Recurring Thrush: Causes, Treatment, and Prevention


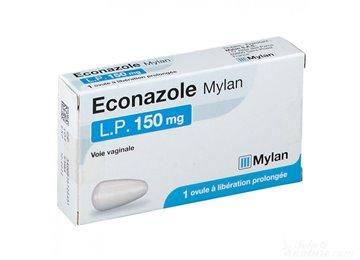
Related products
What is Recurring Thrush?
Recurring thrush is a common and often distressing condition caused by an overgrowth of Candida fungus, typically Candida albicans. It is characterised by frequent episodes of itching, irritation, and inflammation of the affected area, most commonly the genitals or mouth. Recurring thrush can significantly impact a person's quality of life, making it essential to understand the causes, treatment options, and preventive measures to manage this condition effectively. This article will explore the various factors contributing to recurring thrush, the role of Candida fungus, and how to address the issue through medical and lifestyle interventions.
Importance of Understanding and Addressing Recurring Thrush
Thrush can be a distressing and disruptive condition, particularly when it recurs frequently. By understanding the underlying causes and triggers, individuals can take proactive steps to minimise the risk of recurrence and improve their overall health and wellbeing. Moreover, addressing recurring thrush is crucial to prevent potential complications, such as invasive candidiasis or emotional and psychological consequences. Gaining a comprehensive understanding of recurring thrush also enables healthcare professionals to provide appropriate care and support to those affected.
Overview of the Article
This article aims to provide a comprehensive guide to recurring thrush, covering its causes, symptoms, treatment options, and preventive measures. It will also delve into the role of Candida fungus in the development of thrush and discuss how various factors, such as antibiotic use, hormonal imbalances, and diabetes, contribute to the condition. Additionally, the article will include expert quotes, statistics, and relevant hyperlinks to provide readers with a thorough understanding of the topic.
What is Candida Fungus?
Candida is a group of fungi that naturally reside on the human body, primarily on the skin and mucous membranes. Candida albicans is the most common species, although other species like Candida glabrata and Candida tropicalis can also cause infections. Under normal circumstances, the growth of Candida is kept in check by the body's immune system and beneficial bacteria. However, certain factors can disrupt this balance, leading to an overgrowth of Candida and causing thrush.
Candida Albicans
Candida albicans is the most prevalent species of Candida fungus responsible for causing thrush. It is a commensal organism, meaning it typically coexists harmlessly with other microorganisms in the body. However, when the delicate balance of the body's microbial ecosystem is disturbed, Candida albicans can multiply and cause infections, leading to symptoms such as itching, irritation, and inflammation.
Other Candida Species
While Candida albicans is the most common species causing thrush, other Candida species can also be responsible for the condition. These species include Candida glabrata, Candida tropicalis, and Candida krusei, among others. Although less common, infections caused by these species can be more challenging to treat due to their resistance to certain antifungal medications.
Common Factors Contributing to Recurring Thrush
Several factors can contribute to the recurrence of thrush, ranging from medical conditions and medications to lifestyle habits. Understanding these factors can help individuals take appropriate steps to minimise their risk of developing recurring thrush.
Antibiotic Use and Thrush
Antibiotics are medications used to treat bacterial infections. While they are effective in killing harmful bacteria, they can also disrupt the balance of beneficial bacteria in the body.
This disruption allows Candida to multiply and thrive, leading to an increased risk of developing thrush. Prolonged or frequent use of antibiotics can further exacerbate this issue, making it more likely for thrush to recur.
Hormonal Imbalances and Thrush
Hormonal fluctuations can also contribute to the recurrence of thrush. Women are particularly susceptible to thrush during certain stages of their menstrual cycle, pregnancy, or menopause, when hormone levels change significantly. Hormonal imbalances can alter the environment in the vagina or mouth, making it more conducive to the growth of Candida, resulting in recurring thrush episodes.
Weakened Immune System and Thrush
Individuals with weakened immune systems, such as those with chronic illnesses, autoimmune disorders, or undergoing treatments like chemotherapy, are at a higher risk of developing recurring thrush. A compromised immune system may be unable to effectively control Candida growth, allowing the fungus to proliferate and cause infections more easily.
Diabetes and Thrush
Diabetes can also play a significant role in the development of recurring thrush. High blood sugar levels can promote the growth of Candida, making it more difficult for the body to keep the fungus under control. Furthermore, individuals with diabetes may have weakened immune systems, further increasing their susceptibility to thrush. Proper diabetes management can help reduce the risk of recurrent thrush episodes.
Poor Hygiene and Thrush
Poor hygiene practices can contribute to the development and recurrence of thrush. Inadequate cleansing of the genital area or using harsh soaps can disrupt the natural balance of microorganisms, creating an environment where Candida can thrive. Maintaining good personal hygiene, including regular and gentle cleaning of the affected area, can help reduce the risk of recurring thrush.
Use of Irritants and Thrush
Exposure to certain irritants, such as scented soaps, bubble baths, or perfumed sanitary products, can also lead to recurring thrush. These products can cause irritation and inflammation, making the affected area more susceptible to Candida overgrowth. By avoiding potential irritants and opting for hypoallergenic alternatives, individuals can minimise their risk of developing recurring thrush.
Stress and Thrush
Stress can have a significant impact on the immune system, making it more difficult for the body to control Candida growth effectively. High levels of stress can also trigger hormonal imbalances, further increasing the risk of recurring thrush. Implementing stress management techniques, such as exercise, meditation, and counselling, can help improve overall health and reduce the likelihood of thrush recurrence.
Recurring Thrush after Intercourse
Some individuals may experience recurring thrush after sexual intercourse. This can occur due to the transfer of Candida between partners or irritation caused by sexual activity. Practicing safe sex, using barrier methods like condoms, and maintaining good personal hygiene can help reduce the risk of thrush recurrence after intercourse.
Recurring Thrush before Period
Some women may notice recurring thrush episodes before their period. This is likely due to hormonal fluctuations that can create an environment conducive to Candida growth. Tracking menstrual cycles and working with a healthcare professional to address hormonal imbalances can help manage and prevent thrush recurrence in such cases.
Recurring Thrush in Pregnancy
Pregnant women are at an increased risk of developing recurring thrush due to hormonal changes and a weakened immune system. To manage thrush during pregnancy, it is essential to consult a healthcare professional for appropriate treatment options and follow proper hygiene practices. In some cases, medical professionals may recommend specific antifungal medications or lifestyle changes to address the issue safely and effectively during pregnancy.
Symptoms of Recurring Thrush
Physical Symptoms
Recurring thrush can present various physical symptoms, including:
- Itching and irritation
- Redness and swelling
- White, curd-like discharge
- Pain during urination and sexual intercourse
Emotional and Psychological Symptoms
Aside from physical symptoms, recurring thrush can also have emotional and psychological impacts, such as:
- Anxiety and embarrassment
- Impact on sexual relationships
Diagnosis and Monitoring of Recurring Thrush
Medical History and Physical Examination
To diagnose recurring thrush, healthcare professionals will typically begin by taking a thorough medical history and performing a physical examination. This will help them identify potential underlying causes and rule out other conditions that may present similar symptoms.
Laboratory Tests
In some cases, laboratory tests may be necessary to confirm the diagnosis of recurring thrush. These tests can include swab tests, which involve collecting a sample of the affected tissue or discharge for analysis. The samples are then cultured and examined under a microscope to identify the presence of Candida fungus. Laboratory tests can also help determine the specific Candida species responsible for the infection, which can be crucial for selecting the most effective treatment options.
Swab Test for Recurring Thrush
A swab test is a common diagnostic tool used by healthcare professionals to identify the presence of Candida fungus in cases of recurring thrush. The swab is gently taken from the affected area and then sent to a laboratory for analysis, where the presence and type of Candida fungus can be identified.
Blood Tests for Recurring Thrush
Blood tests can help determine if there are any underlying health issues that may be contributing to recurring thrush, such as diabetes or a weakened immune system. By addressing these underlying conditions, individuals can reduce their risk of developing recurrent infections.
Urine Tests for Recurring Thrush
Urine tests can be useful in identifying the presence of Candida in the urinary tract, which could be a factor in recurrent thrush infections. This information can help healthcare professionals determine the most effective treatment approach for each individual case.
Identifying Triggers and Underlying Factors
Understanding and addressing the triggers and underlying factors that contribute to recurring thrush is crucial for effective prevention and management. This may include factors such as antibiotic use, hormonal imbalances, weakened immune system, and lifestyle habits. By identifying and addressing these factors, individuals can significantly reduce their risk of recurring thrush.
Conditions That Can Be Mistaken for Thrush
Several conditions can present similar symptoms to thrush, making accurate diagnosis essential for effective treatment. Some of these conditions include:
Bacterial Vaginosis
Bacterial vaginosis is a common vaginal infection caused by an imbalance of bacteria in the vagina. Although it can cause symptoms similar to thrush, such as itching and discharge, it requires a different treatment approach.
Dermatitis
Dermatitis is an inflammation of the skin that can be triggered by a variety of factors, including irritation from certain products or allergens. The symptoms of dermatitis, such as redness and itching, can be similar to those of thrush, but the condition requires different management strategies.
Sexually Transmitted Infections
Some sexually transmitted infections (STIs) can cause symptoms that resemble thrush, such as itching, redness, and discharge. Accurate diagnosis and appropriate treatment for the specific STI are essential to ensure the condition is effectively managed.
Treatment Options for Recurring Thrush
There are several treatment options available for recurring thrush, including:
Antifungal Medications
Topical creams and ointments, as well as oral antifungal medications like fluconazole, can be prescribed to treat recurring thrush. These medications work by targeting the Candida fungus responsible for the infection.
Probiotic Supplements
Probiotic supplements can help restore the balance of beneficial bacteria in the body, which may help prevent the overgrowth of Candida fungus and reduce the risk of recurring thrush.
Lifestyle Changes
Implementing lifestyle changes, such as improved hygiene, diet modifications, and stress management, can help address some of the underlying factors that contribute to recurring thrush and improve overall health.
Recurring Thrush Treatment During Menopause
During menopause, hormonal changes can increase the risk of developing thrush. In these cases, treatment options may include hormone replacement therapy (HRT) alongside antifungal medications to
address both the hormonal imbalances and the Candida infection. It is essential for individuals experiencing recurring thrush during menopause to consult with their healthcare provider to determine the most appropriate treatment approach.Prevention Strategies for Recurring Thrush
Implementing prevention strategies can help reduce the risk of recurring thrush. Some effective prevention measures include:
- Practicing good personal hygiene: Regularly washing the genital area with mild, unscented soap and water, and drying thoroughly can help prevent the growth of Candida.
- Maintaining a healthy diet: Consuming a balanced diet that is low in sugar and processed foods can help support a healthy immune system and reduce the risk of Candida overgrowth.
- Managing stress: Practicing stress management techniques, such as meditation, exercise, or therapy, can help support overall health and wellbeing, reducing the risk of recurring thrush.
- Using barrier protection during intercourse: Using condoms can help reduce the risk of transmitting Candida between sexual partners, potentially preventing recurring thrush.
- Regular check-ups: Scheduling regular check-ups with a healthcare professional can help identify any underlying health issues that may be contributing to recurring thrush and allow for early intervention.
Prevention Strategies for Recurring Thrush
Implementing various prevention strategies can help reduce the risk of recurring thrush:
Maintaining a healthy immune system
Supporting a healthy immune system through a balanced diet, regular exercise, and sufficient sleep can help prevent the overgrowth of Candida fungus and reduce the risk of recurring thrush.
Proper hygiene practices
Practicing good personal hygiene, such as regularly washing the genital area with mild, unscented soap and water and drying thoroughly, can help prevent the growth of Candida.
Avoiding irritants
Avoiding the use of irritants, such as harsh soaps, douches, and scented feminine products, can help prevent irritation and inflammation that may contribute to recurring thrush.
Safe sexual practices
Using barrier protection, such as condoms, during intercourse can help reduce the risk of transmitting Candida between sexual partners and prevent recurring thrush.
Regular medical check-ups
Scheduling regular check-ups with a healthcare professional can help identify any underlying health issues that may be contributing to recurring thrush and allow for early intervention.
Proper diabetes management
Individuals with diabetes should carefully manage their blood sugar levels, as high blood sugar can contribute to the overgrowth of Candida fungus and increase the risk of recurring thrush.
Stress reduction techniques
Practicing stress management techniques, such as meditation, exercise, or therapy, can support overall health and wellbeing, reducing the risk of recurring thrush.
How to stop recurring thrush
Implementing the prevention strategies outlined above, along with appropriate medical treatment, can help stop recurring thrush and improve overall health.
How to soothe thrush itching
To soothe itching caused by thrush, individuals can apply cold compresses to the affected area, take over-the-counter antihistamines, and avoid scratching the area, which can worsen symptoms and prolong healing.
Potential Complications of Recurring Thrush
Recurring thrush can lead to several potential complications:
Chronic infections
Repeated thrush infections can become chronic, causing ongoing discomfort and potentially impacting an individual's overall wellbeing.
Invasive candidiasis
In severe cases, Candida fungus can enter the bloodstream and cause invasive candidiasis, a serious and potentially life-threatening infection that requires immediate medical attention.
Emotional and psychological consequences
Recurring thrush can lead to anxiety, embarrassment, and negative impacts on mental health and relationships.
Impact on fertility and sexual health
Untreated or poorly managed thrush can potentially impact fertility and sexual health, making it essential to seek appropriate medical care.
Recurring Thrush in Specific Populations
Recurring thrush can affect various populations differently:
Pregnant women
Pregnant women may be more susceptible to thrush due to hormonal changes that can alter the balance of bacteria and yeast in the vagina. Treatment options during pregnancy should be discussed with a healthcare professional to ensure the safety of both the mother and the baby
Recurring thrush in men
Men can also experience recurring thrush, often presenting as itching, redness, and irritation on the head of the penis or the foreskin. Risk factors for men include antibiotic use, a weakened immune system, diabetes, and poor hygiene. Treatment options and prevention strategies are similar to those for women, with antifungal medications and lifestyle changes playing a crucial role.
Recurring thrush in babies
Babies can experience recurring thrush, commonly presenting as oral thrush or diaper rash. Ensuring proper hygiene, frequent diaper changes, and the use of antifungal creams can help manage and prevent recurring thrush in babies.
Recurring oral thrush
Recurring oral thrush presents as white, creamy patches in the mouth, often accompanied by soreness and difficulty swallowing. Risk factors include a weakened immune system, diabetes, and the use of certain medications. Treatment options include antifungal mouthwashes, lozenges, and oral medications, along with maintaining proper oral hygiene.
Recurring nipple thrush
Nipple thrush, often experienced by breastfeeding mothers, presents as redness, itching, and pain on the nipples. Treatment options include topical antifungal creams, oral medications, and ensuring proper hygiene practices. It is essential to treat both the mother and the baby simultaneously to prevent re-infection.
Frequently Asked Questions
Why does my thrush keep coming back?
Recurring thrush can be caused by various factors, including a weakened immune system, hormonal imbalances, antibiotic use, diabetes, and poor hygiene. Identifying and addressing these factors can help prevent thrush from coming back.
Can recurring thrush be something else?
Some conditions, such as bacterial vaginosis, dermatitis, or sexually transmitted infections, can present with similar symptoms to thrush. Accurate diagnosis and appropriate treatment for the specific condition are essential for effective management.
Can recurring thrush be a sign of cancer?
Recurring thrush is not typically a sign of cancer; however, it can be associated with a weakened immune system. If you are concerned about your risk for cancer, it is important to consult with your healthcare provider for proper evaluation.
How long does it take for recurring thrush to clear up?
The duration of thrush treatment can vary depending on the severity of the infection and the chosen treatment method. Most cases of thrush resolve within 7 to 14 days with appropriate treatment, but recurrent cases may require longer treatment durations or additional interventions.
How to treat recurring thrush
Recurring thrush can be treated using antifungal medications, probiotic supplements, and lifestyle changes, such as improved hygiene, diet modifications, and stress management. It is essential to work with a healthcare professional to determine the most appropriate treatment approach for each individual case.
Conclusion
Recap of key points
Recurring thrush is a common and often frustrating condition. Understanding the causes, treatment options, and prevention strategies can help individuals effectively manage and prevent future episodes.
Importance of early detection and intervention
Early detection and intervention are crucial in managing recurring thrush and preventing potential complications. Regular medical check-ups and prompt treatment of symptoms can help ensure
effective management of the condition.
Encouragement to seek medical help and maintain a healthy lifestyle to prevent recurring thrush
Individuals experiencing recurring thrush should seek medical help to determine the underlying causes and receive appropriate treatment. Maintaining a healthy lifestyle, practicing good hygiene, and implementing prevention strategies can help reduce the risk of future episodes and improve overall wellbeing.
Related Thrush and Fungal Treatments
- Buy Daktarin Cream
- Buy Daktarin Gel
- Buy Vagisil Creme
- Buy Canesten cream
- Buy Fluconazole
- Buy Canesten Combi Creme
- Buy Canesten Thrush Pack
- Buy Gyno-daktarin
- Buy clotrimazole
- Buy Canesten Thrush Duo
- Buy Diflucan
- Buy Scholl Fungal Treatment
- Buy Lamisil
- Buy Curanail
- Buy amorolfine
Thush Related Articles
- How to get rid of thrush quickly
- Immediate thrush relief
- Why do I keep getting thrush?
- How to treat thrush in women
- Thrush on the tongue
- Thrush and diabetes
- Thrush and antibiotics
- Can stress cause thrush?
- Does thrush go away on its own?
- How to soothe thrush itching
- How long does it take to get rid of thrush?
- How to treat thrush in men?
- Thrush in babies
- Thrush and the elderly
- Is thrush an STI?
- Angular Cheilitis
- Vaginal thrush
- Thrush and HIV
- Best diet for candida
- Probiotics for thrush
- Thrush in animals
- Thrush and sexual health
- Thrush and the immune system
- Econazole
- Thrush pictures in females
- Nystatin for oral thrush
- Research advancements in thrush treatment
- Chronic yeast infections
- Can thrush cause bleeding?
- Esophageal thrush
- Natural thrush remedies
- Breastfeeding thrush
- Nipple Thrush
- Is thrush contagious?
- Penile Thrush
- Recurring Thrush
- White Tongue: Causes, Treatments & Prevention
- Gentian Violet






















 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews