVA into conventional asthma if it is not treated, though.
A thorough evaluation that considers the patient's medical history, clinical presentation, and objective testing is necessary to make the diagnosis of cough variant asthma. The healthcare professional will question about the frequency, duration, and causes of the cough as part of a full medical history. Any family history of allergies or asthma is pertinent.
Objective testing is necessary to confirm the diagnosis and eliminate further probable causes of chronic cough, such as postnasal drip, gastroesophageal reflux disease (GERD), or chronic obstructive pulmonary disease (COPD). Spirometry and bronchoprovocation testing are two examples of pulmonary function tests (PFTs), which are often used. Bronchoprovocation testing involves inhaling agents that cause airways to constrict in order to gauge the airway's reactivity, while spirometry evaluates the lung's capacity and airflow.
The methacholine challenge test is yet another helpful tool for identifying CVA. Methacholine, a chemical that causes bronchoconstriction in those with sensitive airways, is inhaled by the patient during this test in increasing quantities. The test reveals airway hyperresponsiveness, a defining feature of asthma if the patient experiences a severe reduction in lung function.
In order to identify which allergens specifically are responsible for the cough, allergy testing is advised. The identification of probable triggers is aided by skin prick tests or blood tests for IgE antibodies specific to allergens.
A proper treatment regimen must be started as soon as a diagnosis of cough variant asthma is made. In order to improve the patient's quality of life, the treatment aims to control the patient's asthma and reduce their persistent cough.
Inhaled Corticosteroids (ICS) are the cornerstone of asthma treatment because they help manage symptoms and minimise airway inflammation. Low to moderate dosages of ICS, either using a dry powder inhaler or a metered-dose inhaler, are frequently successful in controlling the chronic cough in CVA.
Cough variant asthma sufferers lead normal lives and have an excellent quality of life with proper care. It is critical to note that CVA occasionally develops into classic asthma, necessitating long-term therapy and monitoring. In order to prevent attacks and keep asthma under control, regular checkups and adherence to the recommended treatment plan are essential.
Lifestyle modifications help improve results for any chronic condition. The likelihood of asthma flare-ups is decreased by leading a healthy lifestyle that includes frequent exercise, a nutritious diet, and stress management.
For efficient management of CVA and to stop the development of typical asthma, proper patient education, constant monitoring, and adherence to the treatment plan are essential. Even though cough variant asthma presents special obstacles, those who have it live happy, healthy lives with the correct approach and support.
Who is commonly affected by cough-variant Asthma?
While cough-variant asthma can affect people of all ages and socioeconomic backgrounds, it tends to impact some groups more frequently. It is typically observed in children, especially those who have a family history of allergies or asthma. Adults also acquire cough-variant asthma, particularly those who have a history of allergies. Additionally, people who are exposed to environmental triggers such as pollution, allergens, or respiratory illnesses are at a higher risk.
Research studies and clinical observations have shown that CVA is indeed common in children, though the exact prevalence can vary. Some studies estimate that up to 30% of children with chronic cough may have underlying CVA. These numbers highlight the importance of considering CVA as a potential diagnosis when evaluating a child with a persistent cough.
Asthma, in general, tends to manifest early in life, which is one reason CVA is frequent in children. Asthma symptoms typically appear in infants and young children during the first few years of life, and CVA is no exception. When a child develops a chronic cough, it is crucial for parents and other adults to be aware of the risk of CVA, especially if asthma or allergy diseases run in the family.
Children have a wide range of CVA triggers, but common ones include respiratory illnesses, allergies, exertion, or contact with irritants. These triggers worsen the airway inflammation that already exists, and a persistent cough emerges as the main symptom.
The prevalence of CVA is typically lower than that of conventional asthma in adults. According to some research, between 30% and 40% of persons with a persistent cough have CVA, though this number varies. According to other estimates, CVA is the cause of 10% to 40% of all adult cases of chronic cough. These variations reflect the challenges in accurately determining the frequency of CVA due to changes in study populations and diagnostic criteria.
How does cough variant asthma differ from other types of Asthma?
Cough variant asthma (CVA) is a subtype of asthma that distinguishes itself primarily through its predominant symptom – chronic coughing. While CVA and other types of asthma, such as allergic asthma and exercise-induced asthma, have certain similarities, they differ significantly in terms of their clinical presentations, diagnostic standards, and therapeutic strategies. For patients and healthcare professionals to effectively manage and treat this particular asthma different kinds, they must be aware of these differences.
It's critical to first recognise the similarities between cough variant asthma and other types of asthma before understanding the differences. All types of asthma are characterised by airway inflammation, which causes symptoms like wheezing, shortness of breath, and tightness in the chest. CVA deviates from the norm, though, in that its main symptom is an unceasing, continuous cough. This cough differs from the common cough associated with asthma in that it frequently produces no mucus or phlegm.
The diagnostic criteria for CVA represent yet another significant distinction. Clinical symptoms, pulmonary function testing, and bronchial provocation tests are typically used to diagnose asthma. Contrarily, CVA is not presented with the typical asthma symptoms, such as wheezing or shortness of breath, making a diagnosis more difficult. Instead, the key diagnostic criterion that must be used by healthcare professionals is the cough's chronic character, which frequently lasts eight weeks or longer. The underdiagnosis and undertreatment of CVA may result from this delay in diagnosis.
Additionally, compared to other types of asthma, cough variant asthma has different causes. While certain asthma types are made worse by allergens or exercise, CVA frequently seems to be brought on by less obvious triggers such as respiratory infections, cold air, or irritants like smoke and strong odours. It is difficult to correctly diagnose and treat the disorder due to the wide range of triggers.
There are significant differences between CVA and other kinds of asthma in terms of treatment. Although inhaled corticosteroids (ICS) are essential for managing asthma, CVA patients do not respond as well to these drugs because coughing is more common in these patients than airway constriction. Alternative therapies are more effective, such as non-steroidal anti-inflammatory medications (NSAIDs) to treat airway inflammation or short-acting beta-agonists (SABAs) to reduce coughing fits.
As part of managing CVA, it is necessary to address the underlying causes and coexisting illnesses that contribute to chronic cough. This strategy involves treating disorders like gastroesophageal reflux disease (GERD), which is frequently linked to CVA, or actively treating allergies.
It is crucial to understand these variations because failing to diagnose or treat cough variant asthma inappropriately causes patients to endure unnecessarily long periods of suffering. As a result, when a patient complains of persistent coughing, healthcare professionals must be alert in keeping CVA as a potential diagnosis in mind.
In conclusion, cough variant asthma is a distinct subtype of asthma that stands out due to its major symptom of chronic coughing, which is distinct from the traditional wheezing and shortness of breath associated with asthma. The persistence of this cough, which distinguishes CVA from other types of asthma, is important to the diagnostic criteria for the condition. When compared to conventional asthma management, CVA management includes non-standard procedures and has different triggers. For healthcare practitioners to correctly diagnose and treat CVA and provide an enhanced quality of life for those affected, it is crucial to be aware of these variances.
What are the causes of cough variant asthma?
Researchers have found a number of factors that lead to the development of cough variant asthma, despite the fact that the exact causes are not entirely known. These factors interact intricately and have multiple sources, including both genetic predisposition and environmental triggers.
Genetic susceptibility is one of the primary causes of cough variant asthma. People who have a family history of asthma or other allergy diseases are more likely to develop CVA. Researchers are still learning about the complex genetic pathways causing CVA. Numerous genes have been linked to an increased risk of developing asthma. Some people are more likely to develop cough variant asthma due to genetic characteristics that affect how the airways react to allergens and irritants.
Another important component influencing cough variant asthma is airway hyperresponsiveness, which is a characteristic of asthma. This phenomenon describes the airways' excessive broncho constrictive response to numerous stimuli. Even insignificant triggers like cold air, smoke, or potent odours might cause coughing spasms in people with CVA. The persistent inflammation that characterises asthma and is brought on by a variety of things, such as infections, allergens, and irritants, is thought to be the cause of the airways' increased sensitivity.
Cough-variant asthma is caused by GERD, a condition where stomach acid rushes back into the oesophagus. The bronchial tubes become irritated and inflamed as a result of the acidic contents that reflux into the throat and airways, which cause coughing. This link between GERD and CVA emphasises how intricately the digestive and respiratory systems interact with those who have asthma symptoms.
Stress and worry are two psychological elements that make cough-variant asthma symptoms worse. Stress causes the release of stress hormones, which may enhance airway hyperresponsiveness and inflammation, intensifying coughing. Furthermore, anxiety-related hyperventilation causes coughing fits in people with CVA.
Other common causes of Cough variant asthma are as follows:
1. Sinusitis
Asthma and sinusitis are two prevalent respiratory illnesses that can have a complicated and interconnected relationship. Despite being separate medical entities, their link has recently drawn more attention.
The link between sinusitis and cough variant asthma begins with inflammation. In reaction to allergens or irritants, sinusitis, an infection of the paranasal sinuses, can trigger the release of inflammatory mediators such as histamines and leukotrienes. These mediators have the power to start an inflammatory cascade in the respiratory system that affects the lower airways. This inflammatory process is thought to be crucial in the emergence of cough variant asthma.
The lower airway, which is made up of the trachea and bronchial tubes, is physically and functionally related to the upper airway, which includes the nasal passages and sinuses. Increased cough sensitivity and reactivity result from inflammation and mucus production in the upper airways, which set off a reflex response in the lower airways. This phenomenon, known as the "nasobronchial reflex," contributes to the persistent dry cough characteristic of CVA.
Cough and nasal congestion are overlapping symptoms between sinusitis and CVA. This symptom overlap might make a diagnosis difficult since doctors initially treat sinusitis without taking into account the likelihood of an underlying asthma component. As a result, CVA goes untreated or is incorrectly identified as chronic rhinosinusitis.
Bronchoprovocation tests and spirometry are frequently used to diagnose cough variant asthma. However, in some people with CVA, these tests produce normal results, thus confusing the diagnosis procedure. When examining patients with a chronic cough, particularly when sinusitis is also present, doctors must keep a high level of suspicion in mind.
In order to address the connection between sinusitis and cough variant asthma, managing sinusitis is a crucial step. It is possible to be prescribed antibiotics and nasal corticosteroids to treat sinus inflammation and congestion. The inflammation of the upper airways that contributes to the symptoms of CVA is reduced by treating sinusitis.
Patients with sinusitis and cough-variant asthma may benefit in two different ways from the use of nasal corticosteroids. These drugs aid in reducing nasal swelling and inflammation and may also have anti-inflammatory effects in the lower airways, aiding in the management of asthma.
2. Exercise
One significant factor in the development of CVA is exercise. While exercise is crucial for overall health and well-being, its relationship with CVA is complex. Exercise is frequently linked to many health advantages, such as increased respiratory function, better weight control, and increased cardiovascular fitness. However, Exercise is a double-edged sword for people with CVA. On the one hand, regular exercise sometimes lessens the symptoms of asthma while enhancing general lung health. On the other side, for those with CVA, exercise makes them cough and makes their symptoms worse. The key lies in understanding the mechanisms by which exercise influences airway function and how these mechanisms are implicated in the development and management of CVA.
Exercise-induced bronchospasm (EIB), also referred to as exercise-induced bronchoconstriction (EIB), is a well-researched phenomenon in which physical effort causes a temporary narrowing of the airways. This condition is not unique to CVA but is experienced by a significant number of individuals, including those without asthma. In individuals with CVA, the response to exercise is particularly pronounced.
Increased breathing rates and volumes during exercise expose the airways to cooler, dryer air, which irritates the airways and causes bronchoconstriction. Furthermore, the inflammation and constriction of the airways in people with CVA are aggravated by the release of different mediators during exercise, such as histamine and leukotrienes. Exercise thus causes the characteristic coughing episodes that are common in CVA patients.
Some people experience the onset of CVA as a result of exercise only. Exercise-induced cough variant asthma (CVA) is a condition that develops in previously asymptomatic people which is a direct result of physical activity. It is thought that repeated exposure to exercise-induced bronchoconstriction causes chronic airway inflammation and hyperresponsiveness, which ultimately results in CVA. The precise mechanisms driving this transition are not yet fully known.
Environmental factors also have an impact on exercise-induced CVA. For instance, people who exercise in cold, dry climates or in places with high levels of air pollution are more likely to experience CVA that is brought on by exercise. These external factors amplify the broncho constrictive effects of exercise and aid in the growth of CVA.
The main symptom, coughing, is frequently not connected to the patient's physical activity, which makes the diagnosis of exercise-induced CVA problematic. Exercise challenge tests are used by clinicians as a diagnostic tool. The purpose of these examinations is to measure lung function while asking subjects to perform controlled activity. It is a symptom of exercise-induced CVA when there is a considerable decline in lung function after exercise.
Combining pharmaceutical and non-pharmacological strategies is required to manage exercise-induced CVA. Albuterol and other short-acting bronchodilators ease discomfort by loosening the muscles that contract the airways and lowering bronchoconstriction. For long-term management of airway inflammation, inhaled corticosteroids are recommended. Avoiding surroundings that are uncomfortable for exercise, such as cold and dry ones, and using a scarf or mask to warm and humidify the air that is inhaled to help reduce symptoms.
Although exercise sometimes causes CVA in some people, it is an effective treatment for the illness. Regular exercise is linked to increased lung and cardiovascular health as well as overall better health. Exercise helps people with CVA improve their quality of life and lessen the number of coughing fits.
For those with CVA, not all types of exercise are made equal. While some activities are more likely to cause symptoms, others are easier to handle. For people with CVA, low-impact activities like swimming and cycling are preferred because they expose you to less cold and dry air. Additionally, breathing-focused exercises like yoga and tai chi aid with symptom management and respiratory function.
3. Outdoor Allergens
Outdoor allergens include a variety of things, such as pollen, mould spores, dust mites, and animal dander. These allergens are all around us, and when exposed, they cause symptoms in people who are allergic to them. Among these allergens, pollen from weeds, grasses, and trees is a particularly significant cause of CVA. Different pollens predominate in the external environment depending on the area and season.
One of the most prevalent outdoor allergens linked to the development of CVA is pollen. Pollen grains can cause inflammation and excessive mucus formation in the airways when inhaled by those who are vulnerable to it. This irritation of the airway linings causes recurrent dry cough which is a defining feature of CVA. The peak CVA exacerbations sometimes coincide with specific seasons when pollen counts are typically at their highest, such as spring and autumn.
Mould spores are yet another outdoor allergen that exacerbates CVA. Outside, moist conditions like heaps of leaves or decaying vegetation encourage the growth of mould. These spores cause respiratory problems if they are inhaled after they become airborne. Mould spore exposure aggravates a CVA patient's cough and causes symptoms similar to asthma.
Dust mites are normally found indoors, but they are found outside, particularly in places with high humidity levels. When inhaled, the allergenic proteins produced by these tiny organisms cause coughing and worsen CVA symptoms.
Exposure to outdoor allergens such as animal dander from cats, dogs, or other animals might act as a trigger for some people with CVA. Sensitive people have coughing fits or aggravation of their CVA symptoms when exposed to pet owners' allergen-filled fur or dander in outdoor places.
In the development of CVA, the immune system is crucial. Inhaling allergens triggers the immune system to identify them as foreign invaders, which causes the release of inflammatory chemicals including histamines and leukotrienes. Coughing and other respiratory symptoms are brought on by these chemicals' inflammation and constriction of the airways.
People who have CVA frequently have hyperreactive airways, which makes them more susceptible to environmental triggers. Even in small quantities, outdoor allergens cause airways to react excessively, resulting in chronic coughing.
Airway linings become inflamed and irritated when exposed to outdoor irritants.
4. Weather conditions
Human health is significantly impacted by weather, and this impact includes respiratory diseases like asthma. One important weather-related aspect that has a big impact on people with CVA is temperature. Many patients, including those with CVA, experience their asthma symptoms as a result of exposure to cold air. Coughing and other asthma-related symptoms occur when cold air enters the respiratory system because it narrows and inflames the airways. This effect is especially noticeable in those with CVA because coughing is their main symptom. Thus, exposure to low temperatures, especially during the winter, might result in coughing episodes that are more frequent and severe.
On the other hand, those who have CVA usually perform better in warm, humid weather. The chance of inflammation is decreased by keeping the airways moist due to the greater humidity levels. Warmer temperatures may also lessen the chance of bronchoconstriction and airway irritation, helping CVA patients. As a result, people with CVA typically discover that their symptoms are less irritating in the summertime when the temperature is warmer and more humid.
The onset and escalation of CVA symptoms are strongly influenced by humidity. The respiratory mucosa gets dehydrated in low-humidity environments, which are prevalent in desert regions or in the winter. In people with CVA, this dryness enhances airway sensitivity and increases the incidence of coughing fits. Higher humidity, on the other hand, supports keeping the moisture in the airways, which lessens irritation and coughing.
Furthermore, the presence of allergens in the environment is impacted by humidity levels. Mould and dust mites, which are frequent allergens that exacerbate asthma symptoms, grow more readily in environments with high humidity. Therefore, those who have CVA have exacerbated symptoms in humid environments, particularly if they are sensitive to these allergens. On the other hand, allergy exposure decreased in dry and low-humidity environments, which resulted in a reduction in CVA symptoms.
A major issue for people with CVA is air pollution, which is impacted by weather conditions. Air pollutants including ozone, nitrogen dioxide, and particulate matter (PM), as well as their dispersion and concentration, are affected by weather patterns. Individuals with CVA are not exempt from the effects of high air pollution levels on asthma symptoms.
Lack of air circulation and stagnant weather conditions cause pollutants to gather up close to the ground, resulting in poor air quality. Temperature inversions, where a layer of warm air holds colder air near the surface and prevents pollutants from dispersing, make such circumstances worse. These circumstances lead to an increase in the amount of asthma triggers in the air, which causes coughing and other CVA symptoms.
On the other hand, windy conditions spread allergens and toxins, potentially lowering the likelihood of asthma attacks in those with CVA. However, windy weather has the ability to spread allergens across greater distances, exposing people to triggers they might not otherwise be exposed to. Consequently, even though wind helps disperse pollutants, it also presents additional difficulties for people with CVA.
Weather patterns have a key role in the development of seasonal allergies, which are frequently brought on by grass, weed, and tree pollen. People who are susceptible to pollen may experience worsening CVA symptoms as a result of these allergies. Climate factors like temperature and precipitation have an impact on when and how strongly pollen seasons occur.
Longer exposure to allergens for people with CVA results from earlier and longer pollen seasons, which are brought on by warmer temperatures. On the other hand, a lot of rain temporarily relieves CVA and pollen allergies by clearing the air of pollen.
In conclusion, People with cough variant asthma have to deal with the effects of the weather on a daily basis. The frequency and intensity of coughing episodes in these people are affected by temperature, humidity, air pollution, and allergen concentrations. The quality of life for persons who live with CVA must be improved by identifying these weather-related triggers and implementing suitable management techniques. People with CVA better manage their disease and experience a higher degree of symptom control throughout the year by staying informed and taking proactive measures to lessen the impacts of inclement weather.
5. Certain medications
ACE inhibitors, a class of drugs frequently administered for hypertension and heart failure, have been directly linked to the emergence of cough-variant asthma. ACE inhibitors are typically well tolerated, but sometimes they cause persistent cough which is a bothersome side effect. Bradykinin build-up in the airways, which is a chemical that induces vasodilation and inflammation, is likely to be the origin of this cough in people. Healthcare practitioners must take alternative antihypertensive drugs into account when a patient complains of a persistent cough while using ACE inhibitors because this inflammation causes CVA symptoms.
Another group of medications with a reputation for exacerbating CVA symptoms in certain people are beta-blockers. These medications are prescribed for various cardiovascular conditions and potentially worsen asthma-related symptoms by blocking the effects of beta-adrenergic agonists, which help relax the airway smooth muscles. Beta-blockers cause bronchoconstriction, a worsening cough, and other respiratory symptoms in people who are predisposed to asthma or CVA. When considering beta-blockers for those with asthma or a history of CVA, healthcare professionals must carefully weigh the risks and benefits.
Non-steroidal anti-inflammatory medications (NSAIDs) are frequently used to treat pain and inflammation. Aspirin and ibuprofen are two NSAIDs that have been linked to causing or worsening cough variant asthma in people who are vulnerable. Patients with a history of asthma and nasal polyps are most likely to experience this condition, which is also known as aspirin-exacerbated respiratory disease (AERD). Although the exact causes of NSAID-induced CVA are unclear, it is believed that deregulation of pro-inflammatory pathways and the generation of leukotrienes, which cause bronchoconstriction and cough, are involved. Healthcare professionals must be cautious when giving NSAIDs to patients who have a history of asthma or CVA and look into non-pharmacological pain relief options.
Statins, which are frequently administered to treat excessive cholesterol, have occasionally been linked to the emergence of CVA. A small percentage of people suffer a persistent cough as a side effect of statin therapy, even though the connection between statins and CVA is less certain than with other drugs. Although the exact mechanisms underlying this relationship are not fully known, it is thought that inflammation and oxidative stress in the airways have a role.
6. Indoor Allergens
Indoor allergens are substances that are present in indoor environments, such as homes, workplaces, and educational facilities, and cause allergic reactions in those who are vulnerable. The most typical indoor allergens are dust mites, pet dander, mould spores, cockroach droppings, and indoor air pollutants like cigarette smoke. These allergens contaminate indoor areas and constitute a major factor in a number of respiratory disorders, including CVA.
Inducing inflammation of the airways is one of the main ways that indoor allergens cause CVA. An asthmatic individual's immune system may interpret indoor allergens as dangerous when they are exposed to that person. This causes the airways to become inflamed, which attracts immune cells, releases cytokines, and produces inflammatory mediators.
This inflammation mostly impacts the bronchial airways in CVA. Chronic contact with indoor allergens can result in lingering airway inflammation, which then causes the defining symptom of CVA, chronic cough. The cough acts as a defence mechanism to clear the airways of mucus that has been induced by allergens and other irritants.
Can air pollution cause cough variant Asthma?
Yes, Air pollution is a growing concern worldwide due to its detrimental effects on human health. Among the various health issues associated with air pollution, one particularly concerning condition is cough variant asthma (CVA).
The respiratory system may be significantly impacted by air pollution, which is a complex mixture of particulate matter (PM), gases, and chemical substances. Common pollutants include ground-level ozone, nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), and fine particulate matter (PM2.5).
These pollutants are emitted into the atmosphere through a number of different processes, including industrial processes, wildfires, and vehicle emissions.
A variety of negative respiratory symptoms, such as bronchitis, worsened asthma, impaired lung function, and an increased risk of respiratory infections, are linked to air pollution exposure. Asthma is one of these side effects that deserves special attention because it causes persistent airway inflammation, which is also the mechanism behind the cough variety of asthma.
Inflammation of the airway lining is caused directly by air pollution, especially PM2.5 and other tiny particles. Eosinophils, which have a role in asthma and CVA, are inflammatory mediators that are released in response to this inflammation.
Oxidative stress in the respiratory system is brought on by air pollution. Airway inflammation and hyperresponsiveness—essential characteristics of CVA—are caused by this stress, which upsets the equilibrium between antioxidants and free radicals.
Long-term exposure to air pollution can impair the immune system's normal operation, making people more prone to respiratory illnesses like CVA. In the airways, this imbalance may cause an excessive immunological response.
People with CVA are more likely to develop coughing fits when exposed to polluted air because air pollution may interact synergistically with other asthma triggers such as allergens, respiratory illnesses, and cold air.
Are there any foods that might trigger cough variant asthma?
Yes, there are food that trigger cough variant asthma. One of the primary food triggers for CVA is allergenic foods. Allergens to nuts, shellfish, eggs, dairy products, soy, and wheat are among the most prevalent. Exposure to certain allergens causes an immunological reaction in those who are vulnerable, which results in symptoms like a chronic cough. Allergen avoidance is essential for treating CVA brought on by food allergies. In order to discover specific food allergies through testing, such as skin prick tests or blood tests, people with CVA must work together with allergists or immunologists. Once these allergens have been identified, they must be removed from the diet.
Another group of substances that increase CVA symptoms is acidic foods and drinks. Citrus fruits, tomatoes, and items containing a lot of citric acid are some of them, along with carbonated beverages. These meals and drinks' acidity might irritate the airways, which causes coughing in people with CVA. CVA symptoms are lessened by limiting the consumption of acidic meals and choosing non-acidic substitutes alternatively. Additionally, some people with CVA benefit from using antacids to treat gastric reflux, which makes coughing up acidic foods worse.
Foods that have been processed and contain a lot of preservatives are to be avoided by CVA patients. These meals frequently contain synthetic additives and preservatives that cause the body to react inflammatory, potentially damaging the airways. Avoiding processed foods and concentrating on whole, fresh foods with little additives help some CVA patients find relief from their symptoms. Choosing items with fewer artificial additives and reading food labels are practical steps towards reducing CVA.
Foods high in histamine are known to make certain people, particularly those with CVA, cough more frequently and experience worse asthma symptoms. Foods like aged cheeses, fermented goods, and processed meats contain the naturally occurring substance histamine. Reducing histamine intake or talking to a doctor about the likelihood of histamine intolerance is beneficial for those with CVA.
Additional CVA risk factors include consuming sulphite-containing foods and beverages. Wine, dried fruit, and some processed meals all include sulphites, which are compounds that are frequently used as preservatives in a variety of foods and beverages. Despite the fact that sulphite sensitivity is very uncommon, people with CVA who suspect a reaction to sulphites must use caution and read labels carefully to prevent consuming goods that contain sulphites.
Each person's dietary needs are unique, and it's essential to pay attention to what you can and cannot eat, as well as what might worsen your CVA (cardiovascular accident) symptoms. These food sensitivities and triggers vary from person to person and aren't always related to things like histamines or allergens. Keeping a food diary and talking to a healthcare professional, like a doctor or dietitian, can help you figure out which foods are causing problems with your CVA.
If you have CVA, it's not only about avoiding problematic foods but also about having a balanced diet that's good for your overall respiratory health. Foods with antioxidants, such as fruits and vegetables, can reduce inflammation in your airways. Omega-3 fatty acids found in fish and flaxseeds can help with inflammation too. Drinking plenty of water is also important for maintaining healthy lungs.
It's crucial to know that there isn't a one-size-fits-all diet for CVA. What makes one person's symptoms worse may not affect another person the same way. So, working closely with medical experts to create a personalised diet plan that considers your unique triggers and needs is very important.
What are the risk factors of cough-variant Asthma?
Several factors contribute to the development and exacerbation of cough-variant asthma, such as encompassing genetic, environmental, and lifestyle influences.
The risk factors for cough-variant asthma are significantly influenced by genetic predisposition. An individual's risk of having CVA is increased by a family history of asthma or other allergy diseases. Specific gene variations associated with asthma susceptibility, such as those linked to airway inflammation and hyperresponsiveness, have been discovered through genetic research. When exposed to environmental stressors, people with certain genetic variations have an increased chance of developing CVA.
Environmental elements are crucial in the development of CVA. Allergy and irritant exposure cause or aggravate cough-variant asthma symptoms. In those with CVA, common allergens like mould, dust mites, pollen, and pet dander cause airway irritation and coughing. Environmental irritants like tobacco smoke, air pollution, and workplace irritants raise the chance of developing CVA or exacerbate already present symptoms. People who work in sectors that produce a lot of dust, chemicals, or fumes have a higher risk of CVA because of persistent respiratory irritation.
Another important risk factor for cough-variant asthma is respiratory infections, particularly viral infections. Infecting the airways with viruses like rhinovirus and respiratory syncytial virus (RSV) causes an inflammatory reaction that results in coughing and other asthma symptoms. People who frequently contract respiratory infections in the past, especially as children, are more prone to developing CVA. These diseases cause long-term airway hypersensitivity, which increases an individual's tendency to cough in response to a number of triggers.
Obesity has become a substantial contributor to the likelihood of developing a number of respiratory illnesses, including cough-variant asthma. Obesity causes mechanical changes in the airways, which reduce lung function and raise the chance of asthma symptoms. In addition to contributing to airway inflammation in people with CVA, obesity is linked to systemic inflammation. For people who are overweight or obese, controlling CVA requires weight loss and a healthy lifestyle.
The development and escalation of cough-variant asthma might be influenced by psychological factors including anxiety and stress. Asthma symptoms, such as coughing, are brought on or aggravated by stress-related immune system changes and heightened physiological reactions.
Additionally, people with CVA feel anxious because of their persistent cough, which creates a vicious cycle of increased stress and deteriorating symptoms.
Cough-variant asthma is frequently correlated with allergies, especially allergic rhinitis. Sneezing, runny nose, and itching are common symptoms of allergic rhinitis, which is an inflammation of the nasal passages. Coughing and other asthma symptoms result from upper airway inflammation that spreads to the lower airways. The symptoms of CVA are avoided or reduced by controlling allergic rhinitis with medication and allergen avoidance in people who are at a higher risk of acquiring it.
It is important to note that while these risk factors contribute to the development and exacerbation of cough-variant asthma, not everyone with these risk factors will develop the condition, and some individuals with CVA have all of these risk factors. Furthermore, the interplay of these factors varies from person to person, making CVA a complex and heterogeneous condition.
What are the common symptoms of cough variant Asthma?
The common symptoms of cough variant asthma are cought, wheezing and shortness of breath. Although wheezing and shortness of breath are the hallmarks of traditional asthma, coughing episodes are the main symptom of CVA. The fundamental mechanisms and causes are the same, despite the absence of these typical asthma symptoms. It is essential for an accurate diagnosis and efficient treatment to be aware of the common symptoms of cough variant asthma.
Cough variant asthma is, naturally, characterised by a chronic cough. This cough is fairly persistent, lasting for weeks or even months, and is often non-productive, meaning it doesn't generate mucus or phlegm. The cough with CVA tends to linger and does not respond to over-the-counter cough treatments, unlike a typical cough brought on by a cold or respiratory illness. It frequently happens at night or in the early hours of the morning, upsetting sleep cycles and creating discomfort.
The absence of other usual asthma symptoms like wheezing or shortness of breath is another sign of CVA. Although some people with CVA later have these typical asthma symptoms, they are rarely the first signs or symptoms. This makes it difficult to diagnose CVA because doctors do not immediately link an ongoing dry cough to asthma, especially if there is no audible wheezing.
Many people with cough-variant asthma find that their cough gets worse at night. This nocturnal cough is especially bothersome and might affect sleep. The person's cough could be extremely bothersome and it causes them and their family a lot of distress.
People who have CVA sometimes have symptoms other than coughing. They experience chest tightness, though it's typically not as severe as it is in classic asthma. Additionally, some people with CVA may develop classic asthma symptoms over time, such as wheezing and shortness of breath, which further complicates the diagnosis and management of the condition.
The symptoms of CVA are significantly influenced by triggers. The cough is made worse by specific environmental variables, just like with traditional asthma. Exposure to allergens including pollen, dust mites, and pet dander as well as irritants like cigarette smoke, pungent odours, and cold air are common triggers. Exercise-induced bronchoconstriction, a condition that causes coughing in people with CVA, is another effect of physical activity and exercise. It's crucial to remember that while these triggers could make coughing worse in CVA, they aren't always the primary cause.
The severity of CVA symptoms varies from person to person. Some people occasionally cough lightly, but others have frequent, severe coughing fits that have a big impact on their quality of life. It's also important to remember that CVA affects people of all ages, including infants and the elderly, despite the fact that it is more frequently detected in these age groups.
Clinical evaluation, medical history, and specialised tests are frequently used by healthcare professionals to diagnose CVA. Spirometry is a standard diagnostic technique that evaluates lung function and reveals underlying airway blockage even in the absence of wheezing. A methacholine challenge test is another crucial diagnostic tool that evaluates the reactivity and sensitivity of the airways to a bronchoconstrictor.
The next step is to create a specialized management strategy if a CVA diagnosis has been made. Controlling the cough and avoiding its recurrence is the main objective of CVA management. In spite of the fact that conventional asthma symptoms like wheezing are not present, this treatment includes the use of asthma drugs such as inhaled corticosteroids and bronchodilators. These drugs help to lessen coughing by reducing airway irritation and enhancing airflow.
In order to effectively manage CVA, monitoring and consistent follow-up with a healthcare professional are essential. In order to preserve the best possible symptom control, modifications to the therapy regimen may become necessary over time. Patients with CVA must be open and honest with their medical staff about their symptoms, any changes to their condition, and any possible pharmaceutical adverse effects.
How is cough variant asthma diagnosed?
An extensive medical history review is the initial stage in the CVA diagnosis process. The majority of patients who need a CVA examination are those who have had a chronic cough for more than eight weeks. The process of obtaining a patient's history allows medical professionals to learn critical details regarding the cough's genesis, course, and features, as well as any possible triggers or exacerbating circumstances. Inquiries concerning a patient's history of smoking, exposure to allergens, respiratory infections, and any family history of asthma or other respiratory disorders are common. This initial stage helps medical experts in finding any relevant indicators that point to CVA as a probable diagnosis.
A physical examination is performed after reviewing the patient's medical history. Despite the fact that people with CVA do not have the characteristic wheezing and breathlessness associated with asthma, the disorder is still detected by a number of distinct symptoms. The entire respiratory function is evaluated by healthcare professionals as they listen for any unusual breath sounds, such as wheezing or crackles. In order to rule out additional potential reasons for a persistent cough, such as postnasal drip, gastroesophageal reflux disease (GERD), or other respiratory disorders, the patient's throat, nose, and chest are also examined.
Specialised tests are used to confirm or rule out CVA after the medical history and physical examination are finished. Pulmonary function testing, particularly spirometry, is one of the best diagnostic methods for evaluating CVAs. Spirometry evaluates how much air a person takes and exhales, as well as how rapidly they do so. Spirometry findings in CVA frequently indicate normal or nearly normal lung function when the patient is at rest, but they show severe airway obstruction after the patient receives a bronchodilator. It helps to distinguish CVA from other chronic cough conditions because this reversible airway obstruction is a major feature of asthma.
The methacholine challenge test is an additional crucial examination in the diagnosis of CVA. This test evaluates airway hyperresponsiveness, a defining characteristic of asthma. Methacholine, a chemical that causes bronchoconstriction in asthmatics, is inhaled by the patient at increasing doses during the test. Throughout the test, the patient's lung function is examined, and if there is a noticeable drop, it indicates airway hyperresponsiveness and raises the possibility of a CVA diagnosis.
Healthcare professionals occasionally request further testing to strengthen the CVA diagnosis. As allergies are a trigger for CVA symptoms, allergy testing identifies particular allergens that are contributing to the cough. In order to rule out additional underlying lung problems or complications, chest X-rays and high-resolution computed tomography (HRCT) scans are carried out.
A trial of asthma drugs is advised in specific circumstances where the diagnosis is still uncertain. It is significant proof in favour of CVA if a patient with a chronic cough achieves symptom relief with the use of inhaled corticosteroids or bronchodilators. Although not all cases of persistent cough are caused by CVA, it is crucial to thoroughly monitor the patient's reaction to these drugs because a favourable response is not always evidence of the diagnosis.
Patient-reported outcomes are extremely important in the diagnosis of CVA in addition to the clinical testing and evaluations. The frequency, severity, and any triggers or patterns connected to the cough are all recorded in a patient's detailed cough diary. The nature of the cough is better understood with the aid of this information, which assists medical professionals in correctly diagnosing the condition.
It is crucial to keep in mind that the diagnostic procedure for CVA is difficult and calls for several visits to a doctor. Chronic dry cough, the predominant symptom of the atypical presentation of CVA, is easily mistaken for the symptoms of other illnesses. In order to differentiate CVA from other possible causes, it is therefore essential to take a methodical and thorough approach.
The next stage is to create a personalised treatment plan once a CVA diagnosis has been made. The main objectives of CVA treatment are to manage and control the chronic cough, stop flare-ups, and enhance the patient's general quality of life. Asthma drugs comparable to those used to treat classic asthma are frequently utilised in treatment, although they are modified to the patient's unique requirements.
Is cough variant asthma diagnosed using different medical tests?
Yes, several medical tests and diagnostic tools are available to help identify Cough variant asthma (CVA).
Pulmonary function tests (PFTs) are a crucial diagnostic tool for CVA. These tests, which measure lung function and airway reactivity, include spirometry and bronchial provocation tests. Spirometry detects any obstruction in the airways and monitors the amount and rate of air expelled. Spirometry readings in CVA are normal because it mostly affects the smaller airways. However, bronchial provocation tests, such as mannitol or methacholine challenge tests, are more sensitive in identifying airway hyperresponsiveness, which is a defining feature of asthma. In the absence of other lung disorders, a positive response on the bronchial provocation test indicates CVA.
FeNO, or fractional exhaled nitric oxide, is another crucial diagnostic test for CVA. Elevated FeNO levels are frequently observed in asthma patients, including those with CVA, as nitric oxide is a sign of airway inflammation. This non-invasive test analyses the amount of nitric oxide inhaled, helping doctors to determine airway inflammation and CVA. In order to determine a CVA diagnosis, FeNO values are often utilised in conjunction with other tests because they are raised in other respiratory disorders.
Imaging tests such as high-resolution computed tomography (HRCT) scans or chest X-rays are sometimes recommended. Although these tests are not specifically for CVA, they aid in ruling out other lung problems or complications that could be the source of the cough. The majority of the time, radiological findings in CVA are insignificant or exhibit inflammation-related symptoms such as thickening of the airway walls.
As part of the diagnostic process, blood testing is helpful. Eosinophils, a category of white blood cells linked to allergy and inflammatory reactions, may be found in high concentrations in a complete blood count (CBC). Elevated eosinophil levels support the diagnosis of CVA, although they are not exclusive to this condition and are seen in other asthma variants as well.
Another diagnostic method that is useful in the diagnosis of CVA is induced sputum analysis. Healthcare professionals identify eosinophils and other inflammatory cells by looking at the cellular makeup of the patient's sputum, which helps to establish the existence of airway inflammation associated with CVA.
How long does a cough variant asthma diagnosis last?
The duration of a cough variant asthma diagnosis varies significantly from person to person, influenced by factors such as prompt medical intervention, individual response to treatment, and the presence of underlying conditions.
The journey of a CVA diagnosis typically begins with the recognition of an unrelenting, chronic cough that lasts for weeks or even months. An individual's quality of life, sleep, and everyday activities all are negatively impacted by this cough. The length of this early phase varies considerably; some people experience symptoms for only a few weeks before seeking medical help, while others experience the cough for much longer periods of time, occasionally misdiagnosing it as being caused by allergies, environmental factors, or viral infections.
Once a CVA diagnosis is made, it is extremely unpredictable how long the ailment will continue to affect a person's life. Some people get relief and are able to effectively control their cough variant asthma by making changes to their lifestyle and taking drugs such as bronchodilators and inhaled corticosteroids. In a few weeks to months, with the correct care, cough symptoms drastically improve or perhaps go away entirely.
What are the different ways to treat cough variant asthma?
Managing CVA requires a specific treatment that targets cough suppression and tackles the underlying airway inflammation. There are numerous therapy options, including pharmacological interventions, lifestyle changes, and even complementary and alternative therapies. We will examine the various approaches to treating cough variant asthma in this in-depth talk, offering insights into their effectiveness and potential drawbacks.
Lifestyle Changes: modifying a person's way of life is the first step in managing CVA. It's essential to recognise and prevent triggers. Cold air, allergies, tobacco, and respiratory illnesses are typical triggers. People with CVA should make an effort to keep their surroundings smoke-free, utilise air purifiers, and wear warmly in cold weather. Adopting stress-reduction strategies lessens the chance of cough aggravation because stress increases or initiates CVA symptoms.
Dietary Modifications: Diet is important for managing CVA because certain foods make the condition worse. Patients must be informed about potential dietary triggers and given advice on how to stay away from them. Acidic meals, coffee, and spicy foods are typical dietary triggers. In order to control inflammation in the airways, it is helpful to promote a well-balanced diet full of anti-inflammatory foods like fruits and vegetables.
Hydration: It's important for people with CVA to maintain good hydration. Drinking enough water keeps the airways wet and lessens the incidence of coughing fits. Patients must be encouraged to sip on water frequently during the day.
Inhaled Corticosteroids: An essential component of CVA therapy is inhaled corticosteroids. They help in lowering airway inflammation, which is a major factor in this illness. Beclomethasone, fluticasone, and budesonide are typical drugs in this class. Regular use of these treatments, which are commonly given via inhalers or nebulizers, helps control coughing and stop flare-ups.
Bronchodilator: Albuterol is one example of a bronchodilator that is used to relax airway muscles and enhance airflow. Although they are not frequently used as the main form of treatment for CVA, they are often administered as an emergency measure to offer prompt relief during severe coughing fits. For certain people, it's vital to combine bronchodilators with inhaled corticosteroids.
Montelukast: Montelukast is a leukotriene receptor antagonist that is used as an additional treatment for CVA. It aids in reducing inflammation and is helpful for patients who do not respond well to inhaled corticosteroids alone or who have triggers for allergies.
Cough Suppressants: Cough suppressants, such as dextromethorphan, are used to temporarily stop coughing fits. They must be taken carefully, as they do not treat the underlying inflammation and hide symptoms that are getting worse.
Antihistamines and allergy shots (immunotherapy) are considered for people with CVA that is brought on by allergens. These remedies lessen the body's allergic reaction, which will result in fewer coughing fits.
Physical Therapy: Physical therapy, which involves strategies to enhance breathing, cough control, and airway clearance, is helpful for some people with CVA. Exercises for breathing and chest physiotherapy help manage cough symptoms and enhance overall lung function.
Acupuncture and Alternative Therapies: Although there is little scientific proof that alternative therapies like acupuncture treat CVA, some people experience comfort from them. In order to be sure these solutions are suitable and safe, it is crucial to discuss them with a healthcare professional.
Are there any home remedies to treat cough variant asthma?
Yes, Although medical care is frequently required for CVA management, some people seek home remedies to ease their symptoms.
Listed below are some important home remedies for cough variant asthma:
Steam Inhalation: Inhaling steam from a bowl of hot water relaxes the respiratory tract and lessens coughing. Additional relief is obtained by adding a few drops of essential oils like peppermint or eucalyptus. The steam relieves throat and bronchial tube irritation while helping to remove mucus. However, as this is simply a short-term remedy, it must only be used to relieve symptoms.
Hydration: It's important for people with CVA to maintain good hydration. Drinking enough water keeps the mucus in the airways thin and simpler to remove. Warm herbal teas flavoured with lemon and honey are especially comforting for a cough and sore throat. Lemon contains vitamin C, which helps the immune system, while honey has inherent anti-inflammatory effects.
Ginger tea: Ginger has long been used as a home treatment for respiratory conditions. It has anti-inflammatory qualities, which lessen coughing and calm the airways. Simply soak fresh ginger slices in hot water and flavour with honey or lemon to make ginger tea.
Honey: Honey is a well-known cough suppressant that is used as a CVA home treatment. Coughing fits are relieved by adding a teaspoon of honey to warm water or herbal tea. It is important to remember, that honey shouldn't be given to infants, younger than a year of age due to the possibility of baby botulism.
Turmeric: Turmeric contains curcumin, a compound known for its anti-inflammatory and antioxidant properties. Adding a pinch of turmeric to warm milk or water helps reduce airway inflammation and alleviate coughing. Turmeric supplements are available but should be used with caution and under medical supervision.
Humidifies: Use a humidifier in the bedroom to bring moisture to the air, which will stop the airways from drying out and lessen coughing.
Dietary Considerations: Some patients discover that specific dietary modifications assist in managing the symptoms of CVA. Avoiding foods that are known to cause inflammation, such as dairy products and meals high in sulphites, and putting an emphasis on a diet full of anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, are helpful.
Water Gargles: Warm salt water gargles are an effective way to ease a sore throat and lessen throat discomfort. When coughing causes throat irritation, this simple cure is quite helpful.
While some people with cough variant asthma find relief using these natural treatments, it's important to stress that they should not be used in place of prescription medications or expert medical guidance. Healthcare professionals are essential in choosing the best course of treatment for each patient with CVA because it is a chronic condition that needs continuing management.
Additionally, not all treatments are effective for everyone, and some people respond negatively or are allergic to specific natural treatments. Therefore, before attempting any new home remedy, especially if you have known allergies or medical concerns, it is important to speak with a healthcare professional.
Can cough-variant asthma be prevented?
Yes, while there is no known cure for CVA, there are a number of proactive measures that are taken to delay its development, lessen its impact, and enhance the general quality of life for those who are impacted by this condition.
Listed below are some important steps to prevent cough variant asthma:
Identifying the risk factors
The first step in prevention is to identify people who are susceptible to CVA. CVA is more likely to occur in those with allergies or asthma in their families. People who are allergic to dust mites, pet dander, or pollen must take care to reduce their exposure to these allergens. Identifying a person's risk factors encourages early intervention and lowers the possibility of CVA occurrence.
Avoiding allergens
Exposure to allergens significantly increases the risk of CVA. One of the most important preventive measures is to take precautions to reduce exposure to common allergies. This involves utilising air purifiers, keeping pets out of sleeping areas, and routinely cleaning and vacuuming the house to reduce dust mites.
Quitting smoking
There is sufficient evidence that smoking increases the chance of developing asthma, particularly CVA. Creating smoke-free environments and giving up smoking are crucial for prevention. Healthcare professionals provide information and encouragement to assist people in stopping smoking and lowering their chance of getting CVA.
Vaccinations
Coughing in CVA patients is often caused by respiratory diseases, such as viral or bacterial infections. It is possible to lower the chance of infection and subsequent cough exacerbations by staying up to date on immunisations, especially the annual flu shot and the required vaccines for preventable diseases like pneumonia.
Healthy Lifestyle and Regular Exercise
Living a healthy lifestyle helps to avoid CVA and, if it already exists, helps to manage its symptoms. Regular exercise enhances respiratory health and lung function. Exercise plans must be well-tolerated and not excessively demanding because severe physical activity makes people with CVA cough. A balanced diet and adequate water promote overall health and lower the chance of exacerbation.
Medication Administration
Effective medication management is crucial for those who have already been diagnosed with CVA or are at high risk due to other asthma subtypes. Long-acting beta-agonists, inhaled corticosteroids, and leukotriene modifiers are some of the drugs frequently recommended to treat CVA. In order to prevent symptoms from worsening and keep the disease under good control, it's essential to follow the recommended treatment plan and to frequently discuss it with a healthcare professional.
Action Plan for Asthma
For those with CVA, developing an asthma action plan in cooperation with a healthcare professional is essential. This plan specifies what to do if symptoms worsen, assisting patients and family members in identifying early indications of exacerbation and taking the necessary action. A carefully planned asthma action plan stops serious coughing fits and patient stays.








 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews