Seasonal Asthma: Definition, Causes, Symptoms, Diagnosis, and Treatments

Related products
Seasonal Asthma
Asthma is a chronic respiratory disease characterised by inflammation of respiratory airways resulting in their narrowing, causing symptoms like wheezing, chest tightness, shortness of breath and coughing. Various triggers like allergens, extreme environment etc., trigger it. Some people experience a sudden onset of symptoms in a specific season, particularly in winter and harvesting, due to increased exposure to specific triggers. The symptoms are particularly severe in children and older adults with weak immune systems.
The treatment and prevention need a comprehensive program, including reducing the exposure to the causative risk factors and timely treatment. Besides the clinical signs, some tests like allergy tests, blood tests, exhaled nitric oxide test, spirometry, and bronchial trigger tests are helpful for diagnosis. The treatment options available are inhalers (containing corticosteroids and beta-agonists), bronchodilators, leukotriene modifiers, biologics, mast cells therapy and more advanced options like immunotherapy.
Some home remedies like stress reduction, lifestyle changes and dietary supplements are helpful. These treatments ensure quick relief and treatment; however, some signs like severe chest pain, difficulty in sleeping and speech, blue tint on the fingers and lips, and extreme shortness of breath need immediate medical assistance.
What is Seasonal Asthma?
Seasonal asthma is allergic asthma, whose symptoms and incidence rates are influenced by factors more common in a particular season. It is a chronic condition, and its breakouts in the susceptible season make living very difficult. Unlike the other seasonal allergens, seasonal asthma symptoms are predominantly respiratory in nature.
Seasonal asthma is an allergic response to an offending agent called the allergen. The allergens cause asthma in two phases. In the first phase, the exposure to the allergens causes the blood cells to produce antibodies (IgE). During the second exposure, these antibodies bind to the basophils and mast cells and cause them to release chemicals like histamine, leukotrienes and prostaglandins. These chemicals cause the airways' narrowing and induce asthma symptoms. The immune cells secrete chemicals that attract other immune cells into the lungs causing inflammation.
How common is Seasonal Asthma?
Asthma is a highly common chronic disease in the UK, affecting both the young and adults alike. An estimated 5.22% of people in the UK were diagnosed with asthma (including seasonal asthma) in 2005, according to a national study published in the Journal of the Royal Society of Medicine in 2010. Every person out of nine was diagnosed with some form of coughing asthma, and more than 32 million prescriptions for asthma were issued to the patients in the same year.
The incidence rate in women was slightly higher (5.6 per 1000 women) than in men (4.8 per 1000). The younger babies in the age group 0-4 years showed the highest rate (22.9 per 1000) than the others. The rate decreases gradually with advancing age and becomes relatively stabilised after 15 years of age.
The incidence rate depends upon socioeconomic factors, and the socially and economically deprived people showed higher lifetime prevalence, incidence and a higher rate of prescription of anti-asthmatic prescriptions than those with better financial and social backgrounds. A decreasing trend in the incidence rate, prevalence, hospital admissions, deaths, and prescriptions being issued is observed in people each coming year due to improved socioeconomic factors and health facilities.

How does Seasonal Asthma differ from other Types of Asthma?
There are 2 broader types of asthma, i.e., allergic and non-allergic. Seasonal asthma is an allergic type of asthma, while exercise-induced, drug-induced, and occupational asthma are non-allergic types. Seasonal asthma is different from other types and is related to seasonal factors. Some key differences are;
Triggers: Seasonal asthma is triggered by seasonal factors like a spike in dust allergens in the harvesting season or extreme cold in the winter months. The incidence of seasonal asthma increases in specific months of the year, while that of other types is not influenced by season or time. Occupational asthma is due to exposure to the workplace allergens like dust, fumes, chemicals and gases and is experienced after prolonged exposure to these irritants, irrespective of the season. Likewise, all other types of allergic asthma are experienced in all seasons.
Sensitivity to the allergens: People with seasonal asthma are allergic to certain seasonal allergens like plant pollens, and the immune system reacts after exposure to these seasonal factors. Stronger immune responses occur in certain seasons. People with other types of asthma are not sensitive to seasonal allergens and experience general sensitivity to environmental allergens. The sensitivity to workplace asthma is experienced more at specific workplaces.
Treatment approaches: The treatment approach for seasonal asthma includes using steroids and bronchodilators to manage specific symptoms and staying indoors to prevent exposure to allergens in the high-risk season. The treatment of other types of asthma needs an extensive long-term plan to reduce the signs and prevent future occurrences.
However, the borderline between seasonal asthma and other asthma types is blurred, with many overlapping.
What season does Seasonal Asthma common?
Lifestyle and seasonal factors cause the symptoms and severity of seasonal asthma to change. Generally, winter and fall are the seasons with the highest frequency and flare-ups of seasonal asthma. It is due to increased respiratory infections in the winter, like flu or common cold. These infections spread rapidly in indoor social gatherings that are more common in fall and winter. People tend to spend more time indoors in the winter, resulting in more exposure to the household allergens like pet dander, mould spores and dust mites.
Another factor influencing the seasonality of asthma is the harvesting season in a particular area. The harvesting crops are a significant source of pollen and other plant-based allergens. For example, the grass and tree pollens reach their peak levels in the middle to late spring, and the peak of ragweed pollen is observed in early fall. Any seasonal activity that influences the air quality results in asthma flare-ups. These include cigarette smoke, particularly in crowded places. Monitoring the air quality index (AQI) is helpful, and outdoor activities in areas with an AQI of more than 50-100 must be avoided.
What are the common Causes of Seasonal Asthma?
Seasonal asthma is allergic asthma, which results from the introduction of allergens and the desperate and heroic attempts by the body to keep that allergen at bay. Several risk factors in a given season are responsible. Here are some common factors and triggers that cause seasonal allergic asthma symptoms.
- Exercise: Exercises worsen the symptoms of already occurring seasonal asthma. During workouts, the demands for oxygen by the body are increased, and the body increases the respiration rate to accommodate increased rate. The rate of respiration increases 2-3 times during exercises. It means a person takes in more air than normal and breathes in more allergens.
- Dust mites: Dust mites are tiny and microscopic organisms in indoor settings. Different materials of the dust mites, like droppings, decaying bodies and skeletal proteins, are highly allergic and cause allergic reactions in the lungs when inhaled.
- Pollen: Pollens are very tiny and microscopic particles produced by plants and cause allergic reactions. Different types of pollen, like weed pollen, tree pollen and grass pollen, peak at different times of the year and cause allergic asthma.
- Air pollution: Different air pollutants like sulphur dioxide, carbon dioxide, ozone, carbon monoxide, particle matter etc, trigger asthma attacks. The effect of air pollution on asthma is highly pronounced in children whose respiratory epithelium is naive and sensitive to allergens. Air pollutants increase the risk of respiratory infections, further exacerbating the allergic asthma symptoms.
- Viral infections: Viral infections like flu, cold, COVID-19 and respiratory synctial virus (RSV) are less talked about asthma triggers. However, they cause severe flare-ups. The risk of viral asthma is highest in the cold months when the flu and cold are most common. The common cold or flu is due to 100s of known viruses that cause viral asthma and aggravate seasonal asthma, causing flare-ups. Between 50-80% of the exacerbations in asthma patients are attributed to viral causes.
- Cold air: Freezing and dry air cause bronchoconstriction. It means the body tries to limit the inflow of cold and dry by constricting the airways. The extremely cold air irritates the respiratory membranes causing the production of the same chemicals as produced during typical infections. High temperature and humidity have the same effect and make respiration difficult.
- Mould or mildew: Mold grows in hot and humid places like window seals and water pipes. In regions with hot and humid climates or having such temperatures for longer, mould grows. The mould produced spores that are very potent respiratory allergens.
Exercise
Exercises are the planned physical activities to improve physical fitness and health. Despite benefits, the exercises cause significant stress to the body.
Exercise-induced asthma (EIA) is a type of asthma triggered by vigorous physical exercise or severe physical stress. These activities trigger acute bronchospasm in people having highly reactive airways. The EIA is more common in asthmatic people. However, it is experienced by people with allergic rhinitis and even by ordinary individuals. The EIA is very important as asthma is silent in 50% of people and is apparent only during exercise.
In the EIA, the problem lies in the lower respiratory tract and is experienced by individuals participating in physical activities that have an aerobic component. It is seen in any exercise but is less common in anaerobic workouts. During aerobic exercises, repetitive and consistent air movements occur through the air passages and influence the temperature and humidity in them. It triggers unknown neurochemical and biochemical pathways leading to bronchospasm. In people prone to the EIA, the first 3-5 minutes of physical activities don't cause any issues. The lung functions decrease as soon as the physical activity is stopped.
The levels of forced expiratory volume in 1 second (FEV1) and peak expiratory flow rate (PEFR) decrease within 5-10 minutes of stoppage of physical activity. Once the training is resumed, the symptoms appear within 5-10 minutes of resumption. The symptoms of decreased lung function persist continuously for 15-40 minutes and then normalize, and the lung functions are restored. The values of FEV1 and PEFR during that phase fall by 20-50%. After that phase, a refractory phase of 1-2 hours starts, during which the symptoms are difficult to replicate.
Many factors influence the severity and frequency of EIA, like bronchial sensitivity, low air humidity, frigid air, airborne allergens, and air pollutants like ozone. The condition affects 12-15% of the general population, 35-40% of the people with allergic rhinitis and 90% of those with already ongoing asthma. After excluding the patients, is it still present in 3-10% of the population. It is more experience during cold weather sports, and incidence rates of as high as 35-50% are reported in cross-country skiers, ice hockey players and skaters.
Dust mites
Dust mites are tiny insect-like pests that are present in the house dust. They feed on dander and dead skin cells the animal and humans shed. Their body parts, droppings and proteins are highly allergic.
Exposure to the house dust mite (HDM) is a significant risk factor for allergic rhinitis and asthma. The allergic diseases occur due to an IgE-medicated immune response, causing itching, nasal obstruction, sneezing and rhinorrhea (runny nose). Asthma is more severe in people having allergic rhinitis (AR). So, as the seasons influence the population of house dust mites, the risk of AR and asthma changes. The dust mites cause sensitisation and IgE-medicated immune responses in people.
The dust mite allergens are the proteins which elicit the immune response in the same way as triggered by allergic foods, plant pollens and mould spores. These are microscopic organisms and are found in the carpets, pillows, comforters, sheets and beds in the living room. In the winter, more bedding materials are used, providing hiding places for dust mites. So, more risk of dust mite allergy is found in the winter months. The ideal conditions for these mite species are high humidity and a temperature range of 25-30oC.
Environmental factors like rainfall, relative humidity and temperature influence the mite population. The indoor moisture levels are influenced by factors like the living habits of the people, the age of the house, orientation, ventilation and floor levels. In areas and seasons with high humidity, a large population of dust mites is present mainly on the mattresses and floors. It is responsible for the high burden of dust mite allergy in these areas and seasons.
Seasons influenced the dynamics of the mite population in the homes of asthmatic patients. The majority (48.35%) of the mites were isolated from the samples collected in the rainy season compared to 37.63% from the samples collected in the rainy season and 14.01% from the samples collected in the winter (A study published in the Journal of Medical Entomology in 2018). The dust mites’ increase in hot and humid climates, but the incidence of the disease is more complicated due to the changes in other triggers.
Pollen
Pollen is a powdery substance, primarily yellow and consists of tiny grains produced by the male cone or male part of the flower. Each grain has a male gamete that fertilizes the female gamete once it is
transported to the flower by insects or wind. The pollens are covered by proteins that cause allergic reactions in sensitized people.
The recent increase in the incidence of seasonal asthma and hay fever is attributed to climate change that favours the spread of ragweed throughout continental Europe. Season influences the risk as winter and rainy seasons restrict the movements, resulting in a lack of early exposure to allergens—and prevent the proper development of the immune system. Most of the seasonal allergies and asthma in the North America and Continental Europe start in the spring when the trees develop their flowers and spread the allergic pollens by air. The primary culprit plant species are mountain cedar, birch, oak and many others.
From last summer to early spring, various weeds and allergic grasses like nettle and mugwort emerge and cause another round of symptoms in the sensitized people. The ragweed season starts from the late summer to the first frost. Likewise, an increase in grass pollens is observed in the early fall.
Global climate change influences the risk of seasonal asthma as the increasing levels of carbon dioxide (expected to reach 600 ppm by 2050) favour the growth and pollen production by the ragweed plant.
The growth of pollen allergens is higher in urban areas due to more heat and increased carbon dioxide levels in the cities, which is responsible for higher levels of ragweed and other plant pollens and a higher risk of seasonal asthma. So, the seasonal variations in the growth and proliferation of different plant pollens influence the incidence rate of seasonal asthma and climate change is further expected to add to the misery.
Air Pollution
Air pollution refers to the contamination of air due to the presence of substances that are harmful to human and animal health. The primary sources of urban pollution are power generation and traffic. The pollutants in the outdoor air, like traffic pollutants (e.g., polycyclic aromatic hydrocarbons and heavy metals), gaseous pollutants (sulphur dioxide, carbon dioxide, carbon monoxide, nitrogen dioxide, ozone) and particulate matter cause or exacerbate seasonal asthma.
These air pollutants directly irritate and cause airway inflammation at very high concentrations, but these exposure levels are sporadic in Europe and America. Air lower levels, these pollutants cause inflammation of airways and hyperresponsiveness, the significant attributes of asthma. Exposure to the pollutants like particulate matter, nitrogen dioxide and ozone cause oxidative stress to the respiratory tissues.
The four mechanisms proposed by the UK's Committee on the Effects of Air Pollutants to understand the mechanism of asthma are increased sensitization to airborne allergens, inflammatory pathways, airway remodelling and oxidative stress. The mutations in the genes that regulate these factors increase the risk of seasonal asthma due to air pollutants. The air pollutants suppress the development of immune responses to infectious agents and allergens.
Particulate matter is produced both naturally and by anthropogenic sources. It is divided into three types based on aerodynamic diameter. The coarse PM, with a 2.5-10 µm diameter deposit in large airways and the head, fine PM (PM2.5) deposits in the respiratory tract, and ultrafine PM (diameter less than 0.1µm) deposits in the alveoli. Besides being an irritant, the PM often carries allergens like plant pollens and fungal spores, further aggravating asthma. The particulate matter alone or combined with the airborne allergens causes hypersensitivity of airways, remodeling and oxidative damage to the respiratory tissues.
Exposure to these air pollutants multiplies the risk of and increases the severity of seasonal asthma. A study covering 10 European cities in 2015 observed that 15% of the exacerbations in asthma cases and 14% of new asthma cases in children were attributed to traffic pollution.
Viral Infections
Viruses are microscopic infectious particles that cause diseases and spread from one person to another. Seasonal flu and the common cold are caused by hundreds of known viruses (like influenza) and become very challenging for people struggling to manage asthma. They are among the little talked about but significant triggers of asthma. The risk of seasonal asthma is very high in the winter months due to a high viral load. Around 60-70% of exacerbations of asthma cases in winter are attributed to viral infections. Several seasonal variations in the incidence of asthma are due to viral infections of the upper respiratory tract.
The highest exacerbations (28.8%) are observed in the fall, followed by 19.6% in the spring, 15.9% in winter and 14.5% in the summer. Some vital infections (like HIV) depress the immune response and cause exacerbations of seasonal asthma cases. Viral infections sometimes cause defective eosinophilic inflammation, reduced death of virally infected cells, increased airway responsiveness and dangerous direct diseases.
Various viruses causing an increased risk of asthma and severe symptoms are rhinoviruses (the most common cause of the common cold and seasonal flu), Influenza viruses, respiratory syncytial virus (RSV, prevalent in young children and infants) and the infamous coronavirus (the cause of a recent global pandemic that had killed millions throughout the world). Due to the relationship between viruses and asthma, susceptible people must take strict measures, particularly during the highest risk season, to avoid severe complications.
Cold Air
Cold weather and cold air are triggers of asthma, and the winter season is challenging for people struggling with asthma. Asthmatic people have a low degree of inflammation, always going on inside the airways. It causes the narrowing of airways and hinders the flow of air. The frigid and dry air irritates the air passages and triggers asthma flare-ups. The cold air causes spasms in the tiny muscles in the airways (that keep them open). Extreme cold causes condensation of water vapours in the air, leading to extremely dry air with humidity levels of less than 40%.
The atmospheric temperatures influence the atmosphere's composition, and severe winters cause an increase/ decrease in the concentrations of gases, most notably carbon dioxide, carbon monoxide and ozone. It changes the microenvironment of the alveoli, making the air passages more sensitive and causing severe respiratory stress in asthmatic people. Extreme dryness causes irritation and breathing problems. During the winter season, common respiratory viral infections like the flu and the common cold are prevalent, and they further serve as asthma triggers and 75% of asthmatic people experience more severe asthma symptoms during the flu and cold. Likewise, the risk of bacterial and viral chest infections multiply in winter, triggering asthma with even worse symptoms.
During winter, there is a rapid surge in other respiratory allergens like dust mites and mould spores. The dust mites seek shelter in the bedding material from the extreme cold outside, and the damp conditions in the winter cause increased fungal growth indoors. The combination of all these factors causes the severity of symptoms of seasonal asthma, and the change is reflected in the increased number of hospitalizations due to asthma, particularly in paediatrics and elderly patients. The study by Yoming Guo and his colleagues in 2012 noted that severe cold temperatures in the winter months cause a significant increase in the number of outpatient hospital visits in the paediatrics. They recommended that asthmatic children need better protection from winter than others. A cold spell of as low as 20 days causes severe symptoms in asthmatic people.
Mould or Mildew
Fungus grows everywhere. Some, like mushrooms and yeasts, are safe and are a food source, while mildew (the dark stains on expired foods, ceilings and bathroom walls) and many other species of fungus produce toxins and allergens. The moulds are microscopic fungus that is airborne, and their ingestion cause respiratory problems. The mould produces spores which are very tiny and invisible reproductive structures but are very effective allergens.
The mould and mould spores in the air stick to the pets' bags, shoes, clothing and fur, increasing the risk of inhalation. Asthmatic people allergic to mould and mould spores experience reduced lung functions, increased hospitalizations and high mortality rates due to severe asthma symptoms. The inflammation of the airways causes them to become narrow and swollen. The increased mucus production causes the symptoms like coughing, wheezing, breath shortness and chest tightness.
Hypersensitivity pneumonitis (HP) is a lung inflammation that develops when people develop severe sensitization and allergic reactions to organic dust, including mould and mould spores, and causes symptoms similar to allergic reactions. The other symptoms of HP are fever, chills, night sweats and extreme fatigue. The symptoms appear after 2-9 hours of exposure and last 1-3 days.
Workers working in damp or dusty conditions, particularly those dealing with the organic stuff, experience a disease known as mushroom picker’s disease. The workers working in the buildings have plumbing leaks, roofing leaks, high indoor humidity, and poor ventilation, develop it and have an increased risk of seasonal asthma in the sensitized people.
The research has found a relationship between asthma onset and symptoms and dampness in the buildings. Individuals with dust allergies, allergic asthma, or other allergic conditions of the respiratory system need to eliminate or at least reduce exposure to the risk factors of mould development in indoor settings and reduce exposure in the outdoor environment.
What are the Symptoms of a Seasonal Asthma?
The symptoms are predominantly respiratory. However, some general signs of infections do occur. The asthma symptoms in adults have some differences from those in children. Some common symptoms of seasonal asthma are;
- Fatigue: Fatigue is a feeling of tiredness and exhaustion, and asthmatic people experience signs of fatigue like low energy and sleepiness during working hours. Various causative factors are night-time coughing leading to poor sleep, overnight hospitalizations and severely compromised respiratory functions leading to insufficient oxygen supply to the tissues.
- Coughing: Coughing is an involuntary action resulting in the forceful expulsion of air from the upper respiratory tract with a loud noise. Some patients experience a cough variant asthma (CVA), whose sole symptom is a chronic cough. The hyperresponsiveness and inflammation of the airways trigger the coughing response during asthma flare-ups.
- Shortness of breath: Shortness means shallow and rapid breathing and is a sign of severe respiratory stress. It is experienced in asthma, but additional asthma symptoms need to be present. Otherwise, it is a sign of infections of the respiratory system.
- Wheezing: Wheezes are the adventitious, musical and high-pitched sounds produced in the airways due to their narrowing, inflammation, and allergic reactions. Seasonal asthma results from the oscillations of the walls of airways, which are caused by the flow of air through them. They are a sign of severe respiratory stress and must be treated immediately.
- Chest tightness: Chest tightness is reported by the patients as a feeling of having a heavy weight on the chest, which makes deep breathing difficult and painful. The inhaled triggers like pollens, pet dander, dust mites, cold air and smoke pollutants cause allergic reactions resulting in chest tightness. In the absence of other respiratory signs and allergic reactions, it is a sign of heart issues and needs immediate attention.
- Rapid breathing: Rapid breathing occurs as the body responds to severely compromised respiratory functions and poor oxygen supply to the tissues by increasing the respiration rate. Medically known as tachypnea, it is a sign of asthma and other issues like chronic obstructive pulmonary disease (COPD), pleural effusion, pulmonary embolism, carbon dioxide poisoning, diabetic ketoacidosis and sepsis.
Fatigue
Fatigue is the inability to perform regular activities or respond to external stimuli. It is the feeling of exhaustion or tiredness due to excessive physical exertion or chronic disease. It is attributed to various asthma-related causes like disturbance of nighttime sleep due to nocturnal cough, lack of or poor appetite, the reduced blood supply to the body due to poor respiratory functions, a chronic cough that causes the spasm of local muscles and a low rate of energy metabolism.
It is reported by as much as 90% of people with uncontrolled or severe asthma, and studies have noted that children with asthma experience tiredness and exhaustion that disturbs their learning and development. The control and management of asthma symptoms are necessary to eliminate asthma-linked fatigue.
The patient needs to work with the doctor to formulate a treatment and prevention plan that includes avoiding triggers like pet dander, dust, pollens and other allergens, using medications to control and treat inflammation of airways, treatment of underlying conditions that cause asthma flare-ups like anxiety, depression, gastroesophageal reflux disease, obesity etc., and the use of quick-relief medications like inhalers and bronchodilators.
Primarily, the fatigue causes by seasonal asthma last only as long as the symptoms of the disease last. It is essential to consult the healthcare provider to formulate an effective treatment and prevention plan for easy and fast recovery.
Coughing
Coughing is the forceful expulsion of air from the lungs and airways with a short yet sharp noise. It is a deliberate attempt by the body to eliminate allergens and other triggers of seasonal asthma. Coughing and asthma are closely related, and as many as 30-40% of people with chronic and untreated coughs ultimately progress to asthma. Both asthma and chronic cough have many features in common, like remodelling and hyperresponsiveness of air passages ways, atopy (genetic tendency to develop asthma) and airway inflammation. The presence of cough in patients with asthma is a sign of severe complications and poor prognosis. Cough due to asthma is classified into three types: CVA (cough variant asthma), resistant cough, and predominant asthma. Among them, CVA has a cough as the only significant sign. The asthmatic cough is minimally productive to dry and involves increased mucus production. Excessive mucus production causes a rapid decline in respiratory functions and death in more severe cases.
Managing asthmatic cough requires a sound strategy to control the symptoms and reduce exposure to the triggers. The asthma action plan must be prepared after consulting the doctor and followed strictly. The other helpful measures are taking the prescribed medications regularly, identifying and avoidance of triggers, maintaining good indoor air quality, maintaining indoor air humidity by using a humidifier, maintaining hydration, stress management, practising good hygiene and practising techniques like pursed lip breathing, deep breathing and diaphragmatic breathing etc.
The duration of the cough depends upon the type of asthma and the exposure to triggers. Sometimes, it is short-lived and last only for free days to weeks and sometimes, it becomes a chronic cough (with chronic asthma) and last for months. Persistent cough must be discussed with the doctor as it is often a sign of more severe conditions like tuberculosis.
Shortness of Breath
Shortness of breath or dyspnea is the feeling of intense tightness in the chest and is accompanied by air hunger and a sense of suffocation. It is a sign of serious respiratory issues.
It is among the primary signs of asthma. During asthma, the airways become blocked and inflamed, and the lungs become more prone to irritation and inflammation. The symptoms are apparent after some stressful events, like physical exercise; however, the symptoms sometimes occur without any triggers. The presence of other signs of seasonal asthma, e.g., chest tightness and nocturnal cough, causing disturbed sleeping and tiredness, confirm the cause.
Chest tightness is not limited to asthma and develops in some other conditions like obesity, lung diseases, anaemia, arrhythmia, coronary artery disease, heart valve disease etc. Healthcare providers rely on tests like chest X-rays, ECG, blood tests, CT scans and lung function testing to diagnose the cause.
The control and prevention need strictly following the asthma treatment plan, identification and avoidance of triggers, practising self-management techniques (e.g., breathing exercises), opting for a healthy lifestyle, using OTC medications like inhalers and bronchodilators and staying prepared for flare-ups by always carrying an inhaler to use in case of emergency are very useful. The duration of symptoms varies and ranges from a few minutes and hours to many days. It is a healthcare emergency and must be dealt with urgently.
Wheezing
Wheezes are the sounds produced as a person tries to breathe through the constricted and narrow airways. The constriction of airways causes the air velocity inside them to increase. It results in lower pressure inside (and higher outside), leading to more constricted airways. As the air rushes with high velocity from these barely open airways, the fluttering of walls of airways causes a continuous and musical sound.
During the immediate-type hypersensitivity response (allergic asthma), antibodies (IgE) are released. These antibodies bound to the antigens. The antigen-antibody complex is identified by the immune cells causing the release of biochemical mediators like histamine. These mediators cause contractions of the airway muscles and increase the mucus production and permeability of the blood vessels, leading to more recruitment of immune cells.
Wheezing is described differently by different patients. Some people experience loud noises with difficulty breathing (wheezy dyspnea), while others experience rattling secretions and whistling with breathing. In many cases, people with chronic asthma become accustomed and don't inform the physician unless asked. Wheezes are more common with exhaled air because airways are more constricted during expiration.
Strictly following the asthma treatment plan, use of inhalers, avoiding triggers, vaccinating for common respiratory infections and practising breathing exercises are helpful measures. The duration of wheezing varies and ranges from a few minutes and hours to days, depending upon the treatment and prevention.
Chest Tightness
Chest tightness is a feeling of burning, fullness and pressure in the chest due to various factors like digestive issues, lung diseases, cardiovascular issues, anxiety, injury and infections. It is a subjective sign, and other symptoms of allergic reactions must be present to associate it with the allergic reactions.
Many factors trigger chest tightness in seasonal asthma, e.g., mould, pollen, cold air, smoke, and pet dander. Many of these factors, like pollen and mould spores, are more common in harvesting and rainy seasons. During asthma, the bronchioles become constricted due to inflammation. The air passageways retain more air. Both factors make inhaling and exhaling air challenging, causing chest tightness.
Managing chest tightness caused by asthma needs the same protocols as with other signs, i.e., following the asthma treatment plan, avoiding triggers, using inhalers and bronchodilators, opting for a healthy lifestyle, proper vaccination for common diseases and practising general hygiene. The duration is highly variable and lasts as long as the causative factors are present. Some people experience improvement within hours, and the chest tightness lasting for days is a sign of severe health issues and must be consulted with a doctor.
Rapid Breathing
Rapid breathing or tachypnea is abnormally fast and shallow breathing. In adults, the average breathing rate is 12-20 breaths per minute and having more than 20 breaths in a minute reflects tachypnea. In children, the rate is relatively higher than the adults.
Various underlying causes like asthma and lung infections cause tachypnea. The symptoms worsen at night, after exercise or contact with cold air and allergens. It is, however, not unique to seasonal asthma. Several other issues like diabetic ketoacidosis, sepsis, carbon dioxide poisoning, COPD, pulmonary embolism, pleural effusion etc., cause it, and the patients need to consult the doctor to identify the cause. During asthma attacks, it occurs as the body tries to compensate for the decreased supply of oxygen or more load of carbon dioxide in the blood.
Several breathing techniques like diaphragmatic and pursed lip breathing, relaxing exercises, taking the prescribed medications regularly, and practising controlled breathing are helpful techniques to manage it. Tachypnea lasts a few minutes to hours, depending upon the treatment, level of immunity, prevention protocols, and exposure to allergens.
How is Seasonal Asthma Diagnosed?
The diagnosis of asthma follows the same approach as used for all illnesses. The physicians take hints from the history, clinical signs and physical examination and use laboratory tests to confirm the findings.
History of illness: During history taking, the doctors ask questions about the symptoms, duration and intensity of symptoms, knowledge about the different triggers, family history of the illness, the presence of other conditions and the current or past use of drugs and medications.
Physical examination: During the physical examination, the doctors monitor the upper airways, including the throat and nose and listen to the respiratory sounds using a stethoscope. The other signs of allergic reactions like eczema, hives and skin lesions show that the cause is an allergic reaction. Some other asthma symptoms, like chest tightness, breathing issues, coughing and wheezing, are essential to note.
Pulmonary testing: These tests help doctors judge the lungs' health and monitor the progression of disease and treatment. These tests are to be conducted and interpreted by qualified professionals. Some standard lung function tests are:
- Spirometry: It is a painless, simple and quick test. During spirometry, the patient is asked to take a deep breath and exhale into a hose connected to the spirometer. The spirometer measures the forced vital capacity (FVC) and forced expiratory volume (FEV). Low values indicate the constriction of air passages due to lung diseases, including asthma. Several tests at regular intervals are used to monitor the progression of illness and medication efficacy.
- Allergen challenge tests: In these tests, substances like methacholine and histamine are inhaled that trigger asthma symptoms. The physician measures the change in lung functions after the challenges.
- Exhaled nitric oxide test: During exhaled nitric oxide test test, the patient is asked to exhale into a tube connected to a machine that detects the nitric oxide levels in the exhaled air. Its higher levels indicate that there is inflammation in the airways.
- Peak flow meter test: It measures the ability of the lungs to expel the air. It is conducted using the peak flow meter, a plastic tube with a mouthpiece at the end. Its working is similar to spirometry but is less accurate.
Other tests: Some other tests helpful for the physician are:
- X-rays: It helps diagnose infections, tumours or other lung issues. During these tests, the patient is asked to hold the breadth in front of the X-ray machine, and the X-rays generate a picture of the lungs. The picture helps the physician in diagnosis.
- Diffusion tests: These tests help measure the blood's ability to absorb the gases from the inhaled air, like oxygen. A measured amount of gas is inhaled while the patient's blood is analyzed for the levels of drugs absorbed.
- Blood tests: Blood tests help measure the immune response to allergens and infections. These tests monitor the levels of immunoglobulins (IgE) and eosinophils, the key players of inflammation and allergy. High levels are indicative of allergic reactions like asthma.
- Sputum eosinophil testing: It detects the presence of eosinophils in the mucus and saliva that are expelled during coughing. The eosinophils take stains with rose-coloured dye and are a sign of asthma.
Based on these tests, the doctors classify asthma into mild intermittent, mild persistent, moderate persistent and severe persistent. The doctors are often interested in testing other conditions causing the symptoms, like allergies, sinusitis, hay fever, heartburn, and gastroesophageal reflux disease (GERD).
Can Seasonal Asthma be diagnosed through symptoms alone?
Yes, the symptoms provide helpful insight into the disease. However, the diagnosis solely based on the clinical signs is less satisfactory, and physicians need to perform more precise clinical tests. The clinical signs are nevertheless helpful in making a presumptive diagnosis and differentiating the situation from related conditions. The symptoms are very likely misinterpreted or not correctly reported by the doctor. Asthma is a chronic illness; patients often become so habitual that they miss the signs entirely. The clinical signs thus provide an initial insight into the causes of the symptoms.
What tests do Doctors perform to diagnose Seasonal Asthma?
Several tests are used by healthcare professionals, i.e., allergists and pulmonologists, to diagnose seasonal asthma. These tests measure the obstruction or inflammation in the airways and reduced lung capacity and are to be performed and interpreted by healthcare professionals. Some standard tests are;
Spirometry: It measures the amount of air inhaled and exhaled and provides a quick view of pulmonary health. The spirometer measures the forced vital capacity (FVC) and forced expiratory volume (FEV). The reference values depend on age, gender, height and race.
The doctors determine the predicted average values of FVC for a person, and the predicted value is compared to the calculated value. The test is normal if the actual value is 80% or more of the predicted value. Values less than 35% indicate severe abnormalities (American Thoracic Society).
Peak flow monitoring: It judges lung health by measuring the amount of air exhaled. It measures the average peak expiratory flow rate (PEFR). The normal PEFR in adult men and women are 450-550 L/ min and 320-470 L/ minute, respectively. The values that are 80% or more of these reference values are considered normal, and the lower values are warning signs.
Immunoglobulin testing: These tests detect the presence of allergen-specific antibodies (particularly IgE) in the blood and help to identify seasonal allergens. The IgE levels in asthma are many times that observed in healthy people. For example, the average values of 151.95 IU/ml were observed in healthy individuals compared to the 1045.32 IU/ml in people with severe asthma in a model developed by the Indian Chest Society in 2010.
Allergy skin test (skin prick test): These tests detect the reaction to a particular antigen after introducing that allergen into the skin. A measured amount of an allergen is placed on the skin. The skin is scratched to allow the entry of allergens into the skin. The subsequent reaction helps the doctors assess the results. These tests are highly sensitive (more than 90% sensitivity).
CT scan and radiography: It is a practical approach to rule out conditions like tuberculosis, lung cancer, etc., that are easily detectable in the lungs.
Nitric oxide test: The levels of nitric oxide in the exhaled air increase in asthma. The NO test (fractional exhaled nitric oxide-FeNO) detects and measures the NO in exhaled air. The values less than 25 parts per billion (ppb) are considered normal, 25-50 ppb as intermediate and more than 50 ppb as higher.
Challenge tests: In these tests, increasing amounts of some allergic substances like methacholine are inhaled, and the responses are measured.
It is important to note that these tests have pros and cons, and many times, a combination of tests and findings of physical examination are used to diagnose asthma.
How accurate are the tests used to diagnose Seasonal Asthma?
The accuracy of tests used for seasonal asthma is variable and depends upon different individual factors.
Spirometry: It is a reliable test; if properly conducted, it detects asthma by a reasonable margin. Under normal conditions, it provides an accuracy of 60% in asthmatic conditions. The accuracy is higher under better conditions (Matthew and colleagues, 2016).
Peak flow monitoring: Its accuracy depends upon the frequency of use, the technique used, and the expertise of the pathologist or laboratory technician. It is less accurate than spirometry but still produces valuable information. Most of the portable peak flow meters are accurate up to 400 L/ min, and the accuracy decreases afterwards.
Exhaled nitric oxide test: It is an accurate and reliable test. However, its usefulness depends upon many factors like respiratory diseases, smoking status, age, health status and the quality of apparatus used. The standardization of all these variables provides more better specificity.
Methacholine challenge test: It is a particular test to detect the hyperresponsiveness of the airways, a common feature of asthma. Its sensitivity for intermittent and mild asthma varies. The test yielded a sensitivity of 39% and specificity of 77% in a study published in the Biochemical Pharmacology in 2020.
Immunoglobulin detection tests: These tests are highly accurate and sensitive in detecting immunoglobulins against allergens. However, the specificity is highly variable (30-95%) as immunoglobulins are produced during conditions like infections and parasitic infestations. These tests' findings need to correspond with the clinical signs and symptoms.
CT scan and radiography: These are useful but not specific to seasonal asthma and are used for differential diagnosis and to rule out other lung diseases. They help monitor the structural changes in the lungs.
How often should I be tested for Seasonal Asthma?
The testing frequency is variable and depends upon factors like disease severity, the frequency of attacks and doctors' recommendations. The standard suggestions are.
Spirometry: It is done annually for monitoring purposes and as recommended during an asthma attack to monitor disease progression and treatment efficacy.
Peak flow monitoring: It is easy to perform and is often conducted at home. It is used to monitor the changes in the health of the lungs and judge the treatment efficacy. Depending upon the need, it is performed daily or weekly.
Challenge tests: The challenge tests like the methacholine challenge test are done only when needed and routine testing is not required.
Exhaled nitric oxide test (FeNO test): It is used to monitor the health of airways and is often used at regular intervals to monitor the signs and predict suspected asthma attacks. Depending upon disease severity, treatment plan and individual health, it is recommended after every 3-6 months or more closely if needed.
Allergy testing: It is done to identify the potential allergens at the initial phase, and repeat testing is not necessary. A symptom change often requires repeat allergy testing to see any new allergen.
These frequencies are given as guidelines, and the pulmonologist or the allergist has the final say in deciding when to test.
What are Treatments for Seasonal Asthma?
The treatment of seasonal asthma needs a comprehensive asthma treatment and prevention plan. It needs to be developed after consultation with the doctor and include all important factors. The plan must include:
- Limiting exposure to triggers.
- The OTC and prescription drugs.
- Quick relief medications.
Some standard treatment options are;
- Inhaled Corticosteroids: These drugs suppress the airway's inflammation, and regular use controls the symptoms and often prevents flare-ups. These drugs are inhaled using a portable device.
- Bronchodilators: Bronchodilators work quickly and are often the first line of action in case of an asthma attack. They dilate and open up the airways in the lungs. They are known as rescue medications and include pirbuterol, levalbuterol and Albuterol.
- Leukotriene Modifiers: These drugs block the effects of a chemical, the cysteinyl leukotrienes (CysLTs), in the airways. The CysLTs cause inflammation and constriction in the airways. Typical examples are Zileuton and Montelukast.
- Combination Inhaler: The combination inhalers contain a combination of long-acting corticosteroids and beta-agonists. Both of these drugs work together to open the airways and reduce swelling.
Inhaled Corticosteroids
The inhalation corticosteroids work like natural cortisone and help prevent and treat asthma symptoms. Their regular use treats the severity and frequency of asthma attacks. However, they don't relieve an already ongoing asthma attack. The common examples include Fluticasone, Budesonide, mometasone, Beclomethasone and Ciclesonide.
The corticosteroids prevent the release of inflammatory chemicals from the cells in the nasal passages and lungs. These include histamine, cytokines and interleukins. The inhalation corticosteroids are used alone or combined with oral corticosteroids and bronchodilators. Different dosage forms are suspension, aerosol powder, powder and aerosol liquid.
They are very effective for asthma symptoms irrespective of the disease severity and age of the symptoms. They improve lung functions, cost-effective, convenient to use, control symptoms, prevent exacerbations, reduce irreversible changes in the air passages due to asthma, and lower the number of deaths.
The adverse effects of inhaled corticosteroids include metabolic disturbances, behavioural abnormalities, decreased growth in children, increased risk of cataracts, skin thinning, bone loss and adrenal suppression. Some other signs are chest pain, pain and burning during urination, unusual weakness and tiredness. Some rare side effects are vomiting, numbness, nausea, loss of appetite, skin pigmentation, hypertension, polyuria, increased thirst, fever, fainting, blurred vision, bloody stools, dizziness, fast and irregular heartbeat,
So, although inhalation corticosteroids are heavily prescribed for treating asthma symptoms, they must be used at the lowest necessary dosages to avoid their side effects.
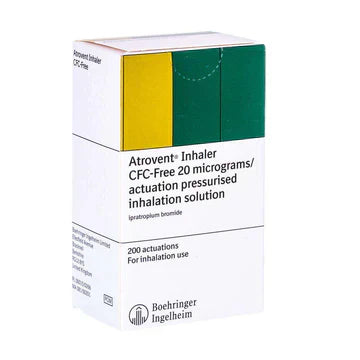
Bronchodilators
Bronchodilators help in asthma by relaxing the muscles around the airways and clearing mucus from the lungs. They are available in long- and short-acting forms and are taken as tablets, nebulizer solutions or inhalers. The short-acting bronchodilators are effective for 3-6 hours and provide quick relief from the symptoms of an acute attack (rescue inhalers). The long-acting bronchodilators are effective for up to 12 hours and are used daily to prevent asthma attacks. Different types of bronchodilators available are;
Beta 2 agonists: These are available in long-acting or short-acting versions. The short-acting versions start working within 15-20 minutes and are effective for 4-6 hours. These include Albuterol (Ventolin®), Levalbuterol (Xopenex®) and a combination of Ipratropium bromide and Albuterol (DuoNeb®). The long-acting versions are effective for 12 hours and are taken twice a day. They include Formoterol (Foradil®), Salmeterol (Serevent®) and combination medications like Advair® (Salmeterol+ Fluticasone) and Symbicort® (Formoterol and Budesonide).
Theophylline: It is available as oral pills, which are taken daily to control symptoms. The familiar brand is Uniphyl®. However, there are other better choices nowadays.
Anticholinergics: These include Tiotropium bromide (Respimate®) and Ipratropium bromide (Atrovent®) and are available as a nebulizer solution or inhaler. These drugs work by blocking the effects of the neurotransmitter acetylcholine. Anticholinergics are effective but are not helpful as quick-relief medications.
Each class of bronchodilators have different side effects. The side effects of beta 2 agonists are troubled sleeping, stomach upsets, increased heart rate, hyperactivity, over-excitement, shaky feelings and nervousness; the side effects of theophylline are nervousness, unstable feelings, muscular cramps, irregular and fast heartbeat, diarrhoea, headache, stomach ache, vomiting and nausea and the side effects of anticholinergics are temporary blurriness of vision, vomiting, nausea, unusual taste and dry eyes, throat and nose. The bronchodilators must always be used according to the doctor's recommendation to avoid side effects.
Leukotriene modifiers
Leukotriene modifiers, sometimes called leukotriene receptor antagonists, treat asthma and allergic reactions. These drugs block the effects of leukotrienes, the inflammatory compounds produced in the body during allergic reactions. These compounds tighten the airway muscles and increase mucus production. The blocking of the effects of leukotrienes prevents the constriction of airways.
The leukotriene modifiers influence the early and delayed types of responses to allergic reactions. They are combined with other drugs in case of an asthma attack and are not used alone. Different leukotriene modifiers available are Montelukast (Singulair®), Zafirlukast (Accolate®) and Zileuton (Zyflo®). Montelukast is recommended for allergic rhinitis and asthma. They are available as tablets, granules and chewable tablets.
The leukotriene modifiers must be used as the doctor for 3-14 days or as the doctor. Proper use ensures smooth breathing, allows an asthmatic person to exercise, keeps the airways open and reduces the frequency, severity and symptoms of asthma attacks.
Liver damage is a common side effect, and people with liver diseases must avoid them unless the doctor asks. They are generally safe. However, some side effects are cough, runny nose, sore throat, fatigue, diarrhoea, ear infection, fever, headache, heartburn, rashes, itchy skin, lack of appetite, nausea and stomach pain. Sometimes emotional side effects like depression, insomnia, anxiety, headaches and abnormal behaviour occur mainly in younger people. Serious side effects are rare. However, some signs of allergic reactions, heart palpitations, tingling or numbness in the feet or hands, vomiting, troubled breathing etc., must be reported to the doctor.
Combination inhaler
A combination inhaler combines two different types of medications inside a single device. The most common combination is a long-acting bronchodilator and a corticosteroid. The bronchodilator relieves asthma symptoms, like chest tightness and breathlessness, and the corticosteroid treats inflammation. They are available as dry powder or aerosol inhalers. Examples include Symbicort®, Fostair® and Seretide®.
The combination inhalers must be taken daily, even without symptoms. Combination inhalers are mostly not helpful in case of asthma attacks and worsening symptoms, and fast-acting inhalers are required in these conditions. Combined inhalers provide relief within a few days, which is shown by the decreased need to use the rescue inhalers, less frequency of breathing issues and wheezing, less nocturnal coughing and better sleep. A few days of regular use are enough to see the benefits. The full benefits of everyday use become apparent after some weeks as the corticosteroids thoroughly treat the inflammation in the airways.
The risk of side effects is relatively lower in the case of proper use. Some people experience issues like oral thrush, mouth infections, hoarse voice and sore tongue. These or any other side effects must be reported to the doctor immediately. The other side effects are upper respiratory tract infections, vomiting, nausea, coughing, dizziness, nausea, headache, sneezing and stuffy or runny nose. Rarely do some people experience paradoxical bronchospasms, particularly those with severe airway inflammation and use an inhaler for the first time. Rarely do signs of allergic reactions develop.
Can Immunotherapy be used to Treat Seasonal Asthma?
Yes, immunotherapy (allergy shots) is an effective way to treat allergic asthma, which often takes a seasonal outlook. During the immunotherapy, the measured doses of the specific allergen are administered to the sensitive person to desensitise the patient. Two modes of immunotherapy used are sublingual immunotherapy (SLIT) and subcutaneous immunotherapy (SCIT). In allergic asthma, the immunotherapy using the house dust mite allergens causes a decrease in the clinical signs, medication dose and hyperresponsiveness of airways. It helps in the natural course of the disease, and its effects continue for a few years, even after the end of the treatment. It suppresses responsiveness to new allergens and lowers remission rates in children. Immunotherapy helps control the other triggers of asthma, like allergic rhinitis.
What are ways to prevent Seasonal Asthma?
The ultimate success of that asthma control strategy is to avoid exposure to the seasonal allergens. As no specific cures are available or are very expensive if available, the following points are helpful to prevent seasonal asthma.
Identify and avoid triggers: The common triggers of seasonal asthma, like pests, e.g., cockroaches, dust mites, pet dander, fragrances, smoke, sinusitis, exercise, cold air, allergens and air pollution, must be addressed. A helpful option is to maintain an asthma diary which details the exposure to emotional and environmental risk factors. The patients must check the diary to see the suspected allergens as soon as the symptoms appear. Some allergens are not obvious, and tests help sort them out.
Healthy physical activities: Healthy exercises and physical procedures benefit lung health, and studies have noted that people spending 30 minutes daily on physical exercises have 2.5 times more control over the symptoms. Yoga, biking, swimming and hiking are beneficial activities. The training is helpful for asthmatic children too.
Avoid allergic foods and medications: The drinks and foods are not among the common asthma triggers. However, some foods like shrimp, dried fruits, potatoes, wine, and bear sometimes worsen symptoms. Some medications like hypertensive drugs and painkillers exacerbate the symptoms and must be consulted with the doctor.
Avoid smoking: Smoking is hardly a good idea for asthmatic people. Limiting exposure to various sources of smoke, like cigarettes, fireworks, candles, fires and incense, must be avoided. If the asthmatic person has the habit of smoking, it must be eliminated or reduced.
Avoid exposure to the cold: The seasonal cold and flu worsen asthma symptoms, and patients need to avoid symptomatic people, particularly in the high-risk season. Regular hand washing must be done to reduce exposure to germs from contaminated surfaces.
Strictly follow the asthma action plan: Regularly taking prescription medications and emergency inhalers are good practices. However, the patients must carry a copy of the asthma action plan with them for more specific instructions in case of unexpected attacks.
Keep a peak flow meter at home: The peak flow meter helps judge how effectively air flows through the lungs. The meters are helpful to see changes in the air circulation hours before the appearance of clinical signs. It is enough time to recall the action in the treatment plan and take appropriate measures to control and prevent the attack.
Take prescribed medications regularly: The long-term treatments are designed to prevent asthma attacks. These medications must be used even in the absence of any clinical signs. However, if side effects are experienced, the patients must consult the doctor for treatment changes.
Consult the doctor for immunotherapy: The allergy shots help prevent seasonal asthma symptoms and more severe issues. It makes a person desensitised to the common allergens and helps reduce severe flare-ups.
Regular vaccination for common infections: The yearly flu shots effectively protect against common flu viruses. The flu worsens seasonal asthma symptoms and increase the risk of complications like pneumonia, which needs hospitalisation. Consult the doctor for an effective vaccination plan against shingles, whooping cough, diphtheria, tetanus etc.
Maintain an allergy-proof environment inside the home: Maintaining an allergen-proof environment at home and the workplace reduces the risk of seasonal asthma attacks. Some effective strategies are regularly washing the pillow and other bedding materials in hot water (at least 130F) to kill the mites, maintaining inside humidity levels between 30-50%, using a moist vacuum to remove dust from the floor, controlling pests in the indoor settings reserving a smoke-free hotel room during outings and staying away from the social gatherings where exposure to the allergens is expected.
Effective pest control: Pests like cockroaches are a source of allergens. So an effective control program including the removal of their hiding places, depriving them of food and water, using closed containers for trash, regularly washing and cleaning the areas that attract pests, sealing the openings and cracks in the plumbing, walls, etc., must be Closed, pesticide traps and baits must be installed.
Does education help prevent Seasonal Asthma?
Educating the patients and general population about asthma control and management aspects is very important. Education aims to allow the patients to recognize the signs and initiate the predetermined plan earlier. The studies have found that including the patient in the informed decision-making process significantly improves disease management. It allows a person to make timely decisions to avoid more dangerous symptoms.
It enhances the communication and trust between the physician and the patient. The guidelines about asthma education plans are developed by the healthcare agencies like the National Heart, Blood and Lungs Institute (NHBLI). The asthma patients participating in the plan are taught about different aspects of asthma-like what asthma is, what the different types of medications used for asthma, how these medications work, when are these medications used, what are their side effects, what are other asthma triggers, and how are they controlled, how to use instruments like the peak flow monitor and respond to changes in the values of the peak flow meter.
A regular program consists of 2 separate sessions of 1 hour each. The patient is interviewed individually during the first session, and individual-specific issues are highlighted. The education is focused on these individual issues. The patient is trained to use peak flow monitors and interpret the values. After 2 weeks, the patients return for another session, and the results of their self-monitoring are analyzed. The patient is trained on more issues that arise, and the information covered in the previous session is again reviewed. The patient education reduces the risk of emergency hospitalizations by allowing the patient to make informed decisions earlier.
Should I avoid particular seasons or weather to avoid Seasonal Asthma symptoms?
Yes, a person with seasonal asthma must be aware of different seasonal triggers to avoid severe symptoms. The everyday things to keep in mind are;
Seasonal variations in pollens: Pollen counts have seasonal variations. When the flowers bloom, the pollen load is higher in spring and early summer. If symptoms appear in spring and early summer season, it is essential to avoid exposure.
Avoiding cold air: The cold weather and air are essential asthma triggers. They cause narrowing of airways and increased mucus production, causing severe symptoms. If symptoms increase in severity in the cold weather, the patients must take steps to avoid exposure to the cold air.
Avoid indoor allergens: Indoor allergens like dust mites, pet dander, mould spores, etc., often show seasonal variations. The dust mites and mould spores increase in hot and humid weather. Likewise, different insects increase in number in different seasons, corresponding to their breeding seasons. Suppose a patient is susceptible to a particular allergen during a specific season. In that case, it is essential to avoid exposure by rigorous indoor cleaning; controlling the indoor humidity, installing HEPA filters, and taking the help of a doctor to manage severe symptoms are helpful options.
Thunderstorms: Some people experience more severe symptoms during thunderstorms. A thunder causes the tiny pollens to burst into small pieces and create fine dust that is more easily inhaled.
So, different asthma triggers have seasonal variations, and it is essential to identify these triggers and address them appropriately.








 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews