Spirometry: Purpose, Procedure, Risks & Results
Related products
Definition of Spirometry
Spirometry is a noninvasive pulmonary function test used to measure the amount and speed of air that can be inhaled and exhaled by the lungs. This test provides essential information about lung function, helping healthcare providers diagnose, monitor, and manage various respiratory conditions.
Importance of spirometry in lung function assessment
Spirometry is a crucial diagnostic tool in assessing lung function because it allows doctors to quantitatively evaluate the performance of the lungs. The test results can help identify lung diseases, evaluate the severity of existing conditions, and monitor the effectiveness of treatments. According to Dr. James T. Good, a pulmonologist at National Jewish Health, "spirometry is an essential component of a comprehensive evaluation of patients with respiratory symptoms" (Good, 2016).
Purpose of Spirometry
Diagnosing respiratory conditions
Spirometry is instrumental in diagnosing various respiratory conditions, including asthma, chronic obstructive pulmonary disease (COPD), and other lung diseases. Dr. John E. Heffner, a pulmonologist and former president of the American Thoracic Society, states that "spirometry can detect airflow obstruction before patients become aware of their symptoms, enabling early interventions to prevent disease progression" (Heffner, 2014). For more information on diagnosing asthma click here.
Asthma
Asthma is a chronic inflammatory lung disease characterized by episodes of reversible airway obstruction, which can cause wheezing, chest tightness, shortness of breath, and coughing. Spirometry helps doctors confirm a suspected asthma diagnosis by measuring airflow limitations and reversibility after administering a bronchodilator (a medication that relaxes the muscles around the airways).
Chronic obstructive pulmonary disease (COPD)
COPD is a group of progressive lung diseases, including emphysema and chronic bronchitis, which cause airflow obstruction and difficulty breathing. Spirometry plays a vital role in diagnosing COPD by measuring the degree of airflow limitation and helping doctors differentiate COPD from other respiratory conditions, such as asthma.
Other lung diseases
In addition to asthma and COPD, spirometry is used to diagnose other lung diseases, such as interstitial lung diseases, bronchiectasis, and sarcoidosis. The test results can provide valuable information about the type and severity of the lung disease and help guide treatment decisions.
Evaluating lung function before surgery
Spirometry is often performed before lung surgery or other high-risk procedures to assess a patient's lung function and determine the potential risks and benefits of surgery. Dr. Charles Irvin, a pulmonologist at the University of Vermont Medical Center, emphasizes that "assessing lung function preoperatively helps surgeons and anesthesiologists develop a personalized plan to minimize complications during and after surgery" (Irvin, 2018).
Monitoring treatment effectiveness
Regular spirometry testing can help doctors monitor the effectiveness of treatments for respiratory conditions and make necessary adjustments to optimize patient outcomes. According to Dr. Michael Alberts, a pulmonologist and former president of the American College of Chest Physicians, "ongoing spirometry monitoring allows healthcare providers to track a patient's lung function over time and ensure that treatments are working as intended" (Alberts, 2015).
Identifying occupational lung hazards
Spirometry is a valuable tool for identifying workers at risk of developing occupational lung diseases due to exposure to harmful substances in the workplace, such as dust, chemicals, or fumes. Dr. Paul Blanc, a specialist in occupational and environmental medicine at the University of California, San Francisco, explains that "spirometry can detect early signs of lung damage from workplace exposures, allowing for timely interventions to prevent further harm" (Blanc, 2017).

III. Spirometry Procedure
A. Preparation for the test
- Patient instructions
Before undergoing a spirometry test, patients should follow specific instructions to ensure accurate results. These instructions may include:
- Avoiding heavy meals and smoking for at least 4 hours before the test
- Wearing loose, comfortable clothing that does not restrict breathing
- Refraining from vigorous exercise or activities for at least 30 minutes before the test
Patients should also inform their healthcare provider about any pre-existing medical conditions, recent surgeries, or current medications, as some factors may impact the test results or require additional precautions.
- Medication restrictions
Some medications can affect spirometry results, so doctors may ask patients to temporarily stop or adjust the dosage of certain medications before the test. These may include bronchodilators, inhaled corticosteroids, or long-acting beta-agonists. Patients should consult with their healthcare provider for specific instructions regarding medication restrictions.
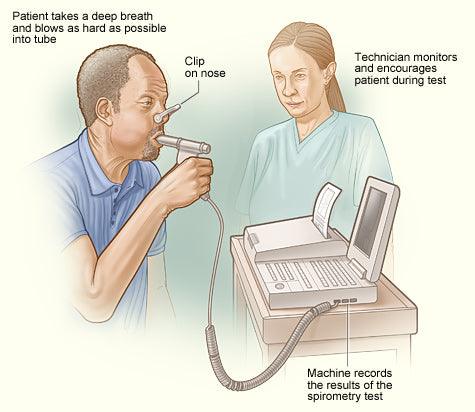
B. Description of the spirometry equipment
The primary equipment used in a spirometry test is a spirometer, which is a device designed to measure lung function parameters. Spirometers typically consist of a mouthpiece connected to a tube that is attached to a recording device. The recording device can be a computer or a handheld unit that displays and records the patient's lung function measurements.
C. Step-by-step process
- Positioning and sealing the mouthpiece
During the spirometry test, patients will be seated in a comfortable, upright position. They will be instructed to place the mouthpiece of the spirometer between their lips, creating a tight seal to prevent air leakage. A nose clip may be used to ensure that all exhaled air passes through the mouthpiece.
- Breathing instructions
Patients will receive specific instructions on how to breathe during the test. Initially, they will be asked to take a deep breath in, filling their lungs completely. Following this, they will be instructed to exhale as forcefully and quickly as possible into the mouthpiece.
- Performing the test
The spirometry test typically involves several attempts to ensure accurate and consistent results. Patients may need to repeat the process at least three times or more, depending on the healthcare provider's recommendations. After each attempt, the healthcare provider will review the results and provide feedback to help the patient improve their technique if needed.
D. Duration of the procedure
The entire spirometry test, including preparation and multiple attempts, typically takes around 15 to 30 minutes to complete. However, the duration may vary depending on individual circumstances and the healthcare provider's recommendations. Patients should plan for some additional time before and after the test for check-in, consultation, and follow-up.
IV. Risks and Precautions
A. Potential risks
Although spirometry is generally considered a safe procedure, it is essential to be aware of potential risks associated with the test. Some of these risks include:
- Shortness of breath
It is not uncommon for patients to experience temporary shortness of breath during or immediately following the test due to the forceful exhalation required. Dr. Michael G. Levitzky, Professor of Physiology and Anesthesiology at Louisiana State University, explains that the feeling of shortness of breath is usually mild and resolves quickly, but patients should inform their healthcare provider if the sensation persists or becomes severe (Levitzky, 2013).
- Dizziness
The forceful breathing technique used during the spirometry test may cause some patients to feel lightheaded or dizzy. Dr. Susan Murin, a pulmonologist at the UC Davis Medical Center, advises patients to rest between test attempts to minimize this risk and to inform their healthcare provider if dizziness becomes an issue (Murin, 2016).
- Chest pain
In rare cases, patients may experience chest pain or discomfort during the spirometry test. Dr. Richard Irwin, former chair of the American College of Chest Physicians' Guidelines Oversight Committee, emphasizes that patients should inform their healthcare provider immediately if they experience chest pain, as this could indicate an underlying issue that requires further evaluation (Irwin, 2007).
B. Contraindications
Spirometry may not be suitable for all individuals. Some contraindications include:
- Recent surgery
Patients who have recently undergone chest, abdominal, or eye surgery may be advised to postpone spirometry testing, as forceful exhalation could potentially cause complications. Dr. Peter J. Barnes, a renowned respiratory medicine expert at the National Heart and Lung Institute, recommends that healthcare providers carefully assess each patient's surgical history before administering spirometry (Barnes, 2014).
- Certain medical conditions
People with specific medical conditions, such as uncontrolled high blood pressure, heart disease, or aneurysms, may be advised against undergoing spirometry testing. Dr. Robert A. Wise, a pulmonologist at Johns Hopkins University, emphasizes the importance of carefully evaluating each patient's medical history to determine if the test is appropriate for them (Wise, 2017).
C. Safety measures and precautions
To minimize risks and ensure patient safety during spirometry testing, healthcare providers will:
- Carefully review the patient's medical history to identify any contraindications
- Provide clear instructions on breathing techniques and offer guidance during the test
- Monitor the patient's condition throughout the procedure and address any concerns or issues promptly
V. Interpreting Spirometry Results
A. Key measurements
Spirometry provides several key measurements to assess lung function, including:
- Forced vital capacity (FVC)
FVC represents the total volume of air that can be forcibly exhaled after taking a deep breath in. It is an important measurement for evaluating lung capacity and detecting restrictive lung diseases. Dr. Sanjay Sethi, Chief of Pulmonary, Critical Care, and Sleep Medicine at the University at Buffalo, highlights the significance of FVC in diagnosing conditions such as pulmonary fibrosis and other interstitial lung diseases (Sethi, 2018).
- Forced expiratory volume in 1 second (FEV1)
FEV1 measures the volume of air exhaled during the first second of the FVC maneuver. This parameter is crucial for identifying obstructive lung diseases, such as asthma and COPD. Dr. Kevin K. Brown, a pulmonologist at National Jewish Health, explains that a decreased FEV1 can indicate
the presence of airway obstruction, which is a common feature of these conditions (Brown, 2019).
- FEV1/FVC ratio
The FEV1/FVC ratio is calculated by dividing the FEV1 by the FVC. This ratio is used to determine the type of lung disease, whether it is obstructive or restrictive. Dr. Fernando J. Martinez, Chief of the Division of Pulmonary and Critical Care Medicine at Weill Cornell Medicine, states that a reduced FEV1/FVC ratio is indicative of an obstructive lung disease, while a normal or increased ratio with a reduced FVC suggests a restrictive pattern (Martinez, 2015).
B. Normal values and variations
Spirometry results are often compared to "normal" or "predicted" values based on the patient's age, height, gender, and ethnicity. These predicted values are derived from population studies and serve as a reference for assessing an individual's lung function. However, Dr. Elizabeth A. Regan, a pulmonologist at the National Jewish Health, cautions that normal values may vary between individuals, and healthcare providers must consider each patient's unique circumstances when interpreting spirometry results (Regan, 2020).
C. Indications of respiratory conditions
Spirometry results can provide valuable information about the presence and severity of various respiratory conditions. For example, a reduced FEV1/FVC ratio with a decreased FEV1 may suggest the presence of an obstructive lung disease, such as asthma or COPD. Conversely, a normal or increased FEV1/FVC ratio with a reduced FVC may indicate a restrictive lung disease, such as pulmonary fibrosis. Dr. MeiLan K. Han, a pulmonologist at the University of Michigan, emphasizes the importance of using spirometry results in conjunction with a thorough medical history and physical examination to make an accurate diagnosis (Han, 2011).
D. Factors affecting results
Several factors can affect the accuracy of spirometry results, including patient effort, technique, and the presence of acute respiratory infections. Dr. Don D. Sin, a respiratory medicine expert at the University of British Columbia, advises healthcare providers to be vigilant in identifying and addressing these factors to ensure accurate and reliable spirometry results (Sin, 2016).
VI. Frequently Asked Questions
A. How to prepare for a spirometry test?
To prepare for a spirometry test, patients should avoid heavy meals and smoking for at least 4 hours before the test. They should also wear loose, comfortable clothing that does not restrict breathing and refrain from vigorous exercise or activities for at least 30 minutes before the test. Additionally, patients should inform their healthcare provider about any pre-existing medical conditions, recent surgeries, or current medications, as some factors may impact the test results or require additional precautions.
B. What to expect during the test?
During the spirometry test, patients will be seated in a comfortable, upright position. They will be asked to place the mouthpiece of the spirometer between their lips, creating a tight seal to prevent air leakage. A nose clip may be used to ensure that all exhaled air passes through the mouthpiece. Patients will receive specific instructions on how to breathe during the test and will typically need to perform the test multiple times to ensure accurate results.
C. How long does the test take?
The entire spirometry test, including preparation and multiple attempts, usually takes around 15 to 30 minutes to complete. However, the duration may vary depending on individual circumstances and the healthcare provider's recommendations. Patients should plan for some additional time before and after the test for check-in, consultation, and follow-up.
D. How often should spirometry be performed?
The frequency of spirometry testing depends on the individual's medical condition and the healthcare provider's recommendations. For patients with chronic lung diseases, such as asthma or COPD, spirometry may be performed regularly to monitor disease progression and treatment effectiveness. For others, spirometry may be conducted on an as-needed basis to evaluate lung function in response to specific concerns or symptoms.
VII. Conclusion
A. Importance of spirometry in managing lung health
Spirometry plays a critical role in diagnosing, monitoring, and managing various respiratory conditions. By providing an objective assessment of lung function, spirometry enables healthcare providers to make informed decisions about appropriate treatment plans and monitor their effectiveness over time.
B. Role of healthcare providers in spirometry
Healthcare providers play a crucial role in ensuring the safe and accurate administration of spirometry tests. They are responsible for carefully reviewing each patient's medical history, providing clear instructions and guidance during the test, and interpreting the results to inform appropriate clinical decisions.
C. Encouraging patients to take control of their respiratory health
By understanding the importance of spirometry and how it can help detect and manage respiratory conditions, patients can take a more active role in managing their lung health. Regular spirometry testing, as recommended by healthcare providers, can help patients stay informed about their lung function and facilitate timely interventions to optimize their respiratory health.
Related Asthma Treatments
- Buy Asthma Inhalers & Treatment Online
- Buy Ventolin Accuhaler
- Buy Ventolin Evohaler
- Buy Salbutamol Inhaler
- Buy Clenil Modulite
- Buy Qvar Aerosol Inhaler
- Buy Salamol Inhaler
- Buy Able Spacer
- Buy Symbicort Turbohaler
- Buy Salamol Easi Breathe Inhaler
- Buy Sereflo
- Buy Child Aerochamber
- Buy Spiriva Respimat
- Buy Sirdupla
- Buy Duoresp
- Buy Qvar Inhaler
- Buy Pulmicort Turbohaler
- Buy Seretide Accuhaler
- Buy Montelukast
- Buy Serevent Evohaler
- Buy Kelhale Inhaler
- Buy Fostair Inhaler
- Buy Flutiform Inhaler
- Buy Flixotide Accuhaler
- Buy Bricanyl Inhaler
- Buy Atrovent Inhaler
- Buy Alvesco Inhaler
- Buy Airomir Inhaler
Related Asthma Articles and Information
- Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments
- Living with Asthma
- Allergic Asthma
- Brittle Asthma
- Asthma Diagnosis and Testing
- Eosinophilic Asthma Guide
- BTS Asthma Guidelines
- Allergies & Asthma
- Reactive Airway Disease
- Do I have Asthma? (Quiz)
- Is Asthma a disability?
- NICE Guidelines on Asthma
- Asthma Control
- Difference Between Asthma and COPD
- Vocal Cord Dysfunction
- Asthma Attacks
- Exercise-Induced Asthma
- What does an Inhaler do to someone without an Inhaler?
- Can I claim PIP for Asthma?
- How to use an asthma inhaler
- How to use a peak flow meter
- Is Salbutamol a Steroid?
- Montelukast, Side Effects and Uses
- AERD












 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews