Nighttime Asthma (Nocturnal Asthma): Definition, What Triggers It, Symptoms and Treatments


Related products
Nighttime Asthma (Nocturnal Asthma) Overview
Asthma is a chronic respiratory condition that affects millions of people worldwide, impacting their daily lives and overall well-being. The daytime symptoms of asthma, such as wheezing, shortness of breath, and chest tightness, are well-known to many people, however, there is a less well-known but no less devastating feature of this condition known as nighttime asthma. The term "nighttime asthma," also referred to as "nocturnal asthma," describes asthma symptoms that worsen or become more noticeable, especially at night. This frequently results in disturbed sleep, a decline in quality of life, and higher medical expenses.
Even though asthma symptoms happen at any time of day, many asthmatics find that their symptoms seem noticeably worse at night. It is a particularly troublesome feature of the condition because nighttime asthma presents special difficulties and complications that are not always present during the day.
The severity of asthma symptoms is influenced by the circadian rhythm, the body's internal clock. Many people's asthma symptoms seem to get worse between 2 and 4 in the morning. This is believed to be connected to the lung function fluctuations that occur naturally during the day.
It is more difficult to breathe when supine (lying down) when sleeping due to the redistribution of lung fluids and increased airway resistance. This shift in posture is a contributor to asthma symptoms at night. Some people undergo hormonal changes during the night, which have an impact on bronchoconstriction and airway inflammation.
The defining feature of asthma at night is persistent coughing. It is severe enough to cause the person to awaken from sleep and dry or produce mucus. A high-pitched whistling sound is made when breathing during nocturnal wheezing. It is brought on by constricted airways and is heard during exhalation.
Asthma at night is a complicated and frequently underestimated aspect of asthma that has a significant influence on the lives of those affected. It is crucial for enhancing asthma management and general quality of life to comprehend the causes, diagnosis, and available treatments for nocturnal asthma. With the right management, adherence treatment, and lifestyle changes, people with nighttime asthma can better control their symptoms, get better sleep, and live healthier, more productive lives.
The components of basic care are opportunities to help people with asthma to understand their condition, to know how to keep their asthma under control and know when to seek help, as explained by Dr Andy Whittamore, GP.
What is Nighttime asthma?
Nighttime asthma, also known as nocturnal asthma, refers to the worsening of asthma symptoms, such as coughing, wheezing, and shortness of breath, during the nighttime hours. Nighttime asthma disrupts sleep and lead to poor asthma control if not managed effectively. Nocturnal asthma is a critical illness that necessitates appropriate treatment and preventative measures because many fatal and severe episodes of asthma occur at night.
Asthma is a chronic respiratory illness affecting 1-18% of the people. Asthmatics exhibit a variety of symptoms including wheezing, breathlessness, chest tightness, and/or coughing with varied expiratory airflow limitation. Numerous asthma patients are unable to control their symptoms despite receiving intensive therapies for the condition, even when such treatments are administered in accordance with the recommended standards. Many of these are due to symptoms occurring in the night, known as nocturnal asthma.
There are still certain asthmatic patients who experience nocturnal symptoms, despite the fact that several treatments exist that attempt to reduce the inflammatory processes or have a direct bronchodilating impact, such as different types of beta-2 receptor agonist therapies. These findings imply that the nighttime symptom is influenced by additional factors.
In the hours before and during sleep, nocturnal asthmatics may have coughing fits, chest tightness, wheezing, and shortness of breath. Patients are repeatedly awakened which makes them drowsy, unfocused, and unable to control their asthma symptoms during the day in both adults and children. On quality of life, this has a considerable effect.
Lying on one's side or front while sleeping restricts airflow, which could exacerbate nocturnal asthma symptoms. While doing so, sleeping flat on the back causes nasal mucus to trickle down to the throat and start a nighttime cough.
A cool environment is healthier for sleeping, but if sleep in an air-conditioned room during the winter, the nighttime asthma gets worse. This is due to the fact that cold air is dry; a loss of heat and moisture in the airways might result in an asthma attack.
Lack of sleep exacerbates asthma symptoms, whether they are brought on by asthma symptoms or just from staying up too late. Lack of sleep increases the likelihood of an asthma attack by encouraging inflammation in the body and affecting lung function.
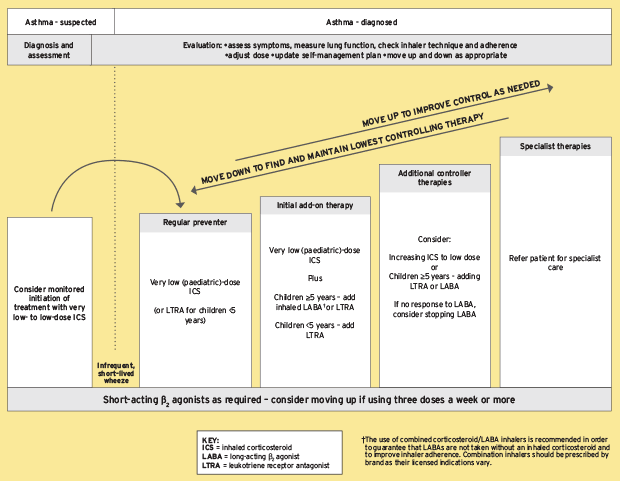
Taking asthma medications and creating a plan to stay away from triggers that aggravate asthma are two common ways to control the condition. There are two types of asthma medications: quick-relief medications that control asthma attacks and long-term control therapies that lessen the frequency and intensity of upcoming asthma attacks.
The American Lung Association advises persons with asthma to speak with their doctor about their Asthma Action Plan at least once a year. Even yet, asthma occasionally gets out of control, despite the best of plans. It's crucial to contact a healthcare physician immediately if an asthmatic person starts developing new symptoms or has problems with everyday tasks like cooking, cleaning, or taking a shower.
It is difficult to obtain a good night's sleep if you have asthma, so it's important to develop sleep-supportive habits. The first important step is to concentrate on enhancing sleep hygiene. People with asthma lessen unnecessary daytime fatigue and concentrate on managing their asthma symptoms by creating a regular sleep pattern and healthy daytime routines.
Asthma at night is brought on by dust mites and bug droppings in the bedroom. It is quite beneficial to eliminate or reduce exposure to these triggers. Weekly vacuuming and dusting, along with frequent sheets and towel washing. It is helpful to use bedding that is resistant to allergens, such as mattress covers and pillows.
When do nighttime asthma attacks?
Although asthma symptoms happen at any time, many asthmatics report that their symptoms seem worse or are more obvious at night. Several factors contribute to this phenomenon. Circadian rhythms are a type of biological internal clock that regulates many physiological processes in our bodies, including lung function. The early morning hours, often between 3 and 4 a.m., are when lung function is at its lowest for many people with asthma. Asthma symptoms may worsen at this time of year due to the natural decline in lung function.
Asthma symptoms are brought on by allergens including pollen, dust mites, and pet dander. People who are sleeping during the night come into touch with allergens in their bedding, pillows, or bedroom settings. Asthma attacks at night result from this exposure, which worsens asthma symptoms.
People with asthma have less sensitive airways at night due to temperature and humidity changes. While warm, humid air encourages the growth of mould and dust mites, aggravating asthma symptoms, cold, dry air irritates the airways and causes bronchoconstriction.
With GERD, stomach acid flows back into the oesophagus and even enters the throat and airways. Because acid reflux often happens more frequently when you're lying down, it exacerbates asthma symptoms and increases the risk of having an asthma attack at night.
Some asthma treatments do not offer sufficient coverage all night long. Asthma symptoms get worse at night if long-acting bronchodilators or controller drugs stop working.
A person's sleeping position has an impact on their asthma symptoms. While sleeping with the head up helps relieve symptoms by reducing acid reflux and providing better airflow, lying flat on the back makes it harder to breathe.
Asthma symptoms are made worse by stress and anxiety, and they are worse at night when people are more likely to be by themselves with their thoughts.
What triggers Nighttime Asthma?
Effective management requires a thorough understanding of the triggers of nocturnal asthma. Asthma sufferers lessen the frequency and intensity of nocturnal symptoms, resulting in better sleep and general health, by recognising and managing these triggers. Working collaboratively with medical professionals to create a specialised asthma treatment plan that addresses both daytime and overnight symptoms is crucial for enabling people with asthma to live better, more pleasant lives.
Several triggers exacerbate asthma symptoms during the night including:
Allergen
Allergens play a pivotal role in the manifestation of asthma, both during the day and at night. The body's susceptibility to specific allergens including pollen, dust mites, pet dander, and mould spores is the main cause of allergic asthma, which makes up a significant proportion of asthma cases. When these allergens are breathed, the immune system responds by generating histamines and other inflammatory compounds, which cause the typical asthmatic symptoms.
People with asthma are more likely to experience allergic-induced exacerbations at night because of a number of variables. The body's inherent circadian rhythm is one important factor. As a result of the natural drop in lung function that occurs at night, airways are more susceptible to swelling and constriction. As a result, asthma sufferers are more likely to suffer from severe symptoms brought on by nocturnal allergen exposure.
The presence of allergens can change during the day, with many airborne allergens being more concentrated at night. For example, dust mites, which are typical indoor allergens, prefer the warm, humid environments frequently present in mattresses and carpets, where they thrive. People who accidentally stir up these allergens when they go into bed for the night are exposed to them and experience symptoms of asthma.
Additionally, overnight habits increase exposure to allergens. During the warmer months, people frequently participate in actions that increase their risk of coming into contact with allergens, such as sleeping with dogs or keeping windows open. Although they seem harmless, these habits significantly affect how severe nocturnal asthma is.
The impact of allergens on nocturnal asthma goes beyond symptom worsening; it has an impact on how well treatments work. Allergen avoidance strategies are necessary for people with allergic asthma, including using allergen-proof covers on pillows and mattresses, keeping a clean and dust-free sleeping environment, and possibly thinking about allergen immunotherapy (allergy shots) to desensitise the immune system to particular allergens.
GERD
One of the key links between GERD and nocturnal asthma is the microaspiration of gastric contents into the airways. In GERD, the oesophagus experiences refluxed stomach acid. Particularly while lying down at night, it aggravates or induces asthma symptoms. In some cases, stomach acid and partially digested food pass through the oesophagus and into the respiratory system, irritating and inflaming the airways. This discomfort, especially at night while you're lying down, starts or aggravates asthma symptoms.
GERD make the airways more sensitive to irritants and allergens as well as other stimuli. Due to their increased airway reactivity, people with GERD and asthma are more prone to nighttime asthma attacks brought on by typical environmental triggers such as dust mites, pollen, or pet dander. GERD activate reflex mechanisms that lead to bronchoconstriction and more mucus being produced in the airways. This makes asthma symptoms worse, especially at night when the body is more likely to have reflex reactions.
Some GERD drugs, including proton pump inhibitors (PPIs), interact with asthma medications. PPIs, for example, lessen the efficiency of inhaled corticosteroids, which are frequently recommended to treat the symptoms of asthma. The management of both illnesses becomes more challenging due to their interaction.
Episodes of nocturnal asthma interfere with sleep cycles, resulting in poor sleep quality and a higher risk of developing GERD symptoms. On the other hand, GERD-related nocturnal symptoms like heartburn and regurgitation cause sleep disruption, which exacerbates asthma symptoms because of sleep deprivation and throws off circadian rhythms.
Cold air and temperature changes
The effect of cold air on airway sensitivity is one of the main factors contributing to the worsening of asthma symptoms. Bronchoconstriction, a defining characteristic of asthma, results from breathing in cold air because it narrows the airways. Asthmatic patients find it challenging to breathe because of this constriction's narrowing of the airways. Additionally causing airflow obstruction by cold air enhances mucus formation in the airways. The heightened sensitivity of the airways to cold is a major factor in why asthma symptoms deteriorate at night.
Asthma sufferers experience an inflammatory reaction in their airways as a result of temperature changes, especially when they occur when warm daytime temperatures change to cooler overnight ones. The bronchial reactivity rises as a result of this inflammation, which increases the likelihood of airways narrowing and becoming irritated. The body's natural defences might be less efficient in reducing this inflammation as temperatures drop at night, which explains why asthma symptoms might worsen at night.
The impact of cold air and temperature changes on nocturnal asthma extends beyond the physiological aspects. As a result of the discomfort and breathing problems, it is difficult to fall asleep or to stay asleep for long periods of time. Stress and sleep loss both have a negative feedback cycle effect on asthma symptoms. The condition of nocturnal asthma becomes worse for patients as a result of increased stress and anxiety caused by overnight symptoms.
Stress and anxiety
Stress and anxiety play a significant role in the development and exacerbation of nocturnal asthma. anxiety and stress enhance the sensitivity of the airways, making them more likely to constrict in reaction to certain triggers, such as allergens and irritants. The symptoms of asthma, particularly nighttime exacerbations, are influenced by this increased airway reactivity.
Stress triggers the body's stress response, which causes the release of stress hormones including cortisol and adrenaline. These hormones have an impact on the way the immune system and the airways work, which causes asthmatics' inflammation and bronchoconstriction to worsen.
What are the causes of nighttime asthma?
Common causes of nighttime asthma include increased exposure to allergens like dust mites or pet dander, changes in lung function and hormones at night, and lying down, which may trigger airway constriction. Gastroesophageal reflux disease (GERD) can also worsen nighttime asthma. Asthma at night is a complicated, multifaceted illness with many underlying causes. The onset and severity of nocturnal asthma symptoms are influenced by a variety of physiological mechanisms, environmental triggers, medication-related concerns, psychological variables, lifestyle choices, genetic predispositions, and concurrent medical illnesses.
Listed below are some common causes of nocturnal asthma:
Circadian rhythms
The circadian rhythm, which governs a 24-hour cycle in the human body, has an impact on many physiological functions, including lung function. According to studies, lung function naturally drops at night, which causes asthmatics' airways to become more resistant to airflow and limit it.
Certain hormones, including cortisol, are produced by the body according to a circadian rhythm. Cortisol acts as a natural anti-inflammatory and bronchodilator. Reduced cortisol levels at night may contribute to increased bronchoconstriction and inflammation, aggravating asthma symptoms.
Hyper-responsive airway
People with asthma have airways that are particularly susceptible to a variety of stimuli, including allergens, irritants, and infections. The airways become more reactive at night, when the body's defences are weak, resulting in increased bronchoconstriction and mucus production.
The airways' cilia, which resemble tiny hairs, are essential for removing mucus and other objects. The accumulation of mucus in the airways brought on by decreased ciliary activity during sleep might make it difficult to breathe.
Environmental allergen
It's crucial to remember that not everyone who has asthma is sensitive to the same allergens, and allergic reactions vary greatly in intensity. Identifying and reducing exposure to allergens that cause symptoms, using the recommended asthma medications, and generally keeping excellent asthma control are all important aspects of managing nocturnal asthma.
There are some specific factors and allergens that are more prominent at night including:
Dust Mites: Dust mites are little insects that are found in mattresses, pillows, and bedding. Especially while you are lying in bed at night, their bodily waste and particles become airborne and cause asthma symptoms when you breathe them in.
Pet Allergens: When you have indoor pets, their dander (minuscule skin flakes), saliva, and urine cause serious allergic reactions in some people. These allergens accumulate in the carpets, furniture, and beds, where they are concentrated more so at night.
Mould: Mould spores are a typical indoor allergen that is found in moist or inadequately ventilated spaces like bathrooms and basements. Mould spore concentrations may increase at night because indoor air is more stagnant then. This could potentially exacerbate asthma symptoms.
Cockroach allergens: The allergenic proteins found in cockroach droppings and body parts might exacerbate asthma symptoms. When cockroaches are active at night, people are more prone to experience cockroach infestations.
Secondhand smoking: It is generally known that asthma is triggered by exposure to secondhand smoking. Inhaling smoke from cigarettes or other sources while at home or in your bedroom makes the asthma symptoms worse at night.
Pollen: Despite being primarily an outside allergen, some people may bring pollen inside their houses on their clothing or pets. Additionally, open windows and doors allow pollen to enter indoor rooms. Because of the slower wind speeds at night, pollen levels may also be higher.
Genetic Influence
People who have a history of asthma in their families are more likely to acquire asthma, including nighttime asthma. The likelihood of inheriting an asthmatic tendency is influenced by genetics.
The chance of developing asthma has been linked to specific genetic variations. Variations in the genes that regulate bronchial reactivity, airway inflammation, and immunological responses can increase a person's risk of developing asthma and exhibiting symptoms at night.
The complex condition of asthma is influenced by both genetic and environmental factors. Asthma development and symptom exacerbation, especially nighttime symptoms, are influenced by a combination of environmental variables, including allergens, respiratory infections, and irritants, as well as genetic susceptibility. The way a person reacts to asthma medications depends on genetic factors. The management of asthma symptoms at night is affected by genetic variations that make some people more or less responsive to specific asthma medications.
Smoking
Smoking causes chronic inflammation and is a significant irritant to the airways. One defining characteristic of asthma is airway inflammation. Smoking exacerbates this inflammation in an asthmatic person, making the airways more sensitive and prone to overnight exacerbations.
Smoking causes the airways to produce more mucus. In cases of asthma, excessive mucus production further constricts the airways, making breathing challenging, especially at night.
Smoking results in chronic obstructive pulmonary disease (COPD), which is characterised by deteriorating airway health and diminished lung capacity. A person with asthma who smokes develops COPD, which could cause their lung function to worsen and make it harder to control their asthma symptoms at night.
The effectiveness of asthma treatments, such as bronchodilators and inhaled corticosteroids, is decreased by smoking. This leads to insufficient management of asthma symptoms, including those that occur at night.
The immune system is weakened and the danger of respiratory infections is increased by smoking. Exacerbations of asthma, including those that happen at night, are brought on by these infections.
It's crucial for those with asthma to give up smoking or stay away from secondhand smoke, especially those who suffer from nighttime symptoms. One of the best actions a person take to improve their asthma management and general respiratory health is to stop smoking. For treating and preventing nocturnal asthma symptoms, a healthcare provider's suggested asthma management plan must be followed, including taking prescribed medications as instructed.

What are the symptoms of nighttime asthma?
The symptoms of nighttime asthma include coughing, wheezing, shortness of breath, difficulty sleeping and chest tightness at night. Listed below are some common symptoms of nighttime asthma:
Coughing
When someone has nocturnal asthma, they frequently have a cough that is different from daytime coughing. It is typically dry and persistent and is brought on by even the smallest irritants, including dust mites or alterations in the temperature of the room. This constant nighttime coughing impairs sleep, causes exhaustion, and decreases one's quality of life in general.
It's crucial to find and treat the root causes of coughing in nocturnal asthma in order to control it successfully. Asthma control issues are one of the main causes. The likelihood of having nocturnal symptoms, such as coughing, is higher in people with poorly controlled asthma. The symptoms of nocturnal asthma, including coughing, can be greatly diminished by taking prescribed asthma drugs, such as bronchodilators and inhaled corticosteroids, on a regular basis.
Wheezing
Wheezing is characterised by a high-pitched whistling sound when breathing. It is caused by narrowed airways and is particularly noticeable during the night.
Although asthmatics find it difficult to regulate their nighttime wheezing, their symptoms are better controlled with the correct techniques and drugs. In order to reduce nocturnal wheezing and enhance overall asthma control, it is crucial to recognise and prevent triggers, follow medication regimens, and get professional advice. Asthma sufferers get more peaceful sleep and a higher quality of life by treating their overnight symptoms.
A localised or widespread obstruction or constriction of the airways from the larynx to the small bronchi causes wheezing. Bronchoconstriction, mucosal oedema, external compression, partial obstruction by a tumour, foreign material, or persistent secretions are a few possible causes of airway narrowing. The nearly airway-closed walls of airways are believed to oscillate or vibrate, which produces wheezes.
According to Bernoulli's principle, reduced gas pressure and flow are produced in the constricted area when air is forced through a restricted part of an airway at a high velocity. At some point, the internal airway pressure starts to rise and then the airway lumen just opens again. It causes a "fluttering" of the airway walls and a melodic, "continuous" sound when the airway alternates between being nearly closed and nearly open.
Shortness of breath
People with nighttime asthma feel out of breath or experience breathing difficulties. This symptom ranges in severity from mild to severe, depending on the patient and the presence of triggers. Breathing problems have a significant impact on how much exercise a person tolerates.
Breathing problems stand out as one of the most distressing and incapacitating symptoms encountered by people with nighttime asthma. Breathing problems are a recognisable indicator of nighttime asthma. It occurs as a result of the airways' swelling and constriction, which prevents enough air from entering and leaving the lungs. When someone has nighttime asthma, their immune system overreacts to some allergens, which results in an inflammatory response in the airways. The muscles that surround the airways constrict due to the inflammation, which results in swelling and an increase in mucus production.
Bronchoconstriction considerably worsens breathing issues. Constrictions in the airways, which make it harder for air to pass through, lead to shortness of breath and the unique wheezing sound. Breathing issues range in severity from slight to severe, and occasionally become life-threatening, requiring urgent medical care.
Breathing issues have a significant negative impact on a person with asthma's quality of life. Simple tasks like climbing stairs, exercising, or even conversing become difficult for people with asthma.
Difficulty sleeping
Sleep disturbance in people with nighttime asthma is a complicated problem that has a big impact on their health and well-being. Healthcare professionals create complete treatment programmes that include both asthma management and sleep interventions by knowing the causes and appreciating how critical it is to address sleep disruption in nighttime asthma. Patients and healthcare professionals must work together to improve asthma control and sleep quality, which will ultimately improve the quality of life for people who have nighttime asthma.
The nocturnal symptoms of nighttime asthma, such as coughing, wheezing, shortness of breath, and tightness in the chest, are more frequent and intense. It is difficult to get a good night's rest because these symptoms can cause a person to wake up from sleep.
Obstructive sleep apnea (OSA) and nocturnal asthma are two breathing conditions that are more likely to develop in people with nighttime asthma. OSA is characterised by brief stops in breathing during sleep due to partial or total obstruction of the upper airway. Short-acting beta-agonists and oral corticosteroids are two examples of drugs used to treat asthma that interfere with sleep or induce insomnia. Sleep difficulties in people with nighttime asthma are made worse by these adverse effects.
The illness known as obstructive sleep apnea (OSA) causes the airways to shrink or close off while you're asleep. Asthma and OSA tend to have a reciprocal link and similar symptoms. This implies that the chance of developing one of these respiratory disorders increases with the presence of the other. People with asthma who snore and those whose asthma symptoms are not well-controlled are more likely to have OSA.
Having a discussion with their doctors about obstructive sleep apnea is beneficial for those with asthma. Research indicates that routine OSA screenings are beneficial in people with asthma because having asthma increases one's risk of getting OSA. Fortunately, treating OSA frequently lessen the symptoms of asthma. Working with a physician, allergist, or pulmonologist (lung specialist) to establish a specialised Asthma Action Plan frequently helps reduce asthma symptoms.
Patients with persistent asthma must be managed with the proper medicine, such as beta-agonists and inhaled corticosteroids. However, despite the use of inhaled corticosteroids (ICS), a significant number of patients continue to experience symptoms, particularly at night. Patients with bronchial diseases experience poor quality of life, sleep deprivation, and anxiety as a result of their nocturnal dyspnoea and alertness. In order to evaluate the disease's control, asthmatic sleep and nighttime management may be relevant.
There are links between asthma-related symptoms and sleep problems. When compared to patients without bronchial problems, asthmatics are more likely to experience difficulty falling asleep, disturbed sleep on polysomnography, early morning awakenings, and daytime drowsiness. Over 40% of children with asthma exhibit clinically significant daily sleepiness. Adult asthmatics who experienced significant daytime sleepiness comprised 50% of the population.
There is now strong evidence that asthmatic symptoms, sleep issues, activity restrictions, lung function impairment, and the need for rescue drugs can all be managed with the right treatment. When asthma is under control, symptoms only sometimes reoccur, and severe exacerbations must be uncommon.
Chest tightness at night
In people with nighttime asthma, tightness in the chest and pain are caused by complex interactions between the neurological system, immunological system, and respiratory system. These symptoms are caused by a number of important factors including:
- Airway Inflammation: In people with nighttime asthma, persistent airway inflammation results in more production of mucus and bronchial constriction, which causes a tightness in the chest.
- Bronchospasm: The rapid contraction of the airway muscles known as bronchospasm causes the already swollen airways to become even more constricted, resulting in discomfort and chest pain.
- Hyper-responsiveness: People with nighttime asthma have airways that are overly sensitive to a variety of triggers, such as allergens, smoke, or exercise, which can cause tightness in the chest and pain.
- Air trapping: In nighttime asthma, the accumulation of air causes prolonged expiration, which causes expansion of the lungs and leads to chest discomfort.
Clinical Consequences
In patients with nighttime asthma, chest tightness and pain have important clinical consequences that affect the patient's general health:
- Reduced quality of life: Physical activity, sleep, and daily functioning can all be greatly restricted by chest tightness and pain, which results in a decreased standard of life.
- Patients with uncontrolled asthma frequently experience numerous exacerbations and need hospitalisations, which become a load on the healthcare system.
- Side effects of medication: Muscle cramps and digestive problems might occur while using high doses of medicines to treat nighttime asthma.
How can nighttime asthma be treated?
Nighttime asthma has no known cause or treatment, however routine asthma treatments, such as inhaled steroids, are very successful at lowering inflammation and preventing nocturnal symptoms. Nighttime asthma, known as nocturnal asthma, strikes at any time when a person is sleeping, thus asthma medication must be effective during these hours.
Long-acting bronchodilators are useful for reducing asthma symptoms and bronchospasm when administered via asthma inhalers. Long-acting inhaled corticosteroids are helpful for people with nocturnal asthma. A medicine that lessens stomach acid production if you have GERD with asthma. Avoiding allergens like dust mites, pet hair, and feathers in down bedding is highly beneficial in reducing allergies, asthma, and nocturnal asthma attacks.
Listed below are some treatment options for nighttime asthma:
Bronchodilators: Bronchodilators are a class of medications designed to relax and widen the airways in the lungs, making it easier to breathe. They are typically employed to quickly alleviate acute asthma symptoms, including those that manifest at night. Short-acting beta-agonists (SABAs) and long-acting beta-agonists (LABAs) are two popular categories of bronchodilators.
SABAs work swiftly to reduce bronchospasm and symptoms like wheezing and shortness of breath. Examples of SABAs include albuterol and levalbuterol. These medicines—often referred to as "rescue inhalers"—are crucial for controlling asthma attacks at night. When used properly, SABAs can offer quick relief, allowing people to breathe more easily and enhancing the quality of their sleep.
Contrarily, LABAs offer long-lasting bronchodilation and are frequently used as maintenance therapy in conjunction with inhaled corticosteroids (ICS) to manage asthma symptoms over an extended period of time. Although LABAs aren't frequently used as rescue drugs for asthma attacks that happen at night, they help lessen the frequency and intensity of nocturnal symptoms when used along with other asthma treatments.
Bronchodilators have a role in managing asthma at night that goes beyond just giving short-term relief. When used wisely, they act as a preventative step. Before bed, those with nocturnal asthma find it beneficial to take a SABA to lessen the likelihood of overnight symptoms. With this proactive strategy, people can get a better night's sleep and lessen the interruption brought on by asthma.
However, it's essential that people with nocturnal asthma utilise bronchodilators under a doctor's supervision. Overuse of SABAs may result in tolerance, decreased effectiveness, and potential adverse effects including tremors and an elevated heart rate. Healthcare professionals assist patients in creating a personalised asthma action plan that addresses their unique requirements, including when and how to use bronchodilators in a safe and efficient manner.
Inhaled corticosteriod (ICS): The cornerstone of asthma treatment, for both daytime and nighttime symptoms, is inhaled corticosteroids. They are anti-inflammatory drugs that function by lowering airway inflammation and suppressing the body's immunological reaction in the lungs. This approach aids in preventing and managing asthma symptoms, including those that manifest at night.
The capacity of ICS to target the underlying inflammation in the airways is one of the main advantages of using them for nocturnal asthma. ICS aids in preventing the airway constriction that causes discomfort at night by lowering inflammation. As a result, those who have nocturnal asthma have fewer episodes of coughing, wheezing, and breathlessness at night, which may enhance their sleep quality and general health.
Their long-term control effect is a significant component of ICS in the therapy of nighttime asthma. Contrary to some other asthma treatments, such as short-acting beta-agonists (SABAs), which reduce symptoms quickly without treating the underlying inflammation, ICS work to maintain control. Over time, ICS use on a regular basis aids in lowering the frequency and severity of nighttime asthma attacks, enabling people to have more restful sleep and live better.
It's crucial to understand that even while ICS are quite successful, they do not provide a permanent cure for asthma at night. In order to enjoy their full benefits, they frequently need regular use over an extended period of time.
Leukotrienes Modifiers: Leukotrienes are lipid substances that the body's numerous cells, especially immune cells, manufacture. They are implicated in the bronchoconstriction and airway inflammation seen in asthma and play a crucial role in the inflammatory response. Leukotriene modifiers are drugs made particularly to target and control leukotriene activities. By doing this, they provide an important treatment choice for controlling asthma, especially asthma attacks at night.
Montelukast is one of the most important leukotriene modifiers frequently used to treat asthma. The way this drug works is by inhibiting the leukotriene receptor, which essentially stops leukotrienes from binding and starting the chain of events that causes inflammation and bronchoconstriction. Montelukast has a variety of uses and benefits in the treatment of asthma at night.
Leukotriene modifiers like montelukast, in particular, have a prolonged duration of action. This means that taking a single tablet in the evening will protect you against nocturnal asthma symptoms all night through. This is a game-changer for people with nocturnal asthma since it helps them get a better night's sleep, wake up with better lung function, and have fewer symptoms.
Moreover, it has been demonstrated that montelukast is efficient in addressing the specific processes and triggers that lead to asthma flare-ups at night. These triggers frequently include changes in airway inflammation with the hour of the day, increased exposure to allergens, and the normal reduction in lung capacity at night. By preventing leukotriene-mediated inflammation and lowering airway hyperresponsiveness, montelukast lessens the effects of these factors and improves asthma management at night.
Leukotriene modifiers provide benefits in terms of accessibility as well. Typically, they are given orally and frequently come in the shape of tablets or granules. This makes them a practical choice for people who might have trouble using inhalers or who prefer a non-invasive method of managing their asthma. Montelukast is also generally well tolerated and associated with a minimal risk of side effects, making it appropriate for a variety of asthma patients, including youngsters.
Biologic therapy: Biologic therapies, also known as monoclonal antibodies, have revolutionised the treatment landscape for asthma by targeting specific components of the immune system responsible for driving inflammation in the airways. The goal of these biologics is to treat severe asthma phenotypes that do not respond well to conventional therapies. Omalizumab, an anti-IgE monoclonal antibody, is among the most thoroughly researched biologics for nighttime asthma. Omalizumab reduces the release of inflammatory mediators by binding to IgE antibodies and blocking them from adhering to mast cells and basophils. This activity is particularly helpful in lowering the symptoms of asthma at night by calming the allergic reaction that frequently leads to nocturnal exacerbations.
Dupilumab, an anti-IL-4R monoclonal antibody, is another biological treatment that has the potential to treat asthma at night. Airway inflammation and hyperresponsiveness are strongly encouraged by interleukin-4 (IL-4). Asthma flare-ups are significantly decreased, and lung function is enhanced, due to dupilumab's ability to block the signalling of both IL-4 and IL-13. By treating the underlying inflammatory processes that contribute to nocturnal attacks, this focused strategy can help reduce the symptoms of asthma at night.
Additionally, the biologics mepolizumab and benralizumab address eosinophilic asthma, a subtype of severe asthma marked by high eosinophil counts in the airways. Immune cells called eosinophils are crucial in the inflammation that occurs with asthma, and their hyperactivity is frequently linked to nighttime exacerbations. These biologics have demonstrated efficacy in reducing nighttime asthma symptoms and enhancing sleep quality for those who suffer from it by lowering eosinophil levels and reducing airway inflammation.
Biologic medicines have their limitations when used to treat asthma at night. First, accessibility is a challenge due to their cost, which is frequently more than that of conventional asthma treatments. Second, not all patients with nocturnal asthma are good candidates for biologic therapy since eligibility requirements are frequently strict and necessitate in-depth assessment. Additionally, the long-term safety data for these drugs are continuously developing, calling for constant monitoring.
Continuous Positive Airway Pressure (CPAP): Continuous Positive Airway Pressure (CPAP) is a widely recognised and effective therapy primarily used for the management of obstructive sleep apnea (OSA). However, its role in nighttime asthma has also garnered attention in recent years. The capacity of CPAP to reduce airway blockage is an essential component of its function in nighttime asthma. Asthma is characterised by bronchoconstriction, in which the airways narrow as a result of inflammation and smooth muscle contraction. People are more prone to airway closure while sleeping because the muscles that keep the airways open relax. By maintaining a consistent stream of air, CPAP prevents this from happening and ensures a steady, unhindered airflow.Additionally, CPAP enhances the general quality of sleep in those with nighttime asthma. Patients with asthma frequently experience poor sleep, which impairs lung function and increases daily weariness. CPAP aids people in getting deeper and more restful sleep by regulating breathing patterns and lowering the rate of nocturnal awakenings brought on by asthma symptoms. An improvement in overall well-being and a reduction in daytime asthma symptoms result from better sleep quality.
By reducing allergy exposure, which leads to asthma episodes at night, CPAP aids in the management of asthma. In the bedroom, it's common to find allergens like dust mites, pollen, and pet dander. Filter-equipped CPAP machines help clean the air, lowering the amount of allergens which a person inhales while sleeping. The likelihood of overnight asthma exacerbations brought on by allergens is decreased, which is especially helpful for people with allergic asthma.
What are the factors that contribute to nighttime asthma attacks?
Nighttime asthma attacks are a common and challenging aspect of asthma management. Various factors contribute to these attacks, including circadian rhythms, reduced medication efficacy, environmental triggers, GERD, psychological factors, symptom awareness, inadequate asthma management, seasonal and environmental factors, respiratory infections, and obesity.
Triggers in the sleep environment: Nighttime asthma attacks are significantly influenced by the sleeping environment. Dust mites, cat dander, mould, and tobacco smoke are the allergens and irritants that cause asthma symptoms and attacks in the bedroom. Since these factors are frequently concentrated inside, the bedroom is potentially a hotspot for asthma flare-ups at night.
In addition, poor ventilation and excessive humidity levels in the bedroom foster an environment that encourages the growth of mould and allergens, aggravating asthma symptoms. A crucial first step in minimising asthma attacks at night is to ensure a clean and allergen-free sleeping environment.
Psychological factors: It is well known that stress and anxiety worsen asthma symptoms, and they are especially challenging at night. People with asthma worry about the risk of nighttime episodes, making the evening an extremely sensitive time for them. Asthma symptoms develop as a result of this anxiety, which leads to a vicious cycle of anxiety and asthma exacerbation.
Stress and anxiety interfere with sleep cycles, which results in poor sleep and raises the chance of asthma episodes at night. For better asthma control at night, stress management techniques, cognitive-behavioural therapy, and stress-reduction methods are extremely helpful.
Lack of symptom awareness: Lack of symptom awareness while sleeping is another issue that contributes to asthma episodes at night. Asthma sufferers do not always become aware when their symptoms intensify, which causes a delay in administering emergency drugs. This delayed response causes asthma attacks to worsen before being treated.
Additionally, due to changes in respiratory feeling, some people perceive their asthma symptoms less strongly while they are sleeping. As a result, one underestimates the condition's severity and fails to take the necessary steps when they should. Asthma sufferers become more aware of their overnight symptoms and take immediate action to stop attacks by educating themselves and self-monitoring.
Inadequate asthma management: In order to prevent asthma episodes at night, effective asthma treatment is essential. A lack of regular medical follow-ups and the improper use of controlled drugs are examples of inadequate management. When asthma is poorly managed, it is more prone to flare up at night because a number of aggravating factors are present.
In addition, some people do not fully comprehend the triggers that cause their asthma or do not have the required knowledge on how to manage the condition. Optimising asthma management and lowering the risk of nighttime episodes require thorough asthma education and regular engagement with healthcare professionals.
Environmental factors: The season and environment have an impact on asthma symptoms, particularly midnight episodes. Asthma symptoms are impacted by pollen, air pollution, temperature and humidity changes. Seasonal allergens like pollen are more common at various times of the year, which makes asthma symptoms worse at night for people who are sensitive to these allergens.
High levels of air pollution in cities make asthma symptoms worse, especially at night. Wintertime air that is chilly and dry irritates the airways and results in asthma attacks. It is possible to lessen the frequency of nighttime asthma attacks by being aware of the environmental factors that influence asthma symptoms and adopting appropriate safety measures, such as utilising air purifiers or staying indoors during times of heavy pollution.
Respiratory Infection: The symptoms of asthma are considerably exacerbated by respiratory infections like the flu and the common cold, and the likelihood of nighttime attacks rises. Breathing becomes more difficult as a result of infections that lead to mucus formation and airway inflammation. Asthma symptoms worsen at night due to the coughing and congestion that come with respiratory infections and keep people from falling asleep.
Obesity: Obesity is a known asthma risk factor, and it leads to asthma attacks at night. Weight gain worsens asthma symptoms by causing the body's tissues, especially the airways, to become more inflamed. Additionally, obesity impairs lung function and lessens one's capacity to adequately expel air, which might exacerbate symptoms at night.
What are the complications of Nighttime Asthma?
Listed below are some common complications of nighttime asthma:
Sleep disturbance
Sleep problems are one of the most noticeable complications of nocturnal asthma. Numerous factors, including alterations in lung function, hormonal changes, and environmental triggers like dust mites and pet dander, contribute to the worsening of asthma symptoms during the night. Repeated awakenings, trouble going back to sleep, and generally poor sleep quality are caused by these exacerbations. Chronic sleep deprivation has negative impacts on physical and mental health over time, which compromises daily functioning and general well-being.
A common side effect of the sleep disruption brought on by nighttime asthma is fatigue and drowsiness during the day. A person's productivity at work or school may suffer if they have nighttime asthma as they find it difficult to stay awake and alert throughout the day. In addition to impairing concentration and memory, this chronic fatigue increases the likelihood of accidents and injury.
Impaired physical health
An individual's physical health suffers as a result of nighttime asthma. Over time, nighttime asthma attacks might cause a deterioration in lung function due to their frequency and severity. The risk of long-term problems such as chronic obstructive pulmonary disease (COPD) is increased by the ongoing inflammation and constriction of airways, which result in permanent damage. Furthermore, poorly managed nocturnal asthma results in more frequent exacerbations, raising the danger of hospitalisation and respiratory failure.
Stress and anxiety
Having asthma at night is emotionally upsetting. Increased worry and emotional stress result from the dread of having sudden, severe asthma attacks in the middle of the night. When someone has nocturnal asthma, they experience anticipatory anxiety, which makes them nervous about going to bed because they worry about the start of their symptoms. Since stress and anxiety cause asthma attacks, this emotional discomfort may lead to a cycle of worsening symptoms.
Decreased quality of life
Nighttime asthma significantly diminishes an individual's quality of life. The constant struggle to breathe, disrupted sleep, and emotional distress lead to a decreased sense of well-being. People with nighttime asthma may limit their physical activities due to fear of triggering symptoms, leading to social isolation and a decreased ability to participate in normal daily activities.
Economic burden
Nighttime asthma difficulties have a major financial impact. Asthma exacerbations result in frequent hospitalisations, visits to the ER, and missed days of work or school, which result in high healthcare expenses and decreased productivity.
Risk of severe asthma attacks
Uncontrolled nocturnal asthma raises the chance of serious, potentially fatal asthma attacks. These episodes, which include significant breathing difficulties and low oxygen levels, call for serious medical treatment, such as mechanical ventilation. When symptoms are frequently at their worst at night, there is a heightened risk of having a severe asthma attack.
Comorbidities
Nighttime asthma is associated with an increased risk of comorbidities, which are other health conditions that coexist with asthma. These comorbidities include obesity, sleep apnea, and gastroesophageal reflux disease (GERD). Managing these extra health issues on top of the nighttime asthma can be difficult and exacerbate the state of overall health.
What are the home remedies for Nighttime asthma without inhalers?
Listed below are some home remedies and lifestyle changes that help to manage this condition:
Maintain a clean sleep environment: Exposure to allergens and irritants is one of the main causes of nocturnal asthma. Make sure the bedroom is allergen-free and clean to help reduce this. Regularly clean the carpets, curtains, and beds. In order to reduce airborne allergens, consider using an air purifier with a HEPA filter and investing in allergen-proof pillow and mattress covers.
Raise your head while sleeping: Raising the head while sleeping helps prevent acid reflux, which exacerbates asthma symptoms at night. You can do this by using an additional pillow or an adjustable bed. The oesophagus and airways are protected from stomach acid by maintaining this elevated position.
Eliminate allergens: Dust mites are a frequent allergen that causes asthma attacks at night. In order to eliminate dust mites, wash your bedding frequently in hot water, and cover pillows and mattresses with allergen-resistant fabric. Avoid having carpets or cuddly animals in the bedroom because they harbour dust mites.
Maintain proper hydration: Good hydration is crucial for maintaining overall respiratory health. Enough water consumption assists mucus in staying thin and maintaining the airways clear of obstruction. However, In order to minimise overnight awakenings, avoid consuming large amounts of fluids shortly before bed.
Use a humidifier: Dry air makes asthma symptoms worse, particularly during the colder months. By introducing moisture to the air in the bedroom, a humidifier helps keep the airways moist and lowers the chance of developing asthmatic attacks at night.
Use relaxation techniques: Asthma symptoms are influenced by anxiety and stress. Reduce stress and improve the quality of sleep by using relaxation techniques like yoga, progressive muscle relaxation, or deep breathing exercises.
Aromatherapy: Using essential oils helps some people get respite from their asthma symptoms at night. When used in a diffuser, oils like lavender and eucalyptus, aid in opening airways and encourage relaxation.
Herbal treatments: Some herbal treatments, including ginger and turmeric, contain anti-inflammatory characteristics that could help reduce the symptoms of asthma. Prior to including herbal supplements in your asthma management strategy, you should speak with a healthcare professional because they may interact negatively with other prescriptions or have unfavourable side effects.
Breathing exercises: Practising breathing exercises like pursed-lip breathing and diaphragmatic breathing help improve lung function and reduce asthma symptoms, especially when done regularly.
Sleeping position: Some individuals with nighttime asthma find relief by sleeping in specific positions. For instance, sleeping on your side rather than your back may help keep the airways more open.
Does Melatonin improve sleep in Nighttime Asthma?
Sleep is a fundamental aspect of human life, essential for overall well-being and cognitive functioning. However, in today's fast-paced world, many individuals struggle with sleep disturbances like nighttime asthma, which significantly impact their quality of life. Melatonin, a hormone produced by the pineal gland, has gained popularity as a natural remedy for sleep-related issues.
The hormone melatonin is essential for controlling the circadian rhythm, which is commonly known as the sleep-wake cycle. It is largely created and released in reaction to darkness by the pineal gland, which is a small gland situated in the brain. Melatonin levels in the body rise naturally in the evening to help the body get ready for sleep and fall in the morning to indicate awake.
The body receives a signal from melatonin that it is time to go to sleep. This is achieved by interacting with particular receptors in the brain, especially the suprachiasmatic nucleus (SCN) in the hypothalamus. The SCN functions as the body's biological clock and reacts to environmental stimuli like light and dark to control the sleep-wake cycle.
The pineal gland releases melatonin into the bloodstream when the SCN signals that it is time for nighttime. People more easily fall asleep because of this increase in melatonin levels, which serves to lower awareness and promote relaxation. Melatonin production declines as dawn comes near and light levels rise, letting the body know it is time to get up and become more aware.
Due to its pivotal role in sleep regulation, melatonin has become a popular over-the-counter supplement for those struggling with sleep difficulties. Melatonin supplements are available in various forms, including pills, gummies, and liquid drops. These supplements are often marketed as a natural and safe solution to improve sleep quality.
The effects of melatonin on asthma go beyond sleep regulation because it has anti-inflammatory, antioxidant, and possibly bronchodilatory characteristics. Clinical trials have revealed encouraging outcomes when it comes to melatonin supplementation's ability to improve sleep quality and lessen asthma symptoms at night. To fully demonstrate its effectiveness and safety, however, more research is required.
People with nocturnal asthma should speak with their doctors about whether melatonin is used as part of their asthma management strategy. To maximise the potential advantages of melatonin while reducing any risks or side effects connected with its use, careful consideration of dose, timing, and individual reaction is necessary. As our knowledge of the connection between melatonin and nighttime asthma grows, melatonin may be a useful tool for helping people with this difficult condition sleep better and live better overall.

Does a humidifier help to prevent Nighttime Asthma?
The purpose of humidifiers is to add more moisture to the air in a space. They operate by dispersing water vapour into the atmosphere, which can assist in preventing dryness and preserving a pleasant relative humidity. Many people look to humidifiers as a viable treatment for reducing the symptoms of asthma at night.
Through the addition of moisture to the air, humidifiers are able to lessen airway discomfort and dryness. The additional moisture makes it easier for those with asthma to breathe at night. Some people discover that breathing is simpler due to their airways being relaxed by humidified air. This relaxation lessens the severity of asthma symptoms or lowers their likelihood. The mucus discharges in the airways become thinned with the help of proper humidity levels. As a result, there is less chance of overnight episodes of asthma and improved mucus clearance in affected people.
Although the potential benefits of utilising humidifiers to manage asthma symptoms at night look encouraging, it is important to carefully review the scientific data to establish their efficacy. The findings of research on this subject have been conflicting, and individual differences may exist in how humidifiers affect asthma. Here is a summary of some significant studies and conclusions:
A 2011 study that was published in the journal "Paediatric Allergy and Immunology" looked into the use of humidifiers in kids who have asthma. According to the study, some children's lung function improved and humidifier use was linked to a lower likelihood of overnight asthma symptoms. However, the results differed for each participant, indicating that personal reactions vary.
It's important to keep the humidity level inside at the proper amount. While too much humidity encourages the formation of dust mites and mould, on the other hand, too much dry air aggravates asthma symptoms. The "American Journal of Respiratory and Critical Care Medicine" reported a 2013 study indicating both high and low humidity levels were linked to an increased risk of asthma symptoms. Therefore, achieving the ideal humidity balance is crucial.
One of the potential benefits of using a humidifier is reducing airborne allergens that trigger asthma symptoms. Humidifiers may help dust settle, making it less likely to become airborne. However, the effectiveness of this approach varies depending on the specific allergens present in the environment.
It's important to recognise that asthma is a highly individualised condition, and what works for one person does not work for another. Some individuals with asthma find relief from using a humidifier, while others do not experience any significant benefit.
Here are some crucial concerns and best practices to keep in mind if you or a loved one are considering using a humidifier to treat asthma symptoms at night:
Consult a Healthcare Professional: It's important to speak with a healthcare professional, such as an allergist or pulmonologist, before utilising a humidifier as part of the asthma management strategy. They can assist in determining whether a humidifier is an appropriate choice for the particular asthma triggers and symptoms you experience.
Select the Correct Type of Humidifier: There are various humidifier types, including warm mist, cold mist, evaporative, ultrasonic, and more. It's critical to select a type that fits your needs and tastes because each type has benefits and drawbacks.
Maintain Good Hygiene: In order to stop mould and germs from growing, the humidifier must be properly maintained. To prevent it from becoming a cause of indoor air pollution, it is vital to routinely clean and disinfect the humidifier's water reservoir and components.
Monitor Indoor Humidity Levels: Invest in a hygrometer to keep track of indoor humidity levels. In order to remain comfortable and avoid exacerbating asthma symptoms, plan for an indoor relative humidity level of 30% to 50%.
Address Other Triggers: While a humidifier helps with humidity levels and allergy control, it's important to address other asthma triggers in the surroundings. This entails using mattress coverings and pillows that are allergen-proof, performing routine cleaning, and limiting exposure to irritants like tobacco smoke.
In conclusion, humidifiers are helpful for those with nighttime asthma, particularly as they add moisture to the air and lessen airway inflammation. However, the effectiveness of humidifiers in managing asthma differs from person to person, and there is inconclusive scientific data to support their usage. Consult with a healthcare professional before using a humidifier as part of your asthma management strategy, and keep a close eye on how it affects your symptoms. A thorough strategy for controlling nocturnal asthma must also involve maintaining ideal indoor humidity levels and addressing other asthma stressors in the surroundings.









 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews