What does an inhaler do for someone without asthma?


Related products

Inhalers are commonly prescribed to individuals with asthma to help manage their symptoms and improve their quality of life. Asthma affects people differently, with variations in severity and triggers, and proper management is crucial to reduce symptoms and prevent serious, potentially life-threatening attacks. However, the effects of inhalers on individuals without asthma are not widely understood, and people wonder what an inhaler does for someone without asthma. The article aims to explore the potential effects and implications of inhaler use for individuals without asthma who don’t suffer from an asthma attack. Expert opinions, research findings, and real-world scenarios are considered to provide a comprehensive understanding of this topic. While this article is specific to the topic of asthma inhalers, one can find a definitive guide on Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments.
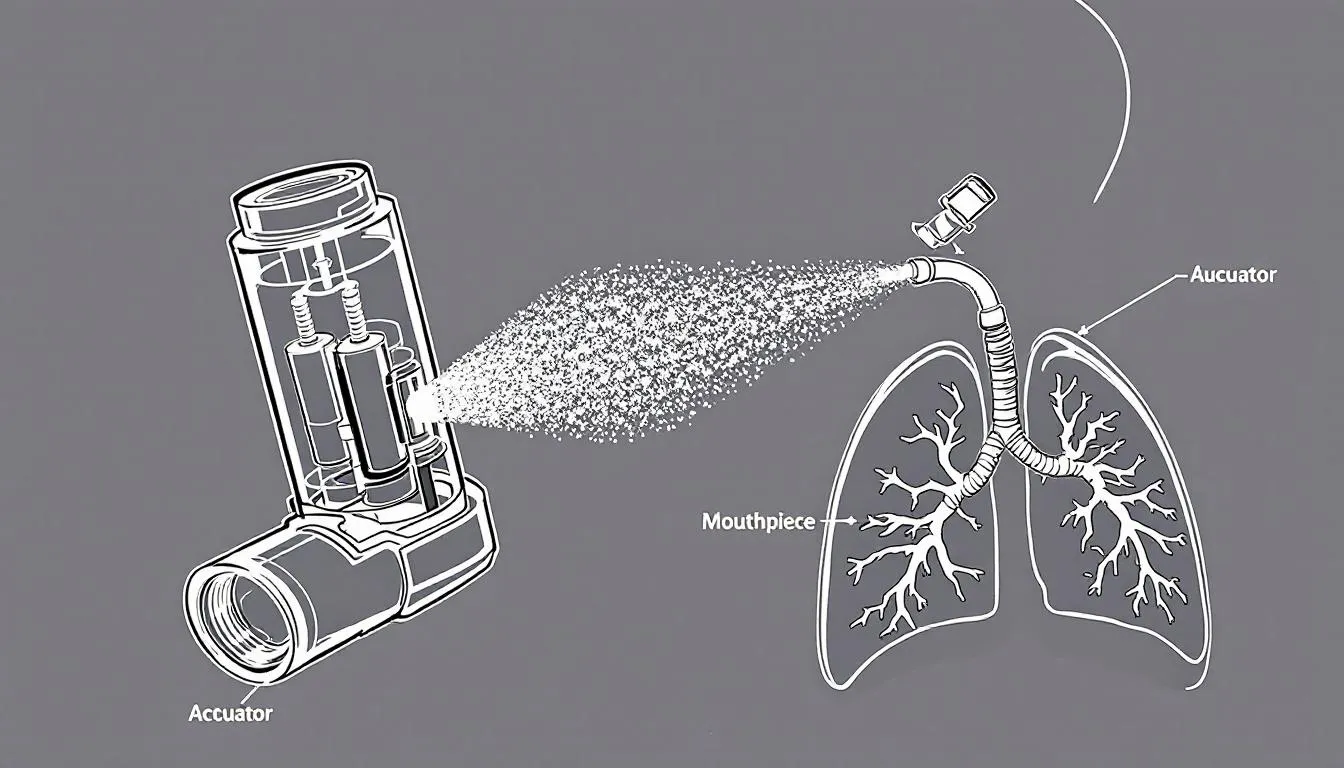
Introduction to Inhalers
Inhalers are a vital component of asthma treatment, designed to deliver medication quickly and effectively to the lungs, where it is needed most. By targeting the airways directly, inhalers help reduce inflammation, relieve bronchospasms, and prevent asthma symptoms such as wheezing, coughing, chest tightness, and shortness of breath.
This targeted delivery system ensures that the medication bypasses the digestive system, allowing for faster onset and fewer systemic side effects compared to oral medications. The rapid action of certain inhalers makes them especially useful during acute asthma episodes, where every second counts in relieving restricted airflow.
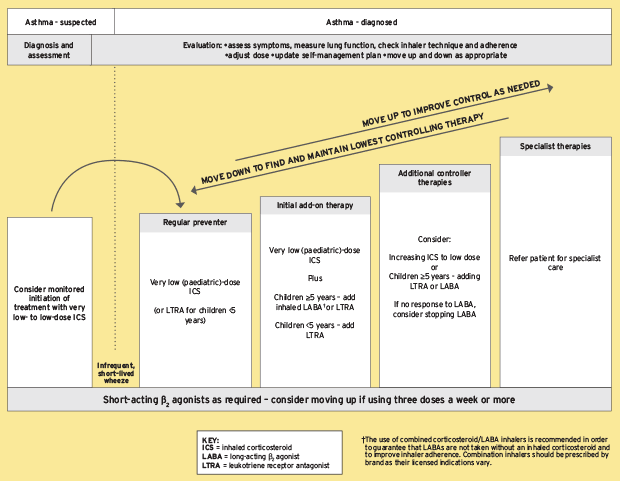
There are several types of inhalers, each serving a specific purpose in managing asthma, allergic reactions, and other lung conditions such as chronic obstructive pulmonary disease (COPD). Preventer inhalers, typically containing corticosteroids, are used regularly to reduce inflammation and airway sensitivity, making them especially important for individuals who experience frequent or severe symptoms.
Reliever inhalers, often referred to as rescue inhalers, provide rapid relief by quickly widening the airways during an asthma attack or when symptoms flare up due to environmental triggers like pollen, smoke, or exercise. These inhalers usually contain a short-acting beta agonist (SABA) such as salbutamol, which helps to ease breathing within minutes.
Combination inhalers offer both long-term control and immediate relief by combining two types of medication—typically an inhaled corticosteroid and a long-acting bronchodilator. These are often prescribed for patients with more persistent asthma symptoms or those who do not respond well to single-medication inhalers.
Using inhalers correctly and as prescribed by a healthcare professional is essential for managing asthma effectively, reducing the frequency and intensity of flare-ups, and improving overall quality of life. Improper inhaler technique is one of the most common reasons for poor asthma control, highlighting the importance of proper patient education and regular check-ins with a GP or asthma nurse.
Understanding Asthma
Asthma is a chronic respiratory condition that affects the airways in the lungs, causing them to become inflamed, swollen, and narrowed. This results in recurring episodes of wheezing, coughing, chest tightness, and shortness of breath. Asthma symptoms can range from mild to severe and may vary in frequency, making it a highly individualised condition.
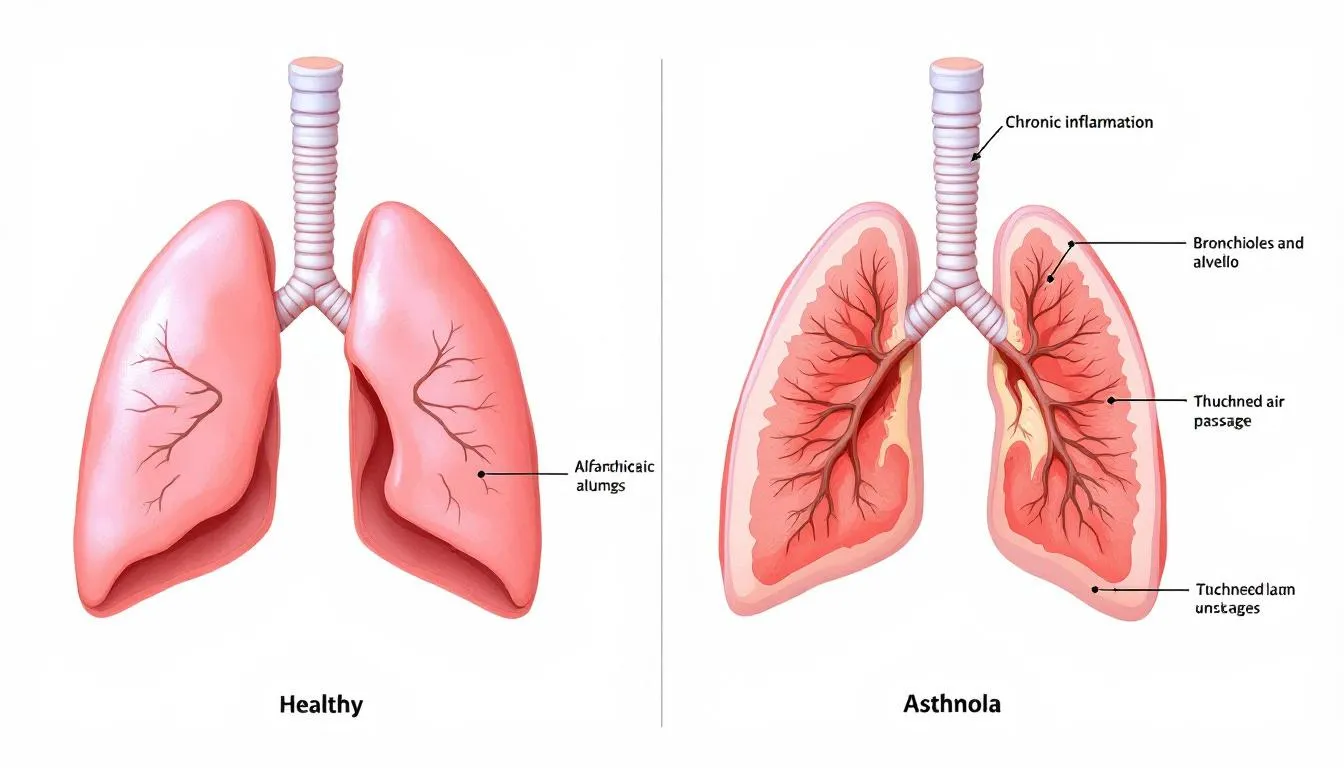
These asthma symptoms can be triggered by a wide variety of internal and external factors, including exposure to allergens (such as pollen, mould spores, and dust mites), viral respiratory infections, physical activity, cold air, tobacco smoke, pet dander, and even emotional stress. Air pollution and occupational irritants such as chemical fumes or industrial dust are also known contributors to asthma exacerbations.
For some individuals, developing asthma is influenced by a combination of genetic predisposition and environmental exposures. Children with a family history of asthma or allergies are more likely to develop the condition, and early-life respiratory infections may also play a role.
People with asthma may experience more severe symptoms if they have allergic asthma, which is triggered by allergens like pollen, or if they suffer from non-allergic asthma, which may be exacerbated by infections or physical activity. Late-onset asthma is another form that typically appears in adulthood, often without a clear allergic cause.
Understanding what triggers asthma attacks is crucial for effective asthma management. Identifying these triggers through peak flow monitoring, allergy testing, or keeping a symptom diary can help individuals and healthcare professionals tailor a treatment plan that minimises exposure and reduces the risk of attacks.
By recognising and avoiding these asthma triggers, individuals can reduce the frequency and severity of symptoms, improve lung function, and maintain better control over their chronic respiratory condition. This not only leads to fewer emergency situations and hospital visits but also improves day-to-day well-being and physical activity tolerance.
For additional support, some people explore supplements that may help maintain respiratory and immune health, such as Source Naturals Wellness Formula – Advanced Immune Support.
Preventing Asthma Attacks: Strategies That Work
Preventing asthma attacks involves more than simply using medication—it requires a proactive and individualised asthma management plan. People with asthma should aim to avoid common asthma triggers such as cold air, pet dander, tobacco smoke, dust mites, and viral respiratory infections. Creating a personal asthma action plan with a healthcare provider helps monitor symptoms and take early action when asthma symptoms worsen. Tools like a peak flow meter can help track lung function and signal when asthma is getting worse. Regular use of a preventer inhaler can reduce inflammation in the airways and lower the risk of severe asthma attacks. By recognising and avoiding triggers early, individuals can improve their breathing, reduce asthma symptoms, and avoid life-threatening flare-ups.
The Role of Breathing Exercises in Asthma Management
In addition to prescribed asthma medications and inhalers, breathing exercises are increasingly recognised as effective tools for improving respiratory function and reducing asthma symptoms. While not a substitute for pharmacological treatment, these techniques can help individuals gain better control over their breathing patterns, especially during periods of stress or mild asthma flare-ups.
Controlled breathing helps reduce airway hyperresponsiveness, enhance oxygen uptake, and promote a sense of calm during episodes of breathlessness. This is particularly beneficial for individuals who experience exercise-induced asthma, anxiety-related breathing issues, or nocturnal asthma symptoms.
Common techniques include:
-
The Buteyko Method: A structured breathing retraining programme that focuses on reduced breathing rates and breath-holding exercises to improve carbon dioxide tolerance and reduce hyperventilation.
-
Pursed-lip breathing: Often used to increase exhalation time and reduce breathlessness, this technique is especially helpful during physical activity or during a sudden asthma flare.
-
Diaphragmatic breathing (also known as belly breathing): Encourages deeper, more efficient use of the diaphragm, which supports lung expansion and reduces shallow chest breathing.
Incorporating breathing exercises into a daily asthma management routine can help lower reliance on reliever inhalers and improve overall quality of life. Breathing retraining may also assist in reducing airway resistance and improving lung capacity, two important metrics for people with persistent asthma.
It's important to work with a respiratory therapist or qualified asthma nurse to learn these techniques correctly and ensure they are suited to the individual's asthma profile. When used alongside peak flow monitoring, medication, and trigger avoidance, these methods can contribute to a more comprehensive and balanced asthma treatment plan.

Types of Inhalers for Asthma and Chronic Obstructive Pulmonary Disease (COPD)
Asthma and COPD are two chronic respiratory conditions that often require the long-term use of inhalers for management and symptom control. These devices are designed to deliver medication directly to the lungs, allowing for faster and more targeted relief than oral medications. Each type of inhaler has a specific purpose, mechanism of action, and ideal use case, making it crucial to understand their differences, particularly when considering their effects on individuals without asthma.
Short-acting bronchodilators for the relief of asthma symptoms
-
Beta-Agonists (e.g., Salbutamol / Albuterol)
Short-acting beta-agonists (SABAs), such as salbutamol (commonly known as albuterol in the US), are considered "rescue inhalers" and are typically used to treat sudden asthma symptoms or asthma attacks. These inhalers work by relaxing the smooth muscles around the airways, which helps to quickly open the air passages and improve airflow.
According to Dr Richard Beasley, Director of the Medical Research Institute of New Zealand, salbutamol is one of the most effective medications for rapidly relieving bronchospasm. In people without asthma, however, the use of a SABA may still cause bronchodilation, but with limited respiratory benefit. Side effects such as an increased heart rate, trembling hands, restlessness, or mild anxiety are more likely in healthy individuals because the medication stimulates beta-adrenergic receptors throughout the body, not just in the lungs.
It’s also worth noting that medications like beta blockers, which are used to treat high blood pressure and heart conditions, can worsen asthma symptoms by triggering bronchospasm. For this reason, healthcare providers must consider a patient’s full medical profile before prescribing certain medications.
-
Anticholinergics (e.g., Ipratropium)
Short-acting anticholinergic inhalers such as ipratropium bromide are another option for immediate symptom relief. These work by inhibiting acetylcholine, a neurotransmitter responsible for constricting the airways—thereby promoting relaxation of airway muscles and reducing mucus production.
Dr Richard Casaburi, a pulmonologist at the Los Angeles Biomedical Research Institute, explains that while ipratropium is effective for asthma and COPD patients, its use in healthy individuals without respiratory conditions offers negligible benefit. Although some bronchodilation may still occur, it does not translate into meaningful improvement in breathing or lung performance for non-asthmatics. In fact, unnecessary use could potentially cause side effects such as dry mouth, dizziness, or blurred vision.
Long-Acting Bronchodilators: Maintenance Therapy Inhalers
-
Beta-Agonists (e.g., Salmeterol, Formoterol)
Long-acting beta-agonists (LABAs), including salmeterol and formoterol, are designed for ongoing asthma and COPD management. These medications are not used for acute symptom relief but rather to maintain open airways over a 12–24 hour period. LABAs are typically used alongside corticosteroids to control chronic symptoms and reduce the frequency of asthma exacerbations.
Dr Nicola Hanania, a pulmonologist at Baylor College of Medicine, advises that LABAs should never be used alone in asthma treatment due to the risk of worsening inflammation. In individuals without asthma, the use of LABAs may still cause systemic effects, such as heart palpitations, muscle tremors, and nervousness, without offering clinical benefits.
The prolonged stimulation of beta receptors in a healthy respiratory system is not only unnecessary but may also mask symptoms of underlying conditions if used without a proper diagnosis.
-
Anticholinergics (e.g., Tiotropium)
Tiotropium is a long-acting anticholinergic bronchodilator most commonly prescribed for COPD. It functions by providing extended relaxation of airway muscles and decreasing mucus secretion. For COPD patients, tiotropium helps improve airflow, reduce flare-ups, and enhance quality of life.
Dr Don Sin, Professor of Medicine at the University of British Columbia, highlights that although tiotropium may induce some bronchodilation in non-asthmatics, its clinical value in this population is unclear. Additionally, inappropriate use may lead to unwanted side effects such as dry mouth, constipation, or urinary retention.
For people without asthma or COPD, the risk-to-benefit ratio of using long-acting bronchodilators like tiotropium is skewed heavily toward potential harm rather than benefit.
Inhaled Corticosteroids (ICS): Anti-Inflammatory Inhalers
Examples: Budesonide, Fluticasone, Beclometasone
Inhaled corticosteroids are considered the cornerstone of long-term asthma control. These medications reduce inflammation, swelling, and mucus production in the airways, helping to prevent asthma symptoms and improve lung function over time.
Dr Fernando Holguin, Director of the Asthma Clinical and Research Program at the University of Colorado, explains that regular use of ICS can significantly reduce asthma attacks and hospitalisations in patients with moderate to severe asthma. However, in individuals without underlying inflammation or airway hypersensitivity, inhaled corticosteroids do not provide measurable improvements in respiratory function.
Moreover, chronic use of ICS without medical need may suppress local immune response in the lungs, increasing the risk of oral thrush (candidiasis), hoarseness, or even pneumonia in rare cases.
Combination Inhalers: Dual-Action Devices
Examples: Fluticasone/Salmeterol, Budesonide/Formoterol
Combination inhalers contain both an inhaled corticosteroid and a long-acting bronchodilator, offering anti-inflammatory action alongside sustained bronchodilation. These are typically prescribed for individuals with more severe or persistent asthma symptoms who require both prevention and maintenance therapy.
According to Dr Sally Wenzel, Director of the University of Pittsburgh Asthma Institute, these inhalers simplify treatment regimens and improve adherence, especially in patients with fluctuating symptom control. However, for people without asthma or COPD, there is no clinical justification for using such combinations. The medications may still induce systemic effects like shakiness, palpitations, or hormonal imbalances without treating any underlying disease.
Can Inhalers Be Used to Treat Other Breathing Problems?
Inhalers are not only used for asthma but are also an important treatment option for a range of lung conditions, including chronic obstructive pulmonary disease (COPD) and bronchitis. You can learn more about the difference between asthma and COPD in our detailed guide. There are different types of inhalers available, such as dry powder inhalers, metered-dose inhalers, and nebulisers, each designed to deliver medication in a way that best suits the patient’s needs. Using an inhaler correctly is essential to ensure the medication reaches the lungs effectively and provides the intended relief. Working closely with a healthcare provider is key to selecting the most appropriate inhaler and developing a treatment plan tailored to individual lung conditions. Proper inhaler technique and regular follow-up with a healthcare provider can make a significant difference in managing chronic obstructive pulmonary disease and other respiratory illnesses.
While asthma is the most common condition treated with inhalers, they are also prescribed for other breathing problems, including exercise-induced bronchoconstriction, chronic bronchitis, and airway inflammation due to allergies. However, using a reliever inhaler or preventer inhaler without a confirmed diagnosis can increase the risk of side effects or mask serious underlying conditions. Those looking to support their breathing naturally can also explore our full range of lung health supplements and breathing support to complement lifestyle changes and expert care.

Effects of Inhalers on Individuals Without Asthma
Potential physiological effects
-
Bronchodilation and increased airflow
Inhalers containing bronchodilators may cause bronchodilation and increased airflow in non-asthmatic individuals, but the overall impact on lung function is likely minimal. A study by Al-Alawi et al. (2005) found that administering albuterol to healthy individuals resulted in only a modest improvement in lung function. Peak flow, which measures how quickly a person can exhale, is often used to assess lung function. A peak flow meter is a simple, handheld device that allows individuals to monitor their lung function at home and can assist in diagnosing asthma.
Peak flow, which measures how quickly a person can exhale, is often used to assess lung function. While inhalers and peak flow meters require medical supervision, some individuals explore respiratory support supplements like Jarrow Formulas NAC Sustain 600mg, which contains N-acetylcysteine — a compound shown to help support antioxidant defence in the lungs and reduce oxidative stress.
-
Reduced airway inflammation (for corticosteroids)
Inhaled corticosteroids are unlikely to have a significant effect on airway inflammation in individuals without asthma, as they are specifically designed to target the underlying inflammation present in asthmatic airways. Inhaled steroids are available as dry powder inhalers and sprays to assist with breathing difficulties, persistent cough and other symptoms of asthma attacks.
-
Possible side effects (e.g., increased heart rate, tremors)
As mentioned earlier, the use of inhalers in individuals without asthma may lead to side effects such as increased heart rate, tremors, or feelings of nervousness. These side effects are generally mild and short-lived, but might be concerning for some individuals.
Possible scenarios for inhaler use in non-asthmatics
-
Exercise-induced bronchoconstriction
Exercise-induced bronchoconstriction (EIB) is a condition in which the airways narrow during or after exercise, leading to shortness of breath, coughing, or wheezing. , states that individuals with EIB may benefit from using an inhaler containing a short-acting bronchodilator, even if they do not have asthma, as stated by Dr. James Hull, a sports medicine specialist at the Royal Brompton Hospital in London. However, it is crucial to obtain a proper diagnosis and prescription from a healthcare professional.
-
Chronic obstructive pulmonary disease (COPD)
Individuals with COPD may be prescribed inhalers containing bronchodilators or inhaled corticosteroids to manage their symptoms. Although COPD is a separate condition from asthma, the use of inhalers in individuals with COPD may provide symptom relief and improved lung function.
-
Other respiratory conditions
In rare cases, inhalers may be prescribed for other respiratory conditions, such as bronchiectasis or cystic fibrosis. However, these situations are uncommon, and the use of inhalers for non-asthmatic respiratory conditions must be guided by a healthcare professional. For individuals with more severe or difficult-to-control symptoms, other treatment options beyond standard inhalers may be necessary to effectively manage their condition.
Misconceptions and risks of inhaler use in non-asthmatics, including developing asthma
-
Inappropriate self-treatment
Some individuals may attempt to self-treat perceived respiratory issues with inhalers obtained from friends, family members, or other sources without consulting a healthcare professional. The approach is potentially dangerous, as it might result in a delayed or incorrect diagnosis, inappropriate treatment, or adverse effects from the medication.
-
Delayed diagnosis of an underlying condition
Using an inhaler without a proper diagnosis may mask the symptoms of an underlying respiratory condition, leading to a delayed diagnosis and potentially worsening the condition over time.
-
Potential adverse effects and drug interactions
Inhalers potentially have adverse effects, such as increased heart rate, tremors, or feelings of nervousness, and may also interact with other medications. Using an inhaler without a healthcare professional’s guidance increases the risk of experiencing these adverse effects or drug interactions.
Expired inhalers should be returned to a pharmacy for safe disposal rather than discarded in household waste, to minimise environmental impact and ensure safety.
Expert Opinions and Recommendations
Inhaler use in non-asthmatics: medical consensus
-
When it may be appropriate
In some cases, such as exercise-induced bronchoconstriction or other respiratory conditions, using an inhaler may be appropriate for individuals without asthma. However, it is crucial to obtain a proper diagnosis and prescription from a healthcare professional to ensure the inhaler's safe and effective use.
-
When it may be harmful or unnecessary
Using an inhaler without a proper diagnosis and prescription may be harmful or unnecessary. It is able to mask the symptoms of an underlying respiratory condition, delay proper diagnosis and treatment, or cause adverse effects and drug interactions.
Importance of proper diagnosis and treatment
-
Consulting a healthcare professional
If experiencing respiratory symptoms or if an individual suspects they have asthma or another respiratory condition, it is essential to consult a healthcare professional for a proper diagnosis and treatment plan. Different ethnic groups may experience varying asthma prevalence and outcomes, highlighting the need for personalised diagnosis and treatment. Using an asthma inhaler without professional guidance leads to potentially dangerous consequences.
-
Avoiding self-diagnosis and self-treatment
Self-diagnosing and self-treating respiratory symptoms with an inhaler or asthma medications are potentially dangerous, resulting in a delayed or incorrect diagnosis, inappropriate treatment, or adverse effects from the medication. It is essential to consult a healthcare professional for a proper diagnosis and treatment plan.
To learn more about options to treat asthma, visit the buy asthma treatment section.
Understanding the effects of asthma inhalers on individuals without asthma is essential to ensure their safe and appropriate use. While inhalers provide relief for certain respiratory conditions, using them without a proper diagnosis and prescription might be harmful or unnecessary. It is crucial to consult a healthcare professional for an accurate diagnosis and an appropriate treatment plan, along with the recommended prescription medication. The article, written for the Welzo medical information website, has provided a comprehensive understanding of the potential effects and implications of inhaler use in non-asthmatic individuals, drawing on expert opinions, research findings, and real-world scenarios.
Whether using a metered dose inhaler, rescue inhaler, bronchodilator inhaler, dry powder inhaler or other inhalers, it is important to use an inhaler properly when prescribed by a doctor or asthma nurse to most benefit from its use.
Conclusion
Asthma is a chronic condition that requires ongoing management and treatment to prevent severe asthma attacks and improve quality of life. By recognising asthma symptoms, avoiding triggers, and using inhalers correctly, people with asthma can significantly reduce their risk of severe asthma and asthma deaths. It is essential to collaborate with a healthcare provider to develop a personalised asthma action plan and ensure access to the right treatment for asthma. With effective asthma management, including the use of inhalers and other treatments, individuals can prevent symptoms, lower their risk of asthma attacks, and lead active, healthy lives. Reducing asthma deaths and improving outcomes for people with asthma remain key goals in asthma management, highlighting the importance of education, proper treatment, and ongoing support from healthcare professionals.
Frequently Asked Questions (FAQs)
Can I use an inhaler if I don’t have asthma?
Using an inhaler without a diagnosis of asthma is not recommended unless directed by a healthcare provider. Inhalers are designed to treat specific respiratory conditions like asthma or COPD. Misuse can lead to side effects such as a rapid heart rate, nervousness, or masking of underlying issues. Always seek professional medical advice before using an inhaler.
What happens if someone without asthma uses a blue inhaler?
Blue inhalers, also known as reliever inhalers, are designed to provide quick relief from breathing difficulties by relaxing the muscles around the airways. In someone without asthma, they may cause mild effects like bronchodilation, but can also lead to shakiness or palpitations. Their use should be medically justified.
Are inhalers harmful if misused?
Yes. Inappropriate or prolonged use of asthma inhalers, especially without a prescription, can lead to negative outcomes, including dependency, increased risk of side effects, and delay in diagnosis of real health conditions. Expired inhalers can also lose effectiveness and should be disposed of properly at a pharmacy.
Do inhalers help with breathing if you’re healthy?
Not really. While bronchodilators may slightly improve airflow even in healthy individuals, there is typically no meaningful benefit unless there's an underlying issue. Moreover, improper use may cause discomfort or complications.
Is shortness of breath always asthma?
No. Shortness of breath can result from a wide range of issues, including anxiety, cardiovascular conditions, respiratory infections, or allergies. It’s important to get a proper diagnosis rather than self-treating with asthma medications.
References:
-
Medical Research Institute of New Zealand. (n.d.). Dr. Richard Beasley. Retrieved from https://www.mrinz.ac.nz/page/8-welcome
-
Los Angeles Biomedical Research Institute. (n.d.). Richard Casaburi, MD, PhD. Retrieved from https://labiomed.org/richard-casaburi
-
Baylor College of Medicine. (n.d.). Nicola A. Hanania, MD, MS. Retrieved from https://www.bcm.edu/people-search/nicola-hanania-21904
-
University of British Columbia. (n.d.). Don Sin, MD, MPH, FRCPC. Retrieved from https://resp.core.ubc.ca/?page_id=42
-
University of Colorado. (n.d.). Fernando Holguin, MD, MPH. Retrieved from https://medschool.cuanschutz.edu/medicine/divisions/pulmonary/faculty/fernando-holguin
-
University of Pittsburgh Asthma Institute. (n.d.). Sally Wenzel, MD. Retrieved from https://www.upmc.com/services/pulmonology/asthma-institute/meet-our-team
-
Al-Alawi, A., Ryan, E., Avolio, J., & Hughes, J. M. (2005). Inhaled salbutamol (albuterol) vs injected epinephrine (adrenaline) in the treatment of anaphylaxis. The Journal of Allergy and Clinical Immunology, 115(2), S207.
-
Royal Brompton Hospital. (n.d.). Dr. James Hull. Retrieved from https://www.rbht.nhs.uk/specialists
-
Vocal Cord Dysfunction
-
Montelukast, Side Effects and Uses
-
Lung UK. (n.d.). Information and support for individuals with lung conditions, including asthma, and details on treatments such as AIR therapy and MART inhalers. Retrieved from https://www.blf.org.uk/

















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews