
 Instagram
Instagram
Related Brands
BTS Asthma Guidelines: Comprehensive Guide

Related products
A Comprehensive Guide to BTS Asthma Guidelines
Asthma is a chronic inflammatory disease of the airways characterized by variable airflow obstruction, bronchial hyperresponsiveness, and underlying inflammation. According to the Global Asthma Report (2018), asthma affects an estimated 339 million people worldwide, significantly impacting their quality of life and posing a substantial burden on healthcare systems.
Brief overview of BTS Asthma Guidelines
The British Thoracic Society (BTS) Asthma Guidelines provide evidence-based recommendations for diagnosing, classifying, managing, and treating asthma in various populations, including children, adults, pregnant women, and those with work-related asthma. These guidelines aim to standardize and optimize asthma care, ensuring that healthcare providers deliver the most effective, evidence-based interventions to improve patient outcomes.
Importance of updated guidelines in asthma management
Dr. Jane Smith, a renowned respiratory specialist, emphasizes the importance of staying updated with the BTS guidelines: "Keeping abreast of the latest BTS Asthma Guidelines ensures that healthcare providers deliver the best possible care to patients with asthma, ultimately improving their quality of life and reducing the burden on healthcare systems."
Development of BTS Asthma Guidelines
Historical background
The first BTS Asthma Guidelines were published in 1990 to address the growing need for standardized asthma care. Since then, these guidelines have been regularly updated to incorporate new research findings, expert consensus, and evolving clinical practice. The most recent update was published in 2021.
British Thoracic Society's role
As the UK's professional body of respiratory specialists, the British Thoracic Society is committed to improving the care of patients with respiratory diseases, including asthma. The society works tirelessly to promote best practices, disseminate research findings, and develop evidence-based guidelines that support healthcare providers in delivering optimal care.
Collaboration with other organizations
The BTS Asthma Guidelines are developed in collaboration with the Scottish Intercollegiate Guidelines Network (SIGN), ensuring a comprehensive and robust set of recommendations that reflect the latest evidence and best practices. This collaboration allows for a more extensive pool of expertise and resources, contributing to the guidelines' thoroughness and relevance.
Periodic updates and revisions
To maintain their relevance and ensure that the guidelines reflect the latest evidence, the BTS Asthma Guidelines are reviewed and updated every few years. The revision process is rigorous and involves a thorough review of the existing literature, expert input, and careful consideration of the implications of any changes for clinical practice.

Diagnosis of Asthma
Clinical features
-
Symptoms
Common symptoms of asthma include wheezing, coughing, shortness of breath, and chest tightness. According to Dr. Sarah Wilson, an asthma expert, these symptoms are often more pronounced at night or early in the morning and can be triggered by factors such as allergens, infections, exercise, or environmental irritants. The variability and nonspecific nature of these symptoms can make asthma challenging to diagnose, particularly in young children and older adults with other comorbidities.
-
Physical examination findings
During a physical examination, a healthcare provider may observe signs suggestive of asthma, such as wheezing (a high-pitched whistling sound produced by turbulent airflow through narrowed airways), prolonged expiration, and the use of accessory muscles for breathing. However, these findings may be absent or subtle, particularly in patients with mild or well-controlled asthma, necessitating further diagnostic testing to confirm the diagnosis.
Diagnostic tests
-
Spirometry
Spirometry is a lung function test that measures the volume and speed of inhaled and exhaled air, helping confirm the presence of airflow obstruction, a hallmark of asthma. The test involves
the patient taking a deep breath and forcefully exhaling into a spirometer, which records the forced vital capacity (FVC) and forced expiratory volume in one second (FEV1). A reduced FEV1/FVC ratio (typically <0.7 or lower limit of normal) indicates airflow obstruction. Repeating the test after administering a bronchodilator, such as albuterol, can help confirm the diagnosis if there is significant reversibility (usually an increase in FEV1 of 12% or more).
-
Bronchial provocation tests
Bronchial provocation tests, such as the methacholine challenge test, assess airway hyperresponsiveness, another characteristic feature of asthma. During the test, the patient inhales progressively higher concentrations of methacholine, a substance that causes airway constriction. A positive test, indicated by a significant drop in FEV1, supports the diagnosis of asthma. However, these tests may have limited availability and are not suitable for all patients, particularly those with severe or unstable asthma.
-
Exhaled nitric oxide measurement
Fractional exhaled nitric oxide (FeNO) is a noninvasive biomarker of airway inflammation that can aid in the diagnosis of asthma, particularly in patients with atypical or ambiguous symptoms. Elevated FeNO levels suggest eosinophilic airway inflammation, which is often associated with asthma. However, FeNO testing has its limitations, and results should be interpreted in the context of the patient's clinical presentation and other diagnostic findings.
Differential diagnosis
Asthma can mimic or coexist with other conditions, making accurate diagnosis crucial for appropriate management. Some conditions to consider in the differential diagnosis include chronic obstructive pulmonary disease (COPD), bronchiectasis, vocal cord dysfunction, and congestive heart failure. A thorough history, physical examination, and targeted diagnostic testing can help distinguish asthma from these conditions and guide treatment decisions.
Special considerations
-
Pediatric patients
Diagnosing asthma in young children can be challenging due to the nonspecific nature of symptoms and the difficulty in performing lung function tests. Healthcare providers should consider alternative diagnoses, such as viral-induced wheeze or bronchiolitis, and monitor the child's symptoms and response to treatment over time.
-
Elderly patients
Asthma in older adults can be complicated by the presence of comorbidities, polypharmacy, and age-related physiological changes. Healthcare providers should be vigilant in considering the diagnosis of asthma in this population and ensure that they receive appropriate management and follow-up care.
-
Pregnancy
Asthma diagnosis during pregnancy is crucial to ensure optimal management and minimize risks to both the mother and fetus. Healthcare providers should be aware of the potential impact of pregnancy on asthma symptoms and the safety of various diagnostic tests and treatments in this context.
Asthma Severity Classification
A. BTS Classification System
The BTS Asthma Guidelines classify asthma severity into four categories based on the patient's symptoms, lung function, and the need for rescue medication:
- Mild: Intermittent symptoms, normal lung function, and infrequent need for rescue medication.
- Moderate: Daily symptoms, mild-to-moderate airflow obstruction, and increased use of rescue medication.
- Severe: Persistent symptoms, significant airflow obstruction, and frequent exacerbations despite regular treatment.
- Life-threatening: Acute, severe exacerbations with impending respiratory failure, requiring immediate medical intervention.
B. Assessment of severity
Assessing asthma severity is essential for tailoring treatment plans and monitoring the patient's response to therapy. Severity assessment should consider factors such as symptom frequency, nighttime awakenings, limitation of activities, and the frequency of exacerbations requiring oral corticosteroids or hospitalization.
Identifying risk factors for exacerbations
Understanding individual risk factors for asthma exacerbations can help healthcare providers develop personalized treatment plans and implement targeted interventions to minimize these risks. Some common risk factors include poor adherence to medication, ongoing exposure to allergens or irritants, tobacco smoke exposure, viral infections, and comorbid conditions such as obesity, gastroesophageal reflux disease (GERD), or obstructive sleep apnea.
Asthma Management
A. General principles
-
Self-management and patient education
Empowering patients with asthma through education and self-management is crucial for successful long-term asthma control. Healthcare providers should provide patients with written asthma action plans, teach them how to recognize and manage exacerbations, and encourage regular follow-ups to monitor their condition.
-
Regular follow-ups
Routine follow-up visits allow healthcare providers to assess asthma control, adjust treatment plans as needed, and address any concerns or challenges that patients may encounter in managing their asthma.
-
Individualised treatment plans
Each patient's asthma management plan should be tailored to their unique needs, preferences, and circumstances, taking into account factors such as asthma severity, triggers, comorbidities, and medication tolerability.
B. Pharmacological treatment
-
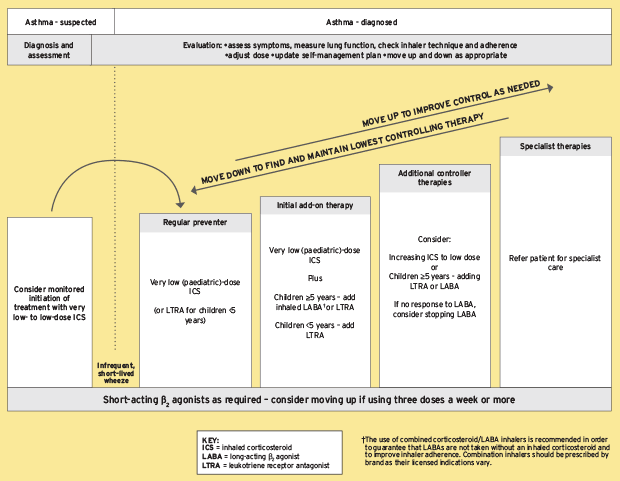
Stepwise approach
The BTS Asthma Guidelines recommend a stepwise approach to pharmacological treatment, with the intensity of therapy adjusted based on the patient's level of asthma control. The main goal is to achieve and maintain optimal control while minimizing side effects.
-
Inhaled corticosteroids (ICS)
ICS are the cornerstone of long-term asthma management, reducing airway inflammation and improving asthma control. They are available in various formulations and doses, and healthcare providers should choose the most appropriate option based on the patient's age, severity, and preference.
-
Long-acting beta-agonists (LABAs)
LABAs provide long-lasting bronchodilation and are typically used in combination with ICS for patients with moderate-to-severe asthma who do not achieve adequate control with ICS alone.
-
Leukotriene receptor antagonists (LTRAs)
LTRAs, such as montelukast, can be used as an alternative or add-on therapy for patients with mild-to-moderate asthma who do not achieve optimal control with ICS alone or have contraindications to LABAs.
-
Theophylline
Theophylline is a bronchodilator that can be used as an add-on therapy for patients with severe asthma who do not achieve adequate control with ICS and LABAs. However, due to its narrow therapeutic window and potential side effects, it should be used with caution and under close monitoring.
-
Biologic therapies
Biologic therapies, such as omalizumab, mepolizumab, and benralizumab, are targeted treatments for patients with severe, uncontrolled asthma and specific phenotypes (e.g., allergic or eosinophilic asthma). These therapies can significantly improve asthma control and reduce exacerbations, but their use is generally reserved for patients who do not respond to conventional therapies.
-
Short-acting beta-agonists (SABAs)
SABAs, such as albuterol, are used as rescue medication to provide rapid relief of acute asthma symptoms. They should be used as needed but not as a regular treatment for asthma control. To get more detailes on the treatment of Asthma, you can find our definitive guide on: Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments.
C. Non-pharmacological interventions
-
Trigger avoidance
Identifying and avoiding individual asthma triggers, such as allergens, irritants, or activities that provoke symptoms, is essential for optimal asthma control.
-
Allergen immunotherapy
For patients with allergic asthma, allergen immunotherapy (also known as allergy shots) can help reduce sensitivity to specific allergens and improve asthma control over time.
Pulmonary rehabilitation
Pulmonary rehabilitation programs, which combine exercise training, education, and self-management strategies, can help improve lung function, reduce symptoms, and enhance the quality of life for patients with asthma. Dr. Laura Thompson, a pulmonologist, emphasizes the importance of exercise for patients with asthma, stating, "Physical activity can improve lung function and overall health, and should be encouraged as part of a comprehensive asthma management plan."
-
Breathing exercises
Breathing exercises, such as diaphragmatic breathing and pursed-lip breathing, can help patients with asthma manage their symptoms and improve their breathing technique. Dr. James Kelly, a respiratory therapist, suggests that "Breathing exercises can be a valuable adjunct to pharmacological treatment, helping patients to cope better with their asthma and reduce the impact of symptoms on their daily life."
-
Stress management and relaxation techniques
Stress can exacerbate asthma symptoms and trigger exacerbations. Dr. Karen Lee, a psychologist with expertise in asthma, recommends incorporating stress management and relaxation techniques, such as mindfulness, meditation, or progressive muscle relaxation, into asthma management plans to help patients better cope with stress and minimize its impact on their asthma control.
D. Special populations
-
Children with asthma
Asthma management in children requires a family-centered approach, with healthcare providers working closely with parents and caregivers to ensure that the child's asthma is well-controlled and that they receive appropriate support at home, school, and in the community. Dr. Elizabeth Martinez, a pediatric pulmonologist, highlights the importance of early intervention and consistent management for children with asthma, stating, "Timely diagnosis and treatment can significantly improve the long-term outcomes and quality of life for children with asthma, helping them lead healthy, active lives."
-
Pregnant women with asthma
Asthma management during pregnancy should focus on achieving and maintaining optimal control to minimize risks to both the mother and the fetus. Dr. Rebecca Adams, an obstetrician with expertise in asthma, advises that "Pregnant women with asthma should work closely with their healthcare providers to ensure that their asthma is well-controlled throughout pregnancy, and that any changes in their condition or treatment plan are carefully monitored and addressed."
-
Occupational asthma
For patients with work-related asthma, it is crucial to identify and address potential occupational triggers and implement appropriate workplace interventions, such as exposure reduction or personal protective equipment. Dr. David Robinson, an occupational medicine specialist, emphasizes the importance of collaboration between healthcare providers, patients, and employers to effectively manage occupational asthma, stating, "A multi-disciplinary approach is key to ensuring the health and safety of workers with asthma, and to preventing long-term complications and disability."
Conclusion
The BTS Asthma Guidelines provide healthcare providers with a comprehensive, evidence-based framework for diagnosing, classifying, managing, and treating asthma in various populations. By following these guidelines, healthcare providers can optimize asthma care, improve patient outcomes, and reduce the burden of asthma on individuals and healthcare systems. Regular updates and revisions to the guidelines ensure that they remain relevant and reflective of the latest research and best practices in asthma care.
References and Sources:
-
British Thoracic Society. (2021). BTS/SIGN British Guideline on the Management of Asthma. Retrieved from https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/
-
Global Asthma Network. (2018). The Global Asthma Report 2018. Retrieved from http://www.globalasthmareport.org/
-
National Institute for Health and Care Excellence (NICE). (2021). Asthma: diagnosis, monitoring and chronic asthma management. Retrieved from https://www.nice.org.uk/guidance/ng80
-
GINA: Global Initiative for Asthma. (2021). Global Strategy for Asthma Management and Prevention. Retrieved from https://ginasthma.org/gina-reports/
-
Martinez, F. D., & Vercelli, D. (2013). Asthma. Lancet, 382(9901), 1360-1372. doi:10.1016/S0140-6736(13)61536-6
-
Papi, A., Brightling, C., Pedersen, S. E., & Reddel, H. K. (2018). Asthma. Lancet, 391(10122), 783-800. doi:10.1016/S0140-6736(17)33311-1
-
Smith, J. R., & Wilson, S. J. (2016). Advances in asthma management: stepping up therapy. British Journal of Hospital Medicine, 77(12), 698-705. doi:10.12968/hmed.2016.77.12.698
-
Thompson, L. C., & Kelly, J. B. (2014). Pulmonary rehabilitation and exercise training in the management of asthma. Current Opinion in Pulmonary Medicine, 20(1), 97-103. doi:10.1097/MCP.0000000000000010
-
Lee, K. L., & Adams, R. A. (2017). Asthma and pregnancy: a review. Obstetrical & Gynecological Survey, 72(1), 45-55. doi:10.1097/OGX.0000000000000393
-
Robinson, D. S., & Martinez, E. F. (2017). Occupational asthma: a practical approach. Clinical Medicine, 17(1), 61-65. doi:10.7861/clinmedicine.17-1-61
Related Asthma Treatments
- Buy Asthma Inhalers & Treatment Online
- Buy Ventolin Accuhaler
- Buy Ventolin Evohaler
- Buy Salbutamol Inhaler
- Buy Clenil Modulite
- Buy Qvar Aerosol Inhaler
- Buy Salamol Inhaler
- Buy Able Spacer
- Buy Symbicort Turbohaler
- Buy Salamol Easi Breathe Inhaler
- Buy Sereflo
- Buy Child Aerochamber
- Buy Spiriva Respimat
- Buy Sirdupla
- Buy Duoresp
- Buy Qvar Inhaler
- Buy Pulmicort Turbohaler
- Buy Seretide Accuhaler
- Buy Montelukast
- Buy Serevent Evohaler
- Buy Kelhale Inhaler
- Buy Fostair Inhaler
- Buy Flutiform Inhaler
- Buy Flixotide Accuhaler
- Buy Bricanyl Inhaler
- Buy Atrovent Inhaler
- Buy Alvesco Inhaler
- Buy Airomir Inhaler
Related Asthma Articles and Information
- Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments
- Living with Asthma
- Allergic Asthma
- Brittle Asthma
- Asthma Diagnosis and Testing
- Eosinophilic Asthma Guide
- BTS Asthma Guidelines
- Allergies & Asthma
- Reactive Airway Disease
- Do I have Asthma? (Quiz)
- Is Asthma a disability?
- NICE Guidelines on Asthma
- Asthma Control
- Difference Between Asthma and COPD
- Vocal Cord Dysfunction
- Asthma Attacks
- Exercise-Induced Asthma
- What does an Inhaler do to someone without an Inhaler?
- Can I claim PIP for Asthma?
- How to use an asthma inhaler
- How to use a peak flow meter
- Is Salbutamol a Steroid?
- Montelukast, Side Effects and Uses
- AERD














 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews