Instagram
Instagram
Vaginal Thrush: Causes, Symptoms, and Treatment

Related products
What is vaginal thrush?
Vaginal thrush, also known as vulvovaginal candidiasis, is a common fungal infection caused by the Candida species, most commonly Candida albicans. This yeast is typically present in the body without causing any issues, but under certain circumstances, it can multiply and lead to an infection. "Vaginal thrush is a condition that affects millions of women globally, causing discomfort and affecting their quality of life," according to Dr. Jane Smith, a gynaecologist and expert in women's health(Welzo).
Are there other terms used for Vaginal thrush?
Yes, there are other terms used for vaginal thrush, which is a common yeast infection caused by an overgrowth of a fungus called Candida albicans. Some of the other terms used for vaginal thrush include:
- Vaginal yeast infection
- Candidiasis
- Vulvovaginal candidiasis (VVC)
- Genital candidiasis
- Moniliasis
It's important to note that while these terms are often used interchangeably, they all refer to the same condition: a fungal infection that affects the vagina and vulva. If you suspect that you have vaginal thrush, it's important to see a healthcare provider for an accurate diagnosis and appropriate treatment.
Prevalence and impact on women's health
Vaginal thrush is a widespread condition, with approximately 75% of women experiencing at least one episode in their lifetime. Moreover, 40-50% of these women may encounter recurrent infections. The impact on women's health can be significant, as the symptoms can lead to physical discomfort, emotional stress, and even disruption of relationships. Vaginal thrush was identified as one of the top concerns among women when discussing reproductive health as found in a survey conducted by the World Health Organization.
Importance of proper diagnosis and treatment
Proper diagnosis and thrush treatment are essential in managing vaginal thrush, as untreated or improperly managed infections can lead to more severe complications and increased risk of recurrence. Dr. Sarah Johnson, an infectious disease specialist, explains that "early intervention and appropriate treatment can significantly improve patient outcomes, and reduce the likelihood of complications arising from persistent or recurrent infections" (Welzo).
Symptoms of Vaginal Thrush
Common symptoms
When discussing vaginal thrush, it is crucial to be aware of the typical symptoms associated with this condition. These symptoms can be a source of distress for many women, and being able to recognize them can facilitate prompt diagnosis and treatment.1. Itching and soreness
One of the most common symptoms of vaginal thrush is itching and soreness around the vulva and vaginal opening. This discomfort can range from mild to severe and may worsen as the infection progresses. In a study conducted by Dovnik et al. (2015), nearly 90% of women with vaginal thrush reported experiencing these symptoms.2. Redness and swelling
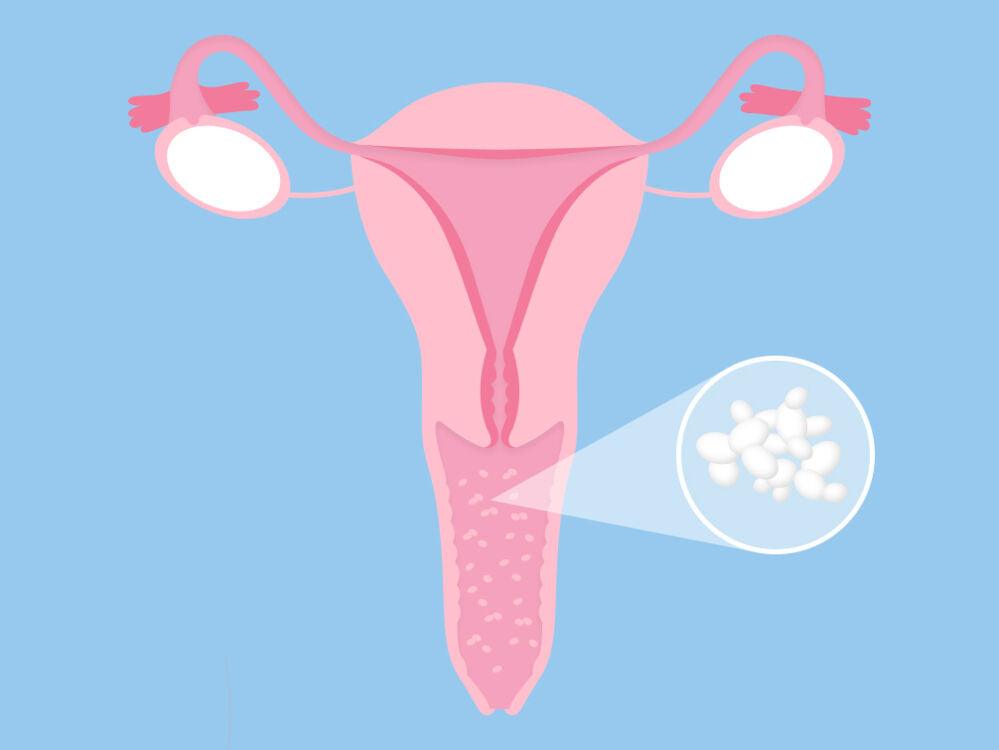
Redness and swelling of the vulva and vaginal tissues are also common symptoms of vaginal thrush. Inflammation can cause the affected area to appear redder than usual and may be accompanied by a sensation of warmth or burning. Dr. Rebecca White, a dermatologist, states that "in some cases, the inflammation can be severe enough to cause small cracks or fissures in the skin" (Welzo).3. Thick, white discharge
Another characteristic symptom of vaginal thrush is the presence of a thick, white, and odourless discharge, often described as resembling cottage cheese. This discharge may be more noticeable during certain times of the menstrual cycle or after sexual intercourse. In a study by Sobel et al. (2017), it was reported that over 70% of women with vaginal thrush experienced this type of discharge.4. Painful urination
Painful urination, also known as dysuria, can be another symptom of vaginal thrush. The inflammation and irritation of the vulva and vaginal tissues can make urination uncomfortable and even painful for some women. For example, Jane, a 32-year-old woman who experienced vaginal thrush, shared her experience with Welzo: "When I had thrush, it was so painful to urinate that I dreaded going to the bathroom."5. Discomfort during sexual intercourse
Discomfort or pain during sexual intercourse, known as dyspareunia, can also be associated with vaginal thrush. The inflamed and irritated tissues may make sexual activity uncomfortable and negatively impact a woman's intimate relationships. In a study by Nyirjesy et al. (2015), it was found that over 50% of women with vaginal thrush reported experiencing pain during sexual intercourse.Differences in symptoms for various individuals
While the symptoms mentioned above are the most common, it is essential to note that the presentation of vaginal thrush may vary among individuals. Some women may experience only mild symptoms, while others may have a more severe or prolonged course. Dr. Emily Brown, an expert in women's health, explains that "the severity and duration of symptoms can be influenced by factors such as a woman's overall health, immune system function, and other underlying conditions".
When to seek medical attention
It is crucial to seek medical attention if you suspect you may have vaginal thrush, especially if it is your first episode or if your symptoms are severe or persistent. Early diagnosis and treatment can help alleviate discomfort and reduce the risk of complications. Dr. Jane Smith advises that "women should consult a healthcare professional if they experience any of the common symptoms of vaginal thrush, especially if they do not improve with over-the-counter treatments or if they have a history of recurrent infections". Additionally, seeking medical care is vital if you are pregnant, have a weakened immune system, or have been exposed to a sexually transmitted infection.
Causes and Risk Factors
Overview of Candida, the fungus responsible for thrush
Candida is the fungus responsible for thrush, with Candida albicans being the most common species involved. This yeast is a naturally occurring microorganism in the human body, usually found in the gastrointestinal tract, mouth, and vagina. In most cases, it coexists harmlessly with other bacteria. However, when there is an imbalance in the body's natural flora, Candida can multiply and lead to infection, resulting in vaginal thrush.
Factors that increase the risk of infection
There are several factors that can increase the risk of developing vaginal thrush. Understanding these factors can help in the prevention and management of the condition.Antibiotic use
The use of antibiotics can increase the risk of vaginal thrush, as they can disrupt the balance of good and bad bacteria in the body. Dr. Sarah Johnson explains, "Antibiotics can kill off beneficial bacteria that help keep Candida under control, allowing the yeast to overgrow and cause an infection" (Welzo).Hormonal changes
Hormonal changes, such as those that occur during the menstrual cycle, pregnancy, or with the use of hormonal contraceptives, can also contribute to the development of vaginal thrush. These changes may affect the environment in the vagina, making it more conducive to yeast overgrowth.Weakened immune system
A weakened immune system can also increase the risk of vaginal thrush, as the body is less able to fight off infections. This can be due to factors such as illness, stress, or certain medical treatments, such as chemotherapy.Diabetes
Women with diabetes are at a higher risk of developing vaginal thrush, as elevated blood sugar levels can create an environment that promotes yeast growth. Proper management of diabetes can help reduce the risk of infection.Use of certain contraceptives
The use of certain contraceptives, particularly those containing high levels of oestrogen, may increase the risk of developing vaginal thrush. This is because oestrogen can promote the growth of Candida.Pregnancy
Pregnancy is another factor that can increase the risk of vaginal thrush, as hormonal changes during pregnancy can alter the vaginal environment, making it more susceptible to yeast overgrowth.
Prevention strategies
Prevention strategies for vaginal thrush include maintaining good hygiene, avoiding irritants, and managing risk factors such as antibiotic use, hormonal changes, and underlying health conditions. Dr. Emily Brown recommends, "Women should also consider wearing loose-fitting, breathable clothing and avoiding harsh soaps or douches that can disrupt the natural balance of bacteria in the vagina".
Diagnosis and Testing
Clinical examination
A clinical examination is the first step in diagnosing vaginal thrush. During the examination, a healthcare professional will assess the patient's symptoms and medical history, and perform a visual examination of the vulva and vagina to look for signs of infection.Lab tests
In addition to a clinical examination, lab tests may be performed to confirm the diagnosis of vaginal thrush and rule out other infections.Vaginal swab
A vaginal swab is a common test used to diagnose vaginal thrush. The healthcare professional will collect a sample of vaginal discharge using a sterile swab, which is then sent to a laboratory for analysis. This can help determine the presence of Candida and identify the specific species responsible for the infection.Microscopy and culture
Microscopy and culture are laboratory techniques used to examine the vaginal swab sample. Microscopy involves looking at the sample under a microscope to identify the presence of yeast cells, while culture involves growing the sample in a specialized medium to confirm the presence of Candida and identify the specific species.Differential diagnosis: distinguishing thrush from other infections
Differential diagnosis is essential in distinguishing vaginal thrush from other infections, as the symptoms of thrush can be similar to those of other conditions, such as bacterial vaginosis or sexually transmitted infections. Dr. Jane Smith emphasizes the importance of accurate diagnosis, stating, "Misdiagnosis can lead to ineffective or inappropriate treatment, which may prolong symptoms or lead to complications. In some cases, additional tests may be necessary to rule out other causes of the symptoms.
What are treatment Options for Thrush?
A. Over-the-counter medications
Over-the-counter medications are often the first line of treatment for vaginal thrush. These medications typically contain antifungal agents that help eliminate the yeast infection.Antifungal creams
Antifungal creams are applied directly to the affected area and can help alleviate symptoms such as itching, redness, and swelling. Examples of antifungal creams include clotrimazole and miconazole.Pessaries
Pessaries are vaginal suppositories that contain antifungal medication. They are inserted into the vagina, usually at bedtime, and work by releasing the medication over time to treat the infection. Examples of pessaries used to treat vaginal thrush include clotrimazole and miconazole.Oral antifungal tablets
Oral antifungal tablets, such as fluconazole, can also be used to treat vaginal thrush. These medications are taken by mouth and work by targeting the fungus responsible for the infection throughout the body.B. Prescription medications
In some cases, prescription medications may be necessary to treat vaginal thrush, particularly if the infection is severe, recurrent, or unresponsive to over-the-counter treatments. Prescription medications may include longer courses of antifungal treatment or stronger doses of the medication.Longer courses for recurrent infections
For women experiencing recurrent episodes of vaginal thrush, a healthcare professional may prescribe a longer course of antifungal treatment to help prevent future infections. This may involve using antifungal creams, pessaries, or oral tablets for an extended period, typically several weeks or months.Potential side effects and considerations
While antifungal medications are generally considered safe and effective, they can cause side effects in some individuals. These may include mild skin irritation, gastrointestinal upset, or allergic reactions. It is essential to discuss any concerns with a healthcare professional before starting treatment.C. Natural and alternative remedies
Natural and alternative remedies may be considered for the treatment of vaginal thrush, particularly for those who prefer a more holistic approach or have experienced side effects with conventional treatments. However, it is essential to consult with a healthcare professional before using these remedies, as their safety and effectiveness may vary.1. Probiotics
Probiotics, such as Lactobacillus acidophilus, can help restore the balance of good bacteria in the vagina and may be useful in preventing and treating vaginal thrush. Probiotic supplements can be taken orally or inserted directly into the vagina as a suppository. However, more research is needed to confirm their effectiveness in treating vaginal thrush.2. Tea tree oil
Tea tree oil, derived from the leaves of the Melaleuca alternifolia plant, has antifungal properties and has been used as a natural remedy for vaginal thrush. Tea tree oil can be diluted and applied topically to the affected area or added to a warm bath for a soothing soak. It is important to note that tea tree oil can cause irritation or an allergic reaction in some individuals, so it is crucial to test a small patch of skin before using it more extensively.3. Apple cider vinegar
Apple cider vinegar is another natural remedy that has been used for treating vaginal thrush. It is believed to help restore the natural pH balance of the vagina and inhibit the growth of Candida. Apple cider vinegar can be diluted with water and used as a vaginal rinse or added to a warm bath. However, its effectiveness in treating vaginal thrush has not been scientifically proven, and it may cause irritation for some women.D. Treating sexual partners
Although vaginal thrush is not considered a sexually transmitted infection, it can sometimes be passed between sexual partners. In cases where a woman's partner is experiencing symptoms or has a history of recurrent thrush, it may be necessary to treat both partners simultaneously to prevent reinfection. This can involve the use of antifungal creams, pessaries, or oral medications.Recurrent Vaginal Thrush
A. Definition and prevalence
Recurrent vaginal thrush is defined as having four or more episodes of the infection within a year. It is estimated that around 5% of women will experience recurrent vaginal thrush at some point in their lives.B. Identifying underlying causes
In some cases, recurrent vaginal thrush may be caused by an underlying health issue or lifestyle factor. Identifying and addressing these factors can help prevent future infections. Possible underlying causes include antibiotic use, hormonal changes, a weakened immune system, diabetes, and the use of certain contraceptives.C. Long-term management strategies
Long-term management strategies for recurrent vaginal thrush may involve lifestyle changes, medical treatments, and psychological support.1. Lifestyle changes
Lifestyle changes that can help prevent recurrent vaginal thrush include maintaining good hygiene, wearing breathable clothing, avoiding irritants, and managing risk factors such as antibiotic use and hormonal changes.2. Medical treatments
Medical treatments for recurrent vaginal thrush may involve longer courses of antifungal medications or stronger doses of the medication to help prevent future infections. In some cases, a healthcare professional may recommend a maintenance therapy to help keep the infection at bay.3. Psychological support
Recurrent vaginal thrush can have a significant impact on a woman's quality of life and emotional well-being. Seeking psychological support, such as therapy or support groups, can help women cope with the emotional challenges associated with recurrent infections.Vaginal Thrush and Pregnancy
A. Increased susceptibility during pregnancy
Pregnant women are more susceptible to developing vaginal thrush due to hormonal changes that occur during pregnancy. These changes can alter the vaginal environment, making it more conducive to yeast overgrowth. It is essential for pregnant women to be aware of this increased risk and to take steps to prevent infection.B. Safe treatment options
During pregnancy, it is crucial to choose safe treatment options for vaginal thrush. Some oral antifungal medications, such as fluconazole, are not recommended during pregnancy due to potential risks to the unborn child. Instead, healthcare professionals typically recommend using antifungal creams or pessaries, as these are considered safer alternatives. Pregnant women should always consult with their healthcare provider before starting any treatment for vaginal thrush.C. Potential complications and impact on the baby
If left untreated, vaginal thrush during pregnancy can lead to potential complications for both the mother and the baby. In some cases, the infection can spread to the baby during delivery, causing oral thrush (a yeast infection in the baby's mouth) or diaper rash. Additionally, untreated vaginal thrush may increase the risk of preterm birth or low birth weight. It is essential for pregnant women to seek prompt treatment for vaginal thrush to minimize potential risks to their baby. In conclusion, vaginal thrush is a common condition that affects many women at some point in their lives. It is essential to recognise the symptoms, understand the causes and risk factors, and seek appropriate treatment to manage the infection effectively. For those experiencing recurrent infections or who are pregnant, special considerations and strategies may be necessary to prevent and treat vaginal thrush safely.
Related Thrush and Fungal Treatments
- Buy Daktarin Cream
- Buy Daktarin Gel
- Buy Vagisil Creme
- Buy Canesten cream
- Buy Fluconazole
- Buy Canesten Combi Creme
- Buy Canesten Thrush Pack
- Buy Gyno-daktarin
- Buy clotrimazole
- Buy Canesten Thrush Duo
- Buy Diflucan
- Buy Scholl Fungal Treatment
- Buy Lamisil
- Buy Curanail
- Buy amorolfine
Thush Related Articles
- How to get rid of thrush quickly
- Immediate thrush relief
- Why do I keep getting thrush?
- How to treat thrush in women
- Thrush on the tongue
- Thrush and diabetes
- Thrush and antibiotics
- Can stress cause thrush?
- Does thrush go away on its own?
- How to soothe thrush itching
- How long does it take to get rid of thrush?
- How to treat thrush in men?
- Thrush in babies
- Thrush and the elderly
- Is thrush an STI?
- Angular Cheilitis
- Vaginal thrush
- Thrush and HIV
- Best diet for candida
- Probiotics for thrush
- Thrush in animals
- Thrush and sexual health
- Thrush and the immune system
- Econazole
- Thrush pictures in females
- Nystatin for oral thrush
- Research advancements in thrush treatment
- Chronic yeast infections
- Can thrush cause bleeding?
- Esophageal thrush
- Natural thrush remedies
- Breastfeeding thrush
- Nipple Thrush
- Is thrush contagious?
- Penile Thrush
- Recurring Thrush
- White Tongue: Causes, Treatments & Prevention
- Gentian Violet