Covid Test Lines: Results Explained
Related products
As the Covid-19 virus engulfs the globe, understanding this novel pathogen becomes paramount. Originating in Wuhan, China in 2019, it has rapidly spread causing severe illness worldwide.
Testing is indispensable to control its spread through early detection and appropriate responses. Commonly used tests are Polymerase Chain Reaction (PCR), Antigen test; and Antibody tests mainly for research work due to their lower sensitivity compared to other methods.
PCR identifies genetic material specific to coronavirus but requires specialized labs and time which poses logistical issues. Conversely, antigen testing detects viral proteins quickly. However, with less accuracy than PCR antibody testing looks at past exposure by detecting antibodies that develop two weeks post-infection not always detectable in symptomatic individuals.
Dr. Margaret Harris of WHO emphasizes diagnosing active cases combined with effective isolation practice for controlling outbreaks more effectively.
According to CSIS, the the majority of diagnostics consist of PCR Antigen methods US India UK using a mixture of all three types as per requirement further conveying about limited accessibility problems faced in some regions due to high costs associated with logistics maintaining quality control.
What Are The Types Of COVID Tests?
PCR Tests

The Polymerase Chain Reaction (PCR) test, trusted for its high degree of accuracy, is utilized extensively worldwide. It operates by determining the presence or absence of specific genetic material belonging to SARS-CoV2 within a collected sample - generally via nose-throat swabs.
Interpreting PCR results involves understanding three potential outcomes – positive, negative, or inconclusive. A 'positive' outcome implicates an active infection; people with such results need immediate isolation and contact tracing measures taken right away. On the contrary, a 'negative' result means that there were no signs of viral genetic materials in one's body at the time testing was conducted—it doesn't exclude the chance of having contracted the virus after said date effectiveness depends on timing sample collection relation patient’s exposure disease last but not least ‘inconclusive’ indicates technique anomalies thereby requiring retesting ensure definitive diagnosis.
Antigen Tests

Contrary to PCR tests which detect pathogen's genetic matter antigen tests focus on identifying proteins expressed by viruses mainly nucleocapsid phosphoprotein found outer layer rapid nature coupled with ease of use makes them suitable choices for large-scale screening. Despite lower sensitivity compared to the gold standard, these assist early detection, particularly symptomatic individuals help mitigate further transmission through speedy initiation of precautionary actions and appropriate treatment regimes if needed.
Regarding interpretation, the Antigen Test comprises two possible conclusions - Positive Negative while the third option "invalid" sometimes arises due to technical issues conducting procedure same as above signifies current infestation whereas signifies lack thereof during moment assessment again does guarantee future immunity from contagion. Lastly eventuality such needs rerun connexion ensuring accurate verdict stringent quality control checks.
Antibody Testing

An Antibody Test albeit a less popular predominantly applied research serology survey purpose lies in examining an individual’s immune response to past infections rather than diagnosing present one approach attention drawn towards antibodies developed post-infection namely IgM &IgG production reaction detected blood samples comprising convalescent plasma serum thus imparting valuable insights regarding community exposure immunity levels as part broader public health strategies.
Discovery of different antibodies in IgG &IgM one’s system offers four possibilities - presence or absence of these proteins signifies past COVID-19 infestation probability having developed some level of enduring resilience Once detected signals recent battle novel coronavirus Whereas occurrence connotes earlier engagement virus indicating potential long-term resistance Lastly denotes lack previous encounter SARS-CoV2 hence no established defense. Unfortunately, results aren't definitive indicators of protective immunity since the actual correlation between antibody titers' safety from reinfection is yet to be fully understood and comprehensively researched.
You can find multiple available COVID tests including COVID-19 Antibody Blood Test, PCR Fit to Fly COVID Test for Travel, and Lateral Flow Antigen Tests that you can carry out in the comfort of your home from Welzo’s E-pharmacy here.
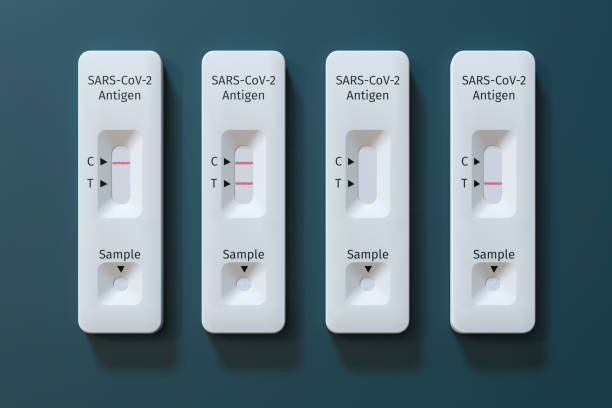
Understanding the Lines on Rapid Antigen Tests
Test Line (T)

The 'Test line' or 'T', when visible, forms an integral part of interpreting a rapid antigen test result. The appearance of this line signifies the presence of COVID-19-specific antigens in one's body, hence translating into a positive outcome. Arguably it indicates ongoing infection thereby necessitating the initiation of immediate isolation procedures followed by requisite medical care.
Conversely absence T-line construes a negative conclusion essentially implying non-detection of viral proteins at time assessment Though the scenario often means the person does not have a current infestation is important to note that timing testing about onset symptoms potential exposure has a paramount impactful role in dictating accuracy results Hence while the principle no T-Line equates lack illness must be borne mind nuances sensitivity these tests alongside individual circumstances.
Control Line (C)

In contrast control line "C" is quintessential ensuring the validity assay irrespective of the final interpretation Its main functions are to demonstrate the correct flow sample along the membrane and confirm the overall functionality of reaction components Pathologists and laboratory personnel rely heavily on intention maintaining gold standard diagnostic measures accurate dependable deductions.
Lack of C-line emergence despite proper conduct procedure alarms about invalidity Irrespective of other observed outcomes case requires immediate retesting due to possible technical failure rendering insufficient reliability lack thereof translates inability to validate integrity consequently deeming conclusions drawn unreliable Thus vital only consider outcomes valid face clear presence regardless underlying condition patient. You can get a detailed article on what c means on a COVID test at Welzo.
What Factors Affect The Test Results?

Timing of the Tests
One influencing variable in COVID-19 testing outcomes involves timing tests. Detecting an ongoing infection requires optimal time duration since exposure or onset symptoms for reliable results. PCR tests work best a few days post-exposure while Antigen tests give more accurate outputs when an individual starts showing signs of illness.
Able to identify the virus even before symptom manifestation, some people might not have accrued enough viral load in their system at point testing thereby leading to negative results despite actual presence Conversely, late detection runs the risk of incomplete viral shedding resulting in falsely indicating non-infection So precision lies understanding ideal window opportunity increases chances correct decipherment.
Sample Collection
Another critical factor is method sample collection where proficiency technique significantly impacts accuracy results. Nasal swabs are a common way of collecting samples yet it’s pivotal to ensure sufficient material is collected from the right area inside the nose to aid true representation of body status during that moment.
An improper collection holds potential skew outcomes either by obtaining inadequate quantity quality may lead to false negatives owing to unavailability of necessary components needed confirmation Additionally contamination of any sort jeopardizes authenticity hence necessitating utmost care hygiene standards maintain proper validity procedure execution decrements errors maintaining standard norms guidelines.
Test Kit Storage and Handling
The last crucial element considers dealing with test kit storage handling which demands meticulous attention following manufacturer instructions correctly Any deviation from set protocol compromises integrity and therefore its applicability. Depending on the specific type each one has unique requirements temperature and humidity factors affect performance upholding those essential for achieving consistent high-quality data.
Improper transportation and inappropriate environmental conditions alter sensitivity specificity kits thereby disrupting normal functioning and yielding inconclusive often misleading information Consequently abiding by recommended practices safeguards product potency optimally avoiding preventable discrepancies due to mishandling negligence. Therefore adhering to provided guidelines par imperative appropriate use of diagnostic tools ensuring credibility achieved conclusions.
What Causes False Positive and False Negative Results?

Causes of False Positives
False positives, though less common in COVID-19 testing, lead to significant implications on individual as well as community levels. One origin is cross-reactivity with other viruses or antigens present within one's body. In such situations tested kits react non-specifically against substances not related to SARS-CoV2 resulting in false alarms overshadowing the actual state health at hand.
In addition, user error emerges as another cause of inaccurate results Misinterpretations instructions inappropriate handling of samples wrong timing all contribute towards inflated positive outcomes Hence essence lies in ensuring high standard technique comprehension coupled with correct implementation methods primary step mitigating these inconsistencies while enhancing credibility interpretations.
Causes of False Negatives
Contrarily false negatives present a larger problem leading to underestimation extent of viral spread and the absence of detection of active infections Main factors contributing include conducting tests either too early or late post-exposure circumstances PCR tests need a few days incubation period to accurately detect pathogens whereas antigen heavily relies on symptomatic phase for optimum output hence incorrect sequencing spirals down into missed diagnosis.
Further poor sample quality due to improper collection storage transport inflates chances of skewed negative outcomes Any discrepancies in practice standards likely affect adequacy thereby dwindling fidelity assays Ultimately emphasis must be laid on intricate but impactful aspects like maintaining top-notch logistics systems alongside personal vigilance and efficient utilization of resources attain most authentic representational data.
What Do You Need to Do After COVID Test?
Positive Result
Following receipt of a positive result from a COVID-19 test, an immediate course of action necessitates self-isolation to limit the potential virus spread to individuals around. Thereafter primary step involves contacting healthcare providers to inform them about their current condition and seek further advice regarding necessary intervention management strategies.
In addition, confirmatory testing using PCR proves prudent to validate initial findings particularly if done through antigen or antibody tests Consolidating outcomes enhances diagnostic accuracy ensuring appropriate therapeutic measures and prevention procedures are implemented without delay hence optimizing patient recovery while reducing disease transmission simultaneously.
Negative Result
On the other hand, witnessing a negative outcome implies the absence of active infection at the moment of assessment Notwithstanding such interpretation ongoing precautions must continue carried out diligently to avoid contracting the virus future. These include regular hand washing wearing face masks maintaining social distancing etiquette among others.
Interestingly onset of symptomatic manifestations despite earlier negative findings calls for retesting Such a scenario indicates that it was likely too early to detect SARS-CoV2 during the first round of evaluation. Another possibility is contamination issues affecting reliability results Hence the emergence of any indicative signs post-test warrants another round of examination to ascertain the real-time status of one's health.
Invalid Result
Lastly encountering invalid output signifies technical malfunction or product failure situations like mandates prompt retesting with a new kit irrespective of symptomatology. Even seemingly insignificant variations in control line appearance might render the procedure invalid thereby necessitating repeat assay to obtain definitive answer.
Persistently recurrent inconclusive results then require professional consultation to interpret available data and provide experienced insight into decision making It ensures the right decisions are taken based on consistent evidence and negates instances of misinterpretation leading to incorrect conclusions Thus seeking expert opinion becomes vital whenever uncertainties arise interpreting home-based rapid test kits.
Takeaway
COVID-19 testing understands the virus with tests like PCR, antigen, and antibody being vital. Post-test actions vary: positive results demand isolation, medical advice plus potentially confirmatory PCR; negatives require persistent caution and retesting if symptoms occur post-result; invalid ones need a new test or professional consultation if unresolved.
Affecting factors include timing of testing, efficient sample collection technique as well as precise storage & handling of kits that affect result dependability. This guide simplifies viral detection understanding for everyone to promote collective action towards the return to normal life.
Frequently Asked Questions
Is C or T positive for a COVID test?
The appearance of the 'C' (Control) line on a COVID test simply validates that the testing process has been correctly initiated and is functioning as it should. It does not contribute to identifying whether an individual is infected with COVID-19.
What are the lines on a COVID test result?
Typically, there are two lines applicable for interpreting a rapid antigen test result - the C (control) Line and the T (test) Line. The presence or absence of these lines helps determine if an individual tests positive or negative for SARS-CoV-2.
What does it mean when the T line is darker than the C line in COVID?
If both C-line and T-Line appear in quick test results, it signifies a positive outcome, meaning active infection by the COVID-19 virus regardless of their darkness compared to each other.
How does a positive COVID test look?
A visible Test line generally indicates a positive result in most cases irrespective of how dark light appears relative to Control distinct alongside suggests ongoing Lastly note darker denser suggests higher viral loads present but doesn't alter the interpretation essentially deeming the patient as having current disease status.









 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews