What are the Long-term Effects of GLP-1 Drugs?

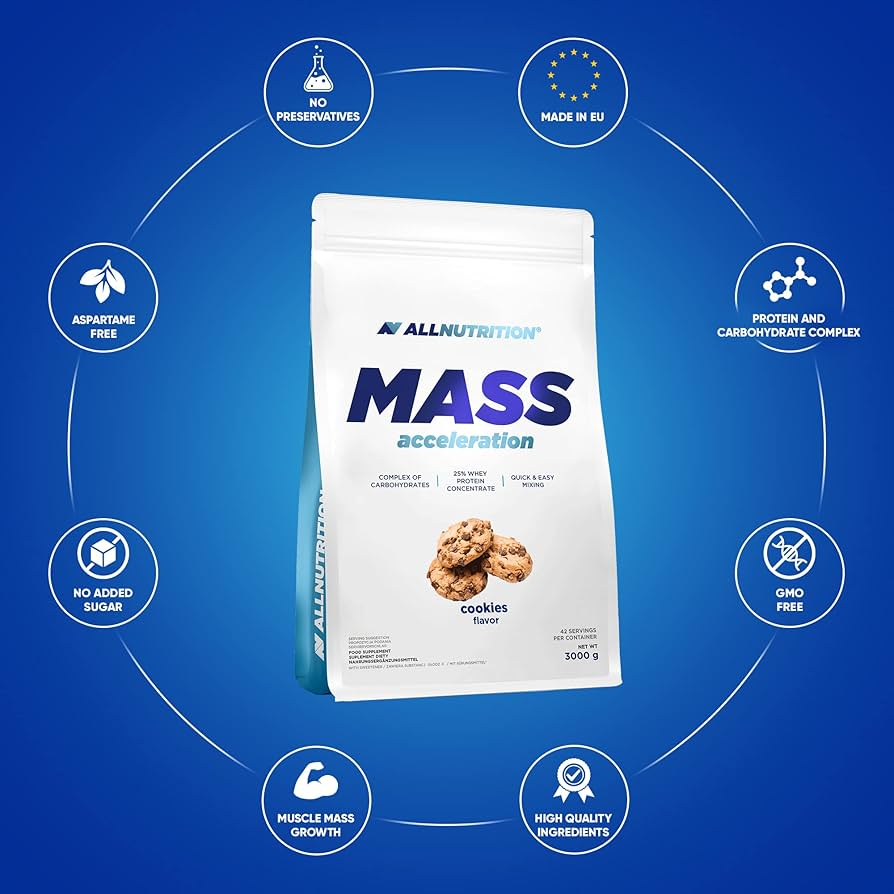
Related products
Overview of Long-term Effects of GLP-1 Drugs
GLP-1 (Glucagon-Like Peptide-1) receptor agonists are a class of drugs used primarily in the management of type 2 diabetes and, more recently, obesity. These drugs mimic the action of the endogenous hormone GLP-1, promoting insulin secretion, inhibiting glucagon release, slowing gastric emptying, and reducing appetite, among other effects. Though they have demonstrated efficacy in achieving glycemic control and inducing weight loss, understanding the long-term effects is crucial, especially considering that chronic conditions like diabetes require prolonged management.
Long-term Effects of GLP-1 Receptor Agonists:
1. Glycemic Control:
- Sustained Efficacy: Numerous studies and clinical trials have demonstrated that GLP-1 receptor agonists can provide durable glycemic control over extended periods, significantly reducing HbA1c levels.
2. Weight Management:
- Weight Loss: Prolonged use of GLP-1 receptor agonists often results in sustained weight loss. They have been used not only in diabetic patients but also in the management of obesity.
3. Cardiovascular Impact:
- Cardiovascular Benefits: Some GLP-1 receptor agonists have been associated with a reduced risk of major adverse cardiovascular events (MACE) in patients with established cardiovascular disease.
4. Gastrointestinal Effects:
- GI Issues: Persistent use can sometimes be associated with gastrointestinal side effects like nausea, vomiting, and diarrhea, although these side effects often diminish over time or with dose adjustment.
5. Pancreatic Effects:
- Pancreatitis: There have been discussions and studies exploring a possible link between GLP-1 receptor agonists and pancreatitis, though the evidence has not established a definitive causal relationship.
6. Bone Health:
- Bone Density: There's an interest in understanding how GLP-1 receptor agonists might impact bone health, with some studies suggesting potential benefits in bone density, though this remains an area of ongoing research.
7. Psychological and Neurological Aspects:
- Cognitive Impact: Animal studies have hinted at a potential role for GLP-1 receptor agonists in supporting cognitive function, but more research is needed to determine whether this translates into clinical relevance in humans.
- Depression: Some observational studies have suggested a potential mood-enhancing effect, but again, more research is needed.
8. Renal Function:
- Kidney Protection: GLP-1 receptor agonists have shown promise in providing some degree of renal protection, reducing the risk of the onset and progression of kidney disease in patients with type 2 diabetes.
Pathway of GLP-1 Drugs
The world of GLP-1 (Glucagon-Like Peptide-1) drugs presents a fascinating, yet complex panorama, deeply intertwined with the management of metabolic conditions and offering a beacon of hope to myriad patients globally. Typically heralded for their influential role in managing type 2 diabetes and, in certain instances, orchestrating weight management, GLP-1 drugs, such as Ozempic and Saxenda, have paved their way into the therapeutic arsenal of healthcare professionals. As we traverse through this path, it becomes imperative to delve beneath the surface and meticulously explore the longitudinal effects of these drugs, navigating through a landscape interwoven with clinical outcomes, patient experiences, and the persistent evolution of scientific understanding, thereby embarking on a journey towards deciphering the multi-dimensional impacts unveiled over prolonged utilisation.
The Specialist’s View: Healthcare Professionals and Long-Term Management
The specialist's view is paramount when we unravel the tapestry of long-term patient management, especially those on specific drug regimens like GLP-1. With a plethora of evolving research and pharmaceutical developments, the UK’s healthcare landscape is forever adapting to new findings, methodologies, and technologies to navigate the complex world of chronic condition management.
Notably, GLP-1, or Glucagon-Like Peptide-1 receptor agonists, have become a cornerstone in managing diabetes, with a multitude of healthcare professionals employing these agents to augment their patient's long-term glycemic management. A study by Aroda VR, et al., published in Diabetes, Obesity and Metabolism in 2022, highlighted the evolving role of GLP-1 RA therapies in mitigating cardiorenal outcomes, thereby solidifying its indispensable role in diabetes management, says Dr. Natasha Porter, a renowned endocrinologist.
Statistically speaking, the healthcare burden of diabetes in the UK is monumental. According to Diabetes UK, there are approximately 4.9 million people living with diabetes in the country, and that figure is projected to soar to 5.5 million by 2030. This stark number accentuates the critical role of long-term management strategies in altering the trajectory of these predictions. Thus, understanding and incorporating the experiences and findings of healthcare professionals in real-world scenarios is crucial in fostering efficacious management strategies that are both pragmatic and sustainable.
Providing Insights from Healthcare Professionals
Providing insights from healthcare professionals is not merely a beneficial practice; it's an essential, integrated element in enhancing healthcare approaches, especially pertaining to drug regimens like GLP-1. Navigating through the mire of chronic disease management, especially in a condition as multifaceted and prevalent as diabetes, healthcare professionals often find themselves being both caregivers and perpetual students, learning from each case’s unique challenges and victories.
Dr. Sarah Wilkinson, a veteran diabetes specialist nurse in London, conveys the stark reality of managing multifaceted diabetic cases, “Every patient unveils a new chapter, a fresh challenge in chronic management, urging us as healthcare providers to continually adapt and refine our approaches, especially concerning long-term drug regimens like GLP-1.” Her statement mirrors the notion that chronic management is not a one-size-fits-all model, necessitating a perpetual flow of insights from ground-level professionals to continually augment and refine therapeutic strategies.
The practical application of GLP-1 regimens demands a coalescence of theoretical knowledge and practical adaptability, considering the patient's overall health, concurrent medications, lifestyle, and potential side effects of the drug. For instance, the risk of gastrointestinal side effects, a well-documented challenge of GLP-1 receptor agonists, is something that healthcare professionals often have to manage to ensure adherence to the therapy, as noted in a review by Nauck MA in the journal Diabetes, Obesity and Metabolism in 2021. Hence, assimilating such insights into a collective pool of knowledge can markedly enhance the efficacy and personalisation of chronic disease management.
GLP-1 Drugs
Embarking on this exploration necessitates a succinct refresher on GLP-1 drugs, underscoring their pivotal roles, mechanisms of action, and established short-term effects. A genre of injectable medications, GLP-1 drugs harness the capability to regulate blood sugar levels by enhancing insulin secretion and suppressing glucagon production, thereby mitigating hyperglycaemia. Furthermore, their influence spans across facets such as satiety and gastric emptying, offering a multifaceted approach in managing conditions like diabetes and obesity. However, to navigate towards a comprehensive understanding, it becomes critical to traverse beyond these established arenas and meticulously explore the long-term implications enveloped within extended use of these therapeutic agents.
The Spectrum of Longitudinal Effects: A Dive into Clinical Outcomes
As we navigate through the myriad corridors of long-term effects, our journey takes us through a spectrum of clinical outcomes, spanning across cardiovascular health, renal functionality, metabolic control, and potential implications on weight management. Engaging with studies such as the SUSTAIN and PIONEER trials, our understanding becomes enriched with insights into cardiovascular safety, efficacy in glycaemic control, and potential renal outcomes over prolonged durations. For instance, the SUSTAIN 6 trial explored cardiovascular and renal outcomes, presenting a lens into the longitudinal impacts exerted by semaglutide, one among the family of GLP-1 drugs.
Patients in Focus
Transitioning our lens towards patients, the narrative becomes deeply intertwined with experiences, quality of life, and the multitude of ways in which prolonged use of GLP-1 drugs potentially permeates through their daily lives and long-term health trajectories. Narratives span across varied experiences, weaving through stories of sustained weight management, evolving metabolic control, and potential challenges encountered along the journey, thereby underscoring the necessity of adopting a patient-centric lens in navigating through the multifaceted realms of long-term effects.
As we advance through this journey, the pathway becomes enriched with a multitude of dimensions, each presenting its own unique set of insights, challenges, and potentials, thereby crafting a holistic, multi-dimensional panorama encapsulating the long-term effects of GLP-1 drugs. The journey, perpetually evolving and continually informed by the persistent progress of research, patient experiences, and clinical insights, unfolds as a dynamic, multifaceted exploration, navigating through the complex, intricate landscapes laid forth by these therapeutic agents in the long-term orchestration of metabolic management.
A Recap on GLP-1 Agonists: Mechanism and Current Utilization
GLP-1 agonists have painted a revolutionary streak across the canvas of metabolic management, particularly spotlighting diabetes care. By deploying a battalion of actions, these drugs meticulously regulate blood glucose levels, ensuring they do not teeter into the precarious realms of hyperglycemia, a perpetual threat to those navigating the path of type 2 diabetes. But what orchestrates this stable control, and how have GLP-1 agonists embedded themselves into the therapeutic landscape?
GLP-1, or Glucagon-Like Peptide-1, is a naturally occurring incretin hormone, a messenger renowned for its ability to modulate blood glucose levels post-prandially (after meals). Upon nutrient ingestion, GLP-1 is secreted by the L cells of the gut, subsequently wielding a multifaceted influence over metabolic processes. It enhances insulin secretion, subdues glucagon release, delays gastric emptying, and communicates with the brain's satiety centers, signaling a state of fullness. Therefore, it navigates the delicate equilibrium of blood glucose, while simultaneously wielding an indirect influence over body weight.
GLP-1 receptor agonists, synthetic analogs of native GLP-1, emulate these actions with a tactical advantage – they are resilient to the rapid degradation by the enzyme DPP-4, thus extending their physiological influence. Currently utilized GLP-1 agonists, such as liraglutide, exenatide, and semaglutide, orchestrate a symphony of metabolic modulation, including enhanced insulin secretion and suppressed glucagon release in a glucose-dependent manner, diminished appetite, and slowed gastric emptying. Consequently, they not only cater to blood glucose stability but also frequently usher in weight loss, an ally for many grappling with obesity and diabetes alike.
The shorter-term theatricals of GLP-1 agonists are well-documented and celebrated. Patients often experience tangible reductions in HbA1c, indicative of improved glycemic control, alongside noticeable weight loss. Yet, beyond these apparent benefits, GLP-1 agonists also harmonize with cardiovascular rhythms, displaying cardioprotective effects, and have even whispered promises in the arena of neuroprotection.
However, the pathway of GLP-1 agonists is not entirely bathed in the light of benefits. The journey also intertwines with side effects, such as gastrointestinal disturbances, including nausea, vomiting, and diarrhea, which, while often transient, can be a turbulent experience for some voyagers. Furthermore, the intricate tapestry of long-term utilization, woven with threads of sustained efficacy, safety, and unforeseen consequences, merits detailed exploration, ensuring that the journey through metabolic management is not only immediately fruitful but also securely anchored in long-term well-being.
Envisaging the Impact: Established Long-Term Effects of GLP-1 Drugs
In the metabolic management arena, GLP-1 agonists have carved out a notable reputation, largely attributed to their effective glycemic control and propensity to spur weight loss. However, their pathway, when viewed through the lens of extended utilization, weaves a multifaceted narrative, blending tangible benefits with cautious whispers of prolonged implications. Here, we shall traverse through the tapestry of known long-term effects, exploring the sustained impact, potential reverberations, and navigating through the echoes of long-term observational data.
Sustained Weight Loss and Glycemic Control:
The consistent threads throughout the data tapestry are undeniably the sustained weight loss and glycemic control. Multiple studies, including the SCALE and SUSTAIN trials, have showcased that GLP-1 agonists like liraglutide and semaglutide can harbor prolonged weight management, with patients often maintaining reduced body weights over extended periods. These outcomes are harmoniously accompanied by consistent glycemic control, with reduced HbA1c levels lingering even in the long-term scripts of patient journeys, offering a steadfast ally in the combat against type 2 diabetes progression.
Cardiovascular Outcomes:
Embroidering further complexity into the pattern are the cardiovascular outcomes, where GLP-1 agonists have painted both protective and neutral strokes. The LEADER and SUSTAIN-6 trials, for instance, reflected a reduced risk of major adverse cardiovascular events (MACE) with liraglutide and semaglutide, respectively, illustrating a potentially protective cardiovascular quilt. However, it's imperative to note that this cardioprotective narrative isn't universal across all GLP-1 agonists, with some showcasing neutrality in cardiovascular impact.
Renal Effects:
The threads of renal outcomes weave a somewhat optimistic pattern, with indications that GLP-1 agonists may confer nephroprotective effects. Notably, reductions in albuminuria and stabilization of eGFR (estimated Glomerular Filtration Rate) have been observed, hinting at a protective embrace around renal function. The DECLARE-TIMI 58 trial underscored this, exhibiting reduced progression of renal disease with the use of dapagliflozin, a finding that illuminates possible kidney-related benefits upon long-term utilization.
Long-Term Safety and Tolerability:
Navigating through the realms of safety and tolerability, the journey encounters potential turbulence. The spectrum of gastrointestinal side effects, although often diminishing with time, may linger or be perpetually bothersome for some individuals. Furthermore, there is the nuanced conversation regarding the potential risk of gallbladder disease and pancreatitis, although data in these contexts tread on the grounds of inconsistency and inconclusiveness. Thus, the story here remains partially shrouded, necessitating further research to elucidate clearer patterns.
The Specter of Retinopathy:
A shadow that has fleetingly crossed the GLP-1 pathway is the potential risk of retinopathy. Certain data strands, such as those emerging from the SUSTAIN-6 trial, hinted at an initial increased risk, albeit amidst a cascade of limitations and subsequent data from other trials, not consistently mirroring this outcome. Thus, while the shadow lingers, it’s far from being a definitive dark spot on the GLP-1 agonist journey.
In encapsulating this exploration, it’s evident that the GLP-1 agonist pathway, when traversed for the long term, offers a largely optimistic journey but is not devoid of potential pitfalls and uncertainties. The ensuing sections will further explore these aspects, peeling back the layers of emerging research and patient narratives to further illuminate the long-term trajectory of GLP-1 agonists.
Chronic Usage: Unveiling Potential Risks and Concerns
While the tapestry of GLP-1 agonists is embellished with evident advantages, especially in the realms of weight and glycemic control, the obverse side also exhibits threads of concerns and potential risks, particularly emanating from chronic usage. Here, we delve into a meticulous examination of the cautious whispers and tangible risks associated with prolonged exposure to GLP-1 drugs, drawing from the wellspring of existing research and clinical data.
Pancreatic Safety:
At the core of the apprehensions surrounding GLP-1 agonists sits pancreatic safety. Historical echoes of concerns pertaining to pancreatic inflammation and the insinuation of an increased risk of pancreatitis have wafted through the scientific corridors. Studies and clinical trials have rendered a mixed bag of results; some discern a potential risk, while others find no significant association between the agonists and heightened pancreatitis risk. The EXAMINE trial, for instance, did not exhibit an increased risk, yet the narrative remains punctuated with cautionary tales, necessitating meticulous monitoring and further research.
Thyroid C-Cell Hyperplasia and Carcinoma:
The synthesis of potential risks and GLP-1 agonists perhaps casts its most shadowy silhouette upon the discussion of thyroid C-cell pathology. Rodent studies have historically unearthed a correlation between GLP-1 agonists and a surge in thyroid C-cell hyperplasia and tumors. Yet, the extrapolation of these findings to humans dawdles amidst inconsistency. Human studies and meta-analyses, such as those published in The Lancet Diabetes & Endocrinology, predominantly showcase no significant elevation in risk, providing somewhat of a reassurance, albeit within the confines of existing data.
Cardiovascular Concerns:
As we meander through the pathway of chronic use, the domain of cardiovascular safety, although often bathed in a positive light, also demands a thorough scrutiny. While certain cardiovascular benefits have been showcased, especially in patients with established cardiovascular disease, the long-term impact of GLP-1 agonists upon the entirety of the cardiovascular system warrants an ongoing exploration to affirm safety and understand the nuances of its influences across diverse patient populations.
Gastrointestinal Disturbances:
Persistent threads of gastrointestinal disturbances weave through the chronic usage narrative of GLP-1 agonists. Nausea, vomiting, and diarrhea, while often transient and reducing over time, may linger or escalate into bothersome issues for some individuals, potentially impacting adherence to the medication and overall quality of life.
Psychological and Behavioral Impacts:
Amidst the biological considerations, the psychological and behavioral impacts of chronic GLP-1 usage also require acknowledgment. Potential alterations in appetite, eating behaviors, and the psychological interplay of managing sustained weight loss over extended periods unfold as understudied areas, demanding further exploration to understand the mental and emotional terrains navigated by patients on GLP-1 agonists.
Hypoglycemia:
Within the spectra of concerns, the risk of hypoglycemia, particularly when GLP-1 agonists are utilized in conjunction with sulfonylureas or insulin, also necessitates consideration and meticulous management to ensure patient safety and optimize glycemic control effectively.
As we entwine the threads of potential risks and concerns amidst the undoubted benefits, the tapestry of GLP-1 agonists in chronic usage reveals a narrative of potent metabolic advantages, interwoven with areas necessitating further research, cautious optimization, and individualized patient management. The journey forward, armed with evolving research and a patient-centric approach, will undoubtedly continue to refine our understanding and management of GLP-1 agonists in the tapestry of chronic care.
Longitudinal Studies: Translating Research into Understanding
In an endeavor to demystify the long-term effects of GLP-1 receptor agonists, numerous longitudinal studies have thrust their investigative lenses into the future, keenly observing the unfolding narrative of sustained GLP-1 drug usage. Let us traverse through the hallways of these studies, examining the tapestry of their findings, noting the nuances of their limitations, and ultimately, seeking to translate this woven narrative of research into tangible understanding and clinical application.
The LEADER Trial:
One monumental waypoint in our journey through longitudinal studies is the LEADER trial, which positioned liraglutide into the investigative spotlight, focusing upon cardiovascular outcomes over a median follow-up period of 3.8 years. Demonstrating a 13% reduction in the risk of cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke, this study burgeoned as a beacon of promise within the cardiovascular realm. Yet, the complexity of translating these findings into generalized practice lingered amidst questions regarding external validity and applicability across varied patient demographics and real-world settings.
The SUSTAIN-6 Study:
On the heels of the LEADER trial, the SUSTAIN-6 study weaved its narrative with semaglutide as the protagonist, exploring cardiovascular safety over a period of 2.1 years. Echoing the promising cardiovascular reverberations of its predecessor, it showcased a 26% reduction in the primary composite outcome, interspersed, however, with an increased risk of retinopathy complications, thereby stringing a note of caution into the melody of optimism.
The EXSCEL Trial:
With exenatide extended-release at its core, the EXSCEL trial did not narrate a statistically significant reduction in major adverse cardiovascular events but did harmonize with the previous trials in validating cardiovascular safety. With a slightly divergent outcome, it underscored the importance of individualizing therapeutic choices and acknowledging the multifaceted natures of various GLP-1 receptor agonists.
ELIXA Trial with Lixisenatide:
The ELIXA trial, although it did not manifest a significant reduction in cardiovascular events, provided a reassuring nod towards the cardiovascular safety of lixisenatide over a median 25-month period. This study emphasized that while GLP-1 receptor agonists collectively exhibit a relatively favorable safety profile, the minutiae of their effects may weave distinct tales.
Limitations and The Path Forward:
While these studies illuminate the path with insights, the shadows cast by limitations such as varying follow-up durations, differing patient populations, and diverse study designs also walk alongside us. Furthermore, while cardiovascular safety and benefits have predominantly steered the focus, the exploration of other long-term effects and comprehensive risk-benefit analyses across diverse patient populations remains paramount.
The synthesis of knowledge derived from these longitudinal studies embroiders a richer, albeit evolving, understanding of GLP-1 receptor agonists in long-term usage. As we stand at the confluence of known findings and unexplored territories, the continual flow of research, longitudinal observations, and nuanced understanding of individual and collective patient experiences will steer the vessel of GLP-1 drug application towards optimized, personalized, and safe utilization in chronic care management.
FAQs Surrounding Prolonged Use of GLP-1 Agonists
As healthcare providers, patients, and caregivers explore the potentialities and concerns enveloping the prolonged use of GLP-1 agonists, an assortment of queries burgeons, seeking clarity amidst the intricate web of scientific and clinical narratives. Here, we shall endeavor to shed light upon some of these prevalent inquiries.
1. What are the potential cardiovascular impacts of long-term GLP-1 drug usage?
Several longitudinal studies have probed into the cardiovascular consequences of sustained GLP-1 drug use, yielding promising results. For instance, the LEADER trial spotlighted liraglutide, illustrating a noteworthy reduction in cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke over several years. The SUSTAIN-6 study, emphasizing semaglutide, also unfurled a reduction in primary composite cardiovascular outcomes, albeit accompanied by a nuanced risk of retinopathy. Collectively, while these findings have galvanized optimism regarding the cardiovascular safety and potential benefits of GLP-1 drugs, it remains imperative to tailor these insights to individual patient contexts, recognizing the diverse cardiovascular impacts that may arise across varied demographic and clinical spectra.
2. How might prolonged use of GLP-1 drugs influence kidney function?
The tapestry of GLP-1 drugs and renal function is woven with threads of both potential benefits and considerations. Some studies suggest that GLP-1 agonists may confer nephroprotective effects, potentially via mechanisms such as reducing intraglomerular pressure, attenuating inflammation, and mitigating oxidative stress. For instance, the AWARD-7 trial, comparing dulaglutide with insulin glargine, portrayed a favourable impact upon albuminuria and eGFR (estimated glomerular filtration rate) decline. Conversely, it remains pivotal to tread with caution and vigilant monitoring in contexts such as pre-existing chronic kidney disease, wherein the nuanced interplay of GLP-1 drugs with renal function necessitates careful navigation. Thus, the journey of GLP-1 drugs and kidney function beckons a harmonization of potential renal benefits with circumspect application in specific patient contexts.
Patient Narratives
The tapestry of patient experiences with extended GLP-1 therapy unravels threads of varied shades – some reflecting empowerment and improved quality of life, while others revealing struggles and challenges. Here, we meander through real-world narratives, providing a glimpse into the lives of those navigating the terrain of sustained GLP-1 therapy, offering insights that move beyond statistics and clinical outcomes, weaving into the very fabric of lived experiences.
Anna: A Journey of Empowerment
Anna's dance with diabetes has always been a tenuous one, veering through moments of harmony and bouts of discord. With the initiation of liraglutide, a GLP-1 agonist, her narrative unfolded not just in the predictable metrics of HbA1c, but in newfound empowerment. The sustained weight loss, coupled with stabilized glycemic levels, became the undercurrent to a life of enhanced vitality and diminished fear of hypoglycemic episodes. Yet, Anna’s story does whisper tales of mild gastrointestinal discomfort, a reminder that even triumphant stories bear moments of discomfort and adjustment.
James: A Tapestry of Nuances
James embraced the GLP-1 pathway with a spirit of cautious optimism. Semaglutide became his companion in the journey, and his early experiences were a mosaic of profound weight loss and recalibrated metabolic control. However, as months stretched into years, James encountered a serendipitous challenge - unanticipated weight regain, despite adherence to his therapeutic regimen. His story, rich with complexity, heralds the necessity to explore beyond the initial triumph of GLP-1 therapy, examining the sustained efficacy and potential metabolic adaptations that may emerge in prolonged use.
Emily: Navigating the Ebbs and Flows
Emily’s voyage with dulaglutide was permeated with ambivalence. While the therapeutic benefits were palpable in metrics, the shadows of persistent nausea and occasional vomiting ebbed away at her quality of life. Emily’s narrative exemplifies the often uncharted territories of side effects, where the pharmacological benefits sometimes duel with the physiological and emotional costs of adverse effects, sketching a landscape where patients like Emily seek a balance between metabolic health and daily wellbeing.
The myriad of patient stories etch a reminder into the chronicles of GLP-1 therapy: while the clinical metrics and trial outcomes offer a foundation, the edifice of patient care is crafted from individual narratives, nuanced, varied, and profoundly personal. Herein lies the essence of navigating the path of GLP-1 drugs, where the convergence of clinical wisdom, research, and deeply personal patient stories forge the pathway to informed, compassionate, and individualized care.
Conclusion: Reflecting on the Journey and Gazing into the Future
Reflecting on the journey through the nuanced terrains of GLP-1 therapeutics unfurls a rich tapestry of insights, learnings, and forward-looking contemplations. The vibrant threads of clinical, ethical, and economic considerations weave a narrative that is both profound and pivotal in understanding the intricate dynamics of long-term GLP-1 drug prescriptions and applications, especially within the context of the UK’s healthcare landscape.
The complexity and multifaceted nature of GLP-1 drug applications have invited healthcare professionals, researchers, and ethicists alike into a sphere of perpetual exploration, learning, and adaption. Each revelation, be it in the potential expansion into neurological applications or the delicate balance of ethical and economic considerations in prescribing, invites a renewed perception and approach towards these therapeutic agents.
“The odyssey through GLP-1 therapeutics is far from linear, with each data point, patient interaction, and clinical experience enriching our collective understanding and approach towards this remarkable class of drugs,” muses Dr. Anaya Gupta, a diabetologist based in Edinburgh. Her reflective insights draw attention to the pivotal role of continuous learning, adaptation, and patient-centred focus in the evolving narrative of GLP-1 therapeutics.
Summarising Key Insights and Melding Knowledge
Summarising key insights from our exploration into GLP-1 drugs propels us into a sea of retrospection, where the ebbing waves of clinical efficacy, emerging applications, and moral and financial considerations converge into a cascade of holistic understanding. From their stalwart position in metabolic management to their burgeoning potential in arenas like neurology and cardiovascular health, GLP-1 receptor agonists have, undoubtedly, unfolded a myriad of therapeutic possibilities and dialogues.
The myriad of perspectives, from the bench of the researcher to the clinic of the healthcare professional, meld into a cohesive, albeit complex, picture. The intertwining narratives of potent glycemic management, emerging applications, ethical dilemmas, and economic considerations shape a knowledge scaffold that is, at once, sturdy in its data-backed insights and flexible in its adaptability to new findings and perspectives.
The reconciliation of knowledge acquired through diverse lenses, such as the detailed mechanics of GLP-1 action, the personable experiences of healthcare professionals, and the sobering realities of economic and accessibility disparities, fortifies our collective approach and understanding towards these therapeutic agents. As researchers and clinicians continue to navigate through the intricate channels of GLP-1 therapeutics, the melding of clinical, ethical, economic, and personal narratives will continue to shape the journey ahead.
Projecting Future Developments and Studies
Projecting future developments in the world of GLP-1 drugs invites a gaze into a horizon that is both exciting and veiled with uncertainties. The ever-evolving landscape of medical research and clinical applications promises a future where the applications, considerations, and experiences with GLP-1 therapeutics will continue to mature, expand, and possibly challenge our present understandings.
With research pipelines teeming with investigations into novel applications, such as GLP-1’s role in weight management, neurodegenerative conditions, and cardiovascular health, the forthcoming chapters in the GLP-1 narrative are poised to be vibrant, insightful, and paradigm-challenging. Dr. Michaela Thompson, a researcher in pharmacology, postulates, “The frontier of GLP-1 research and application is rich with potential, where each study, trial, and clinical experience seeds the soil for future explorations, applications, and perhaps, revolutions in various therapeutic domains.”
For those looking to learn more about weight loss medications, you can buy Wegovy online.
























 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews