When to worry about pancreatitis?
Identify the signs of chronic or severe acute pancreatitis before it is too late.

The term 'itis' denotes inflammation. So pancreatitis means the inflammation of the pancreas. The inflammation on the skin can be easily identified due to the pain, redness, swelling etc. But, identifying inflammation in the internal organs is cumbersome. A combination of clinical signs and laboratory tests can help you in the job.
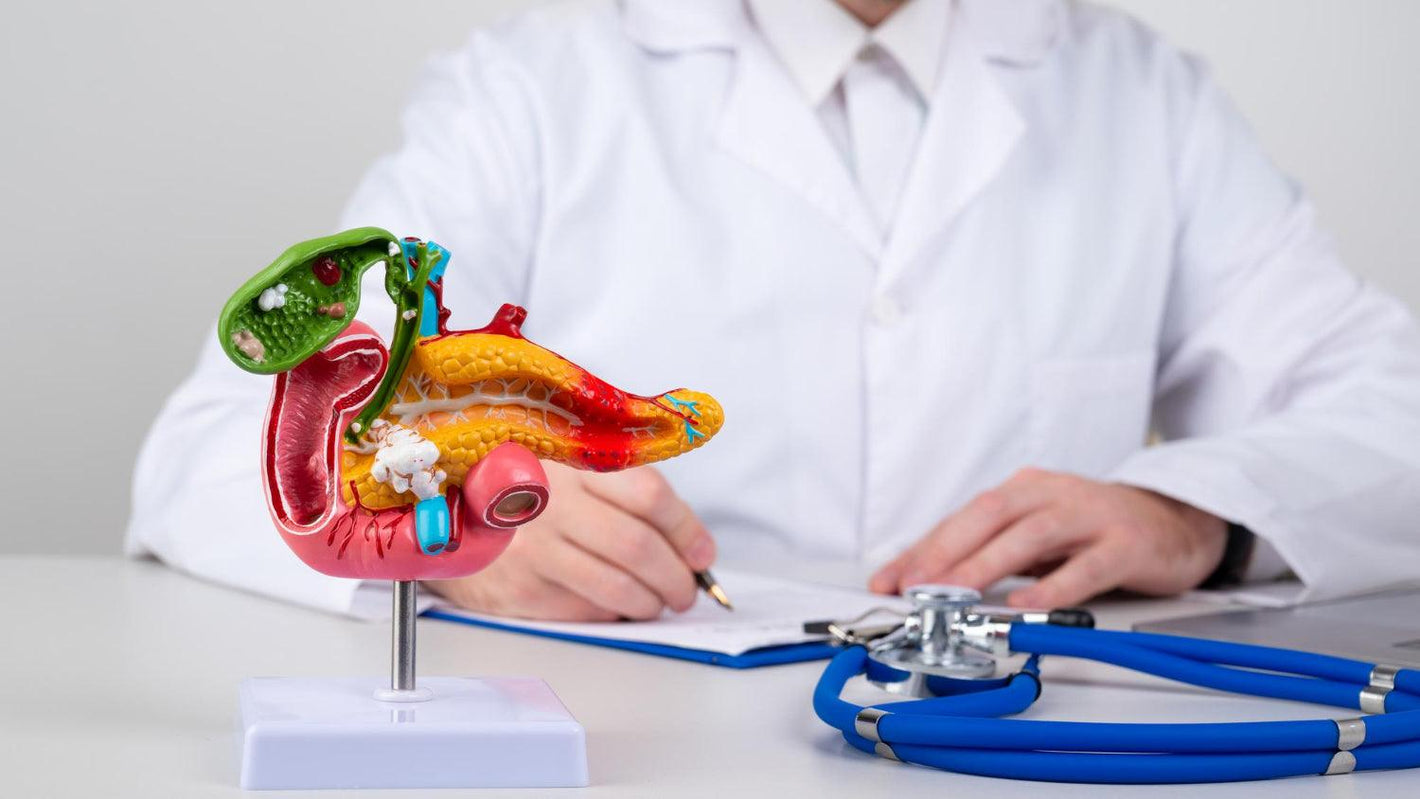
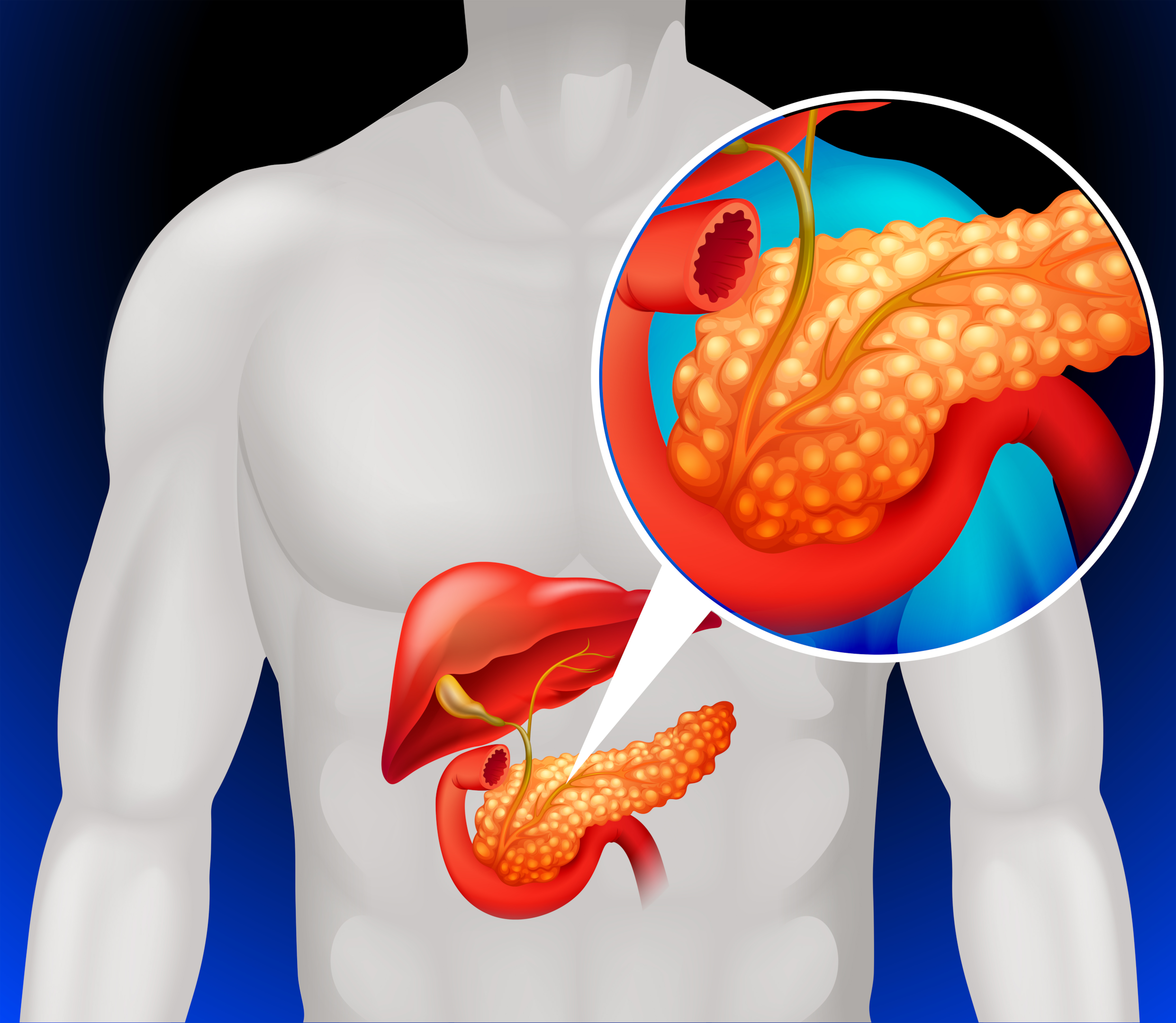
So, how can you know if your pancreas is inflamed? Let's first have a brief introduction to the pancreas.
Have you any know-how about the pancreas? It is a flat, long organ that lies behind your stomach in the abdomen. It is an organ and a gland as it is a source of enzymes, e.g., lipase, protease etc., that help digestion and hormones that regulate the blood sugar levels.
It is a source of two essential hormones, insulin and glucagon, which help to regulate your blood glucose. So, a healthy and functional pancreas is necessary for you.
There are a lot of situations that can cause your pancreas to get inflamed. What are the causes of pancreatitis? How to know if you have pancreatitis, and when should you worry about the health of the pancreas? Stay on the lines for answers.
Several causes and risk factors can trigger acute pancreatitis. The same factors can contribute to the development of chronic pancreatitis. Severe pancreatitis is a result of the accumulation of more causes and risk factors, e.g.,
The pancreas produces enzymes which help in the digestion of food. These include;
Lipase, which digests fats
Protease (trypsin), which digests proteins
Amylase digests carbohydrates.
The internal organs are also made of proteins. So, why not the protease digests the organs itself? These enzymes are produced in an inactive form and are activated as they enter the intestines. However, if due, for any reason, these enzymes are activated inside your pancreas, they will cause irritation and inflammation, causing acute pancreatitis.
Sometimes, if the causative factor (s) is not removed, this acute pancreatitis lingers to become chronic. The healing of wounds will leave behind a scar with much less functional abilities. It decreases the functionality of the pancreas.
Besides this, there are several risk factors of developing acute pancreatitis e.g.,
Obesity
Abdominal injury
Excessive consumption of fatty or spicy foods
Cystic fibrosis (in which the small tubes that are transporting enzymes out of the pancreas are blocked with the mucus).
Internal infections
Pancreatic cancer
Abdominal surgeries
Hypercalcemia (higher level of calcium in the blood)
Use of some drugs, e.g., cisplatin, antibiotics, enalapril, acetaminophen etc.
Gallstones (stones in the gallbladder block the bile duct, and the pancreatic enzymes can't leave the pancreas and are forced back).
Use of alcohol (heavy drinking is the most important single cause of pancreatitis and is responsible for 70-80% of cases).
Higher levels of triglycerides
Some medical procedures, e.g., cholangiopancreatography (the surgical removal of gall stones, etc.
However, many times, people develop pancreatitis due to unknown causes, called idiopathic pancreatitis.
Given the essential functions it has in your body, you need to check your pancreas's health regularly. A higher blood level of pancreatic lipase is often the first sign of compromised pancreas health. Our Lipase Blood Test does this job for you. All it needs is a single drop of blood. Click here to get your kit.
Can you leave an inflamed pancreas as such? No. Chronic inflammation of the pancreas can cause severe complications that can endanger your life. These include;
Pancreatic cancer is a highly dangerous, malignant tumour with a high fatality rate. It has a moderately high prevalence in the UK, as according to CancerresearchUK.org, more than 10,000 new cases of pancreatic cancer are reported each year in the UK, with thousands of deaths annually.
Among other risk factors, chronic pancreatitis, which lingers on for months or years, is a significant risk factor. Undiagnosed or untreated pancreatitis can lead to pancreatic cancer. There is also a risk that an inflamed pancreas can be misdiagnosed with cancer.

A study published in the Annals of Oncology in 2012 found that a moderate association exists between pancreatic cancer and pancreatitis, and a small proportion of cases of pancreatic cancer can be avoided by timely treatment of pancreatitis.
Chronic or even mild acute pancreatitis can damage the pancreas's cells that produce insulin and glucagon, leading to diabetes. Consequently, the body will not be able to regulate its glucose levels.
Pancreatitis as a risk factor for diabetes was noted by a 2016 study published in Medicine. It was found that 564 patients, in a total of 2011, developed diabetes mellitus in the follow-up period of 22 years.
The acute form of pancreatitis can lead to kidney failure. You may need emergency dialysis. Renal failure in patients with acute pancreatitis adds to the chances of death. For example, a retrospective study conducted in Taiwan noted that patients with acute pancreatitis also have a higher risk (15.05%) of acute renal failure, and those with both of these issues have much higher mortality rates.
Recall the functions of the pancreas. Both chronic and acute pancreatitis can result in damage to the cells which produce digestive enzymes. So, your body will not be able to process the food and thus will go deficient in the essential nutrients. The results will be a deficiency of essential nutrients (malnutrition) with diarrhoea. You may be eating enough food, but it is not available to your body.

Other associated symptoms are severe abdominal pain, vomiting, diarrhoea, bloated abdomen and fever.
The chemical changes associated with acute pancreatitis can disturb the functions of the lungs, causing severe breathing issues. The body will not get enough oxygen to keep functioning (hypoxia). One of the complications of acute pancreatitis is an acute lung injury.
Besides the lungs, the complicated cases of chronic and acute pancreatitis can also involve the other organs in the chest cavity, e.g., vascular structures, pleura, mediastinum etc., adding further stress to the respiration and mortality.
The inflammation results in the production of fluids. These fluids and the debris can accumulate in the pancreas in the form of pockets (called cysts). Sometimes, a cyst can rupture, leading to severe infection and internal bleeding, a life-threatening situation.
In most cases, these cysts are the pseudocysts lined by fibrous tissues, inflammatory tissues and scar tissues. These cysts are harmless (benign) and cause very few symptoms. However, some of these cysts can be pre-cancerous and lead to pancreatic cancer. The doctor will determine the type of cyst and provide treatment accordingly.
An infection causes favourable conditions for the development of another disease. If left untreated, this vicious cycle of infections can cause permanent damage to your pancreas, and it will be needed to be removed.
Sometimes during severe acute pancreatitis, the pancreas can lose its blood supply, leading to the death of some of its issues (necrosis). The necrosed part becomes infected, which can spread to multiple organs through blood (sepsis), causing multiple organ failures. It is a fatal situation. However, timely assistance at the earliest symptoms of acute pancreatitis can improve the chances of survival.
Both acute and chronic pancreatitis leave many signs that can help diagnose. However, clinicians may use more diagnostic approaches for this purpose. The common symptoms are;
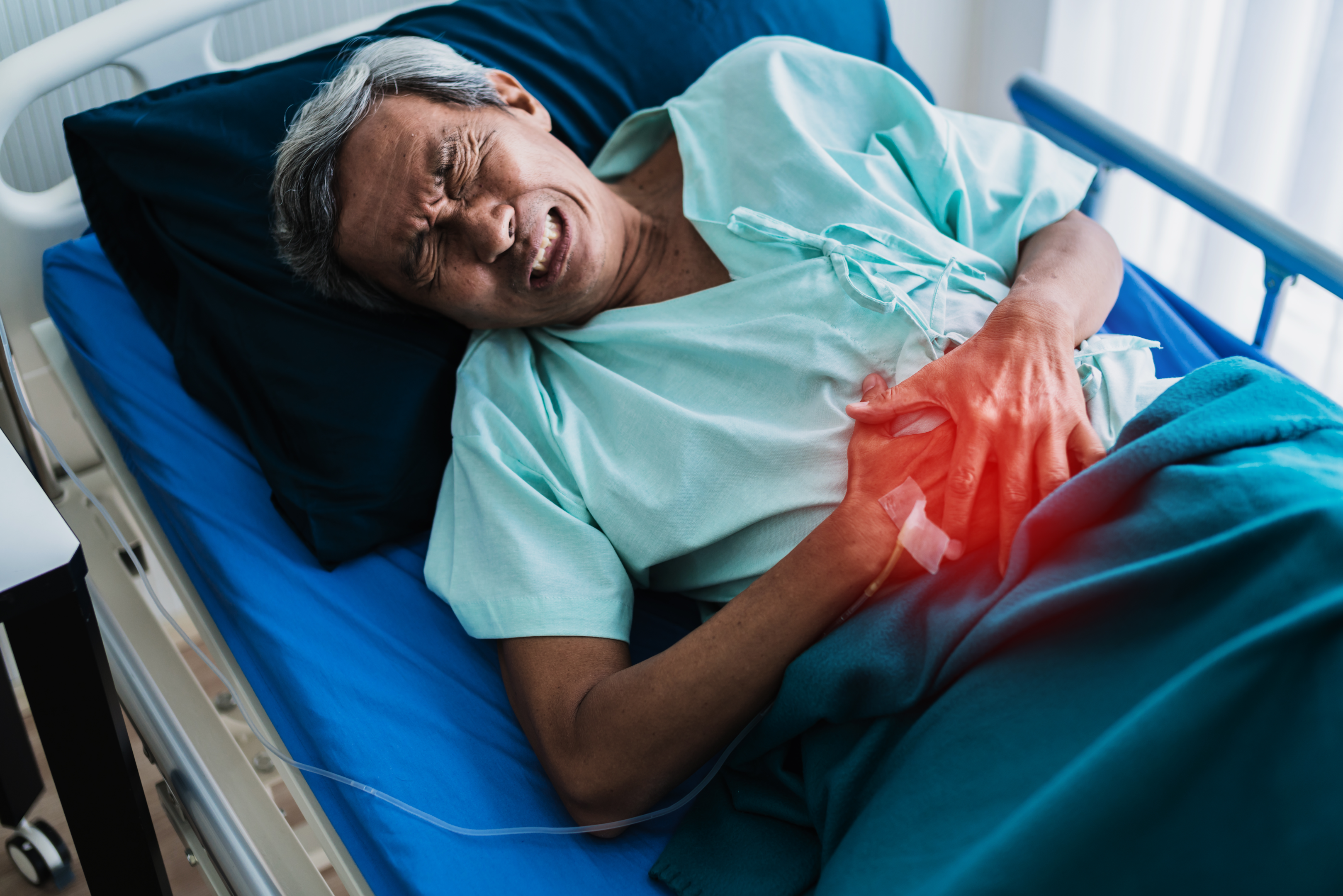
People with acute pancreatitis experience the following symptoms;
Tenderness and swelling in the belly and pain during touching
Fever
Increased heart rate and pulse
Vomiting and nausea
Pain in the upper abdomen, which stretches towards your back
Some cases of chronic pancreatitis can be asymptomatic. Symptoms that do appear are similar to the above symptoms. However, some additional signs are;
A constant, disabling and severe pain in your belly with frequent painless periods, the pain also felt relieved when leaning forward.
Chronic diarrhoea leading to weight loss
Foul-smelling, greasy and difficult-to-expel stools
Stomach upsets with nausea and vomiting
Increased risk of chest or urinary infection
Diarrhoea can, however, be due to a variety of other causes. Regardless of the reasons, it can do hell to your overall health within a few days, and you need instant treatment. We have various treatment options available for you, which you can avail of by clicking here.
Both acute and chronic pancreatitis can be severe and life-threatening, and you need to consult a specialist as soon as the signs appear, and particularly, if they are persistent. Despite tremendous advances in the critical emergency care of acute pancreatitis in the last 2 decades, the death rate of acute pancreatitis remains high at 10% (National Pancreas Foundation).

Diagnosing acute and chronic pancreatitis is very important, and intensive and emergency care is required for people with signs of complications. The milder forms are easy to treat, provided a timely invention is made. But, acute and complicated pancreatitis often needs many days of hospitalisation and multiple surgical interventions.
Sometimes, the doctors may recommend the removal of the organ in cases where the organ has been damaged beyond any hope of repair.
It would help if you continued to monitor the signs of acute and chronic pancreatitis and go to the doctor as soon as the symptoms worsen and the signs of complications are too apparent. The appearance of the following signs needs immediate medical attention.
Agitation, confusion, and loss of consciousness
Foul-smelling and greasy faeces due to improper digestion of proteins, fats and carbohydrates
The appearance of symptoms of jaundice, e.g., yellowing of white portions of eyes and skin
Unexplained and persistent weight loss
Persistent weakness, fatigue and faintness
Fever
Increased heart rate
Nausea, vomiting and breathing issues
Abdominal pain, which is not responding to the painkillers
Also, seek medical assistance if you are worried about the treatment being used, have any questions about it, or are planning to use some over-the-counter or herbal medications. Also, take the help of a doctor to eliminate risk factors, e.g., smoking, alcoholism and eating a portion of healthy food.
The tentative diagnosis is made based on clinical signs and symptoms. However, the doctor takes the help of some other tests for a definitive diagnosis, e.g.,
Faecal analysis to determine the consistency of your stools, e.g., the presence of undigested fats.
MRI to detect the abnormalities in the pancreas, gall bladder and their ducts
Blood tests: the presence of higher levels of pancreatic enzymes, white blood cells or liver enzymes is often a sign of infection inside your body and can give the doctor a clue about your inner health.
Ultrasonography: an abdominal ultrasound will help to detect gallstones or an inflamed pancreas.
CT scan: working principle and objectives are similar to ultrasonography, but it provides more details about pancreatitis health.
Several treatment options are available for pancreatitis. The exact approach depends upon the type and severity of the situation. Cases of acute pancreatitis recover relatively more easily than chronic ones.
The most common method for acute, chronic and complicated cases is to hospitalise a person and use painkillers, antibiotics and intravenous fluid therapy. Any other complications are treated as they arise.
The doctors often recommend that patients fast or at least use a low-fat diet as soon as the symptoms of infection subside. The administration of intravenous fluids also accompanies it to maintain the hydration status.

In severe cases, where treatment is too complex or risky and very large gallstones are present, the doctor may ask you to undergo cholecystectomy, the surgical removal of the pancreas.
If you think you have the symptoms of acute or chronic pancreatitis and the cause is not established, contact us. Our health experts are specialised in the job and will help you to know the cause of symptoms. You may need an appointment with our health experts. Click here to proceed. The page also contains many of our products related to gut health, which you can purchase after consulting our professionals.
There is, however, a novel idea in medicine, which is to use your food as medicine, as many foods commonly used have medicinal value. Click here to read our informative article on the topic.
The pancreas is a longitudinal organ present near the stomach which helps in the regulation of glucose and the digestion of food. Its functions are essential for your life or at least your life's quality. Pancreatitis is the inflammation of the pancreas. It is an inflammation of inner organs and should never be ignored. The treatment and management plan is the job of your doctor.
However, you need to keep an eye on the signs and symptoms of acute and chronic pancreatitis and go to the doctor immediately as soon as any issue (s) is noted. Untreated pancreatitis can cause severe and life-threatening complications requiring immediate and intensive help. However, it is best to avoid pancreatitis through a healthy lifestyle, e.g., a healthy weight and avoiding alcohol and smoking.
Studies have shown that a healthy lifestyle can help you to avoid more than one-third of cases of gallstones which are often the cause of acute pancreatitis. At Welzo.com, our health professionals can guide you through pancreatitis and other health issues. Click here for online consultation.








Plus get the inside scoop on our latest content and updates in our monthly newsletter.