Nucleated Red Blood Cell Count: What Can This Mean?

Related products
Various components collaborate seamlessly to ensure the human body’s optimal functionality, with each structure playing a crucial role. One such integral participant in this complex system is the Nucleated Red Blood Cell (NRBC) which is an immature version of red blood cells primarily found within bone marrow: our body's dedicated factory for producing red blood cells. NRBCs are distinct owing to their nucleus - something matured or normal counterparts lack as it gets ejected at a time when an adolescent cell transforms into a fully grown non-nucleated specimen.
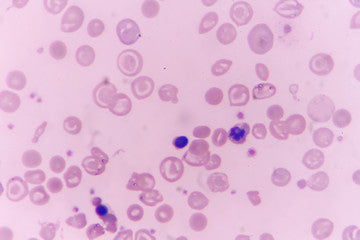
Examining and comprehending NRBC counts plays a critical part in clinical diagnostics and health assessment scenarios. An abnormal increment in these numbers often signifies grave medical anomalies usually linked with serious illnesses like cancerous conditions, infections, or cardiovascular diseases; wherein increased presence detected outside the confines of bone marrow i.e., peripheral circulation serves as a diagnostic indicator.
Background
Normal Erythropoiesis
Examining the origins of Nucleated Red Blood Cells gives insight into erythropoiesis - a process that generates new red blood cells. As an extraordinary and complex mechanism, erythropoiesis functions within the bone marrow under stringent hormonal regulation. During this routine operation, what begins as a hematopoietic stem cell morphs into a proerythroblast- a term coined by scientists.
As it continues through numerous developmental stages such as basophilic, polychromatic, and orthochromatic erythroblasts to finally become an NRBC or normoblast. A pivotal occurrence marks this terminal stage – nucleus expulsion leading to reticulocyte formation which is essentially immature but lacks its predecessor’s nucleus bringing it closer to functional maturity than before.
These fledgling reticulocytes leave their cradle place - the bone marrow for the bloodstream where they mature over two days into fully grown entities known commonly as mature Red Blood Cells or Erythrocytes tasked mainly with delivering oxygen throughout body tissues using haemoglobin an iron-rich protein lending RBCs iconic red colour.
Interestingly reticulocytes form only about one percent of the total circulating population count at any time ensuring balance between production destruction and thus enabling uninterrupted supply of requisite quantity indicating signs of a healthy functioning system.
Pathophysiology
Nucleated red blood cells typically remain confined within bone marrow – their appearance in peripheral blood often signifies a state of physiological disturbance or 'stress'. One primary trigger for such premature release is an intense systemic response to hypoxia.
Hypoxia indicates reduced levels of oxygen, necessitating immediate consideration and intervention from the body's physiology. Mature red blood cells (erythrocytes) under standard conditions efficiently manage oxygen supply across our bodies. However, when challenged with hypoxic stress due to situations like severe lung diseases or heart failure; it propels the erythropoiesis process into overdrive leading to increased immature stages including NRBCs populating the bloodstream.
On another note, excessive breakdown of erythrocytes affects haemoglobin abundance thereby prompting compensatory responses that increase production activity at all developmental stages hence contributing towards the influx of these entities.
Direct stress impacting bone marrow as seen in infiltrative diseases - cancers leukaemia disrupt harmony between different cell populations and thus might lead to elevated counts observed laboratory tests uncovering yet another facet of disease states warrant careful monitoring crucial better management of patient outcomes.
Why Will You Need An NRBC Test?

The need for an NRBC test comes into being when there are grounds to believe significant health problems exist. Such complications have the power to interfere with the routine procedure of red blood cell growth or erythropoiesis, resulting in the premature dispatch of immature cells including nucleated versions into the bloodstream.
Medical professionals might suggest such a screening based on manifestation symptoms indicating latent disorders - weakness fatigue caused by anaemia breathlessness indicative of systemic hypoxia resultant diseases like lung ailment heart failure recurrent infections unresponsive usual treatment methods implying sepsis.
Further clinical scenarios suggesting disruption within bone marrow–inexplicable weight reduction nocturnal perspiration joint discomfort overall swollen lymph nodes too necessitate comprehensive examination along with counting.
What Are The Clinical Scenarios Indicating NRBCs?
Hemolytic Anaemia
Abnormalities in red blood cell count are noticed within different clinical contexts. A prime example of such is Hemolytic anaemia - a situation where erythrocytes (red cells) undergo premature destruction, causing their numbers to dwindle in circulation. Such events prompt the bone marrow into overdrive, increasing production and sometimes leading to NRBCs appearing in the bloodstream.
Additionally, Hemolytic anaemia includes various subtypes like hereditary spherocytosis and sickle cell disease wherein deformed haemoglobin generates crescent-shaped RBCs that become fragile- as stated by National Health Services.
Severe Infections or Sepsis
Conditions such as severe infections or sepsis demand swift medical intervention. Sepsis is the body's systemic response to a grave infection, primarily bacterial in origin, inciting widespread inflammation throughout multiple organ systems.
In circumstances of sepsis, harmful endotoxins and pathogens infiltrate the bloodstream leading to substantial inflammatory reactions through the release of cytokines - proteins vital for cell communication during immune responses. These proinflammatory molecules are necessary for combating foreign intruders; however, their overabundant emission becomes counterproductive causing harm including damage to vascular walls eventually culminating in multi-organ dysfunction syndrome seen with systemic septic shock.
Under these intense pathogenic situations there is ramped-up erythropoiesis activity within bone marrow – a process by which red blood cells get formed bypassing standard maturation procedures one being nucleus discard before entering circulation Hence the observation of elevated counts often highlights amplified illness severity has been extent noted healthcare personnel treating patients diagnosed necessitating strict vigilance expedited therapeutic measures ensuring improved survival rates.
Hypoxic Conditions
Every single function of the human body depends on a steady oxygen supply, and this task is dutifully performed by erythrocytes - mature red blood cells. They transport life-sustaining gas from the lungs to all parts of our system.
However, certain situations such as lung diseases (chronic obstructive pulmonary disease or pneumonia) or heart conditions affecting circulation (blue baby syndrome), lead to inadequate delivery of necessary oxygen amounts across tissues subsequently causing Hypoxia.
When deprived of its vital fuel, tissues send out signals for immediate response triggering compensatory mechanisms within physiology which translate into an increased production rate in a process known as Erythropoiesis; where core bone marrow constructs new RBCs.
Erythropoietin- hormone primarily produced kidney responding hypoxic state acts as a stimulating factor speeding maturation various stages and eventually forming reticulocytes Though amidst high demand some of these semi-formed ones i.e., NRBCs make their way to peripheral circulation serving marker for condition's intensity.
Research strongly links elevated counts of patients experiencing respiratory distress implying it is a valuable assessment tool guiding treatment plans Hence unravelling how intricate biological processes adapt critical aspects like indispensable not only helps us comprehend underlying pathophysiology but assists in making efficient informed healthcare decisions optimising patient outcomes.
Bone Marrow Disorders
Disruptions within bone marrow originate from various disease states. One such case is Myelofibrosis, a severe disorder that interferes with standard blood cell formation by inducing scar tissue or fibrous creation inside vital organs. As a result, it interrupts the regular progression and development cycle of red blood cells resulting in premature release of immature variants like NRBCs into circulation.
Leukaemia provides another stark instance where harmful alterations occur in the cellular composition of bone marrow - effectively it's cancer affecting the body's tissues responsible for forming blood including the marrow itself Inevitably leads to excessive production of white cell precursors overshadowing the growth of other types of necessary balanced haematopoiesis unusual proliferation of inadvertently releases significant amounts NRBCs circulating bloodstream thereby complicating diagnostic profiles.
In both cases, higher counts serve as pivotal biomarkers aiding the detection and assessment severity of diseases with utmost precision whilst tracking responses towards therapeutic interventions facilitating personalised care enhancing survival rates ultimately improving the quality of life of those affected.
Other Conditions
Venturing into the realm of neonatal medicine, it's important to highlight that nucleated red blood cells bear great significance even at birth. One such condition demanding attention is asphyxia among newborn babies, a severe deficiency of oxygen supply to the body.
Birth complications like umbilical cord accidents or placental insufficiency result in this state known as perinatal hypoxia or neonatal asphyxia. In response to low levels of oxygen reaching the tissues - essentially creating a situation similar to systemic hypoxia experienced by adults - an acceleration happens on the erythropoiesis pathway within the foetal bone marrow.
As part and parcel of its protective mechanism striving for survival against these challenging circumstances; NRBC counts escalate entering the bloodstream aiming to compensate for reduced availability. Therefore, increased presence has been recognized as an early indicator reflecting severity degree exposure thus becoming a critical diagnostic tool for physicians assessing a baby’s health prognosis after suffering from distress during the delivery process.
How To Interpret NRBC Result

Normal Range of NRBCs
Typically, Nucleated Red Blood Cells (NRBCs) stay confined to the bone marrow and do not circulate in peripheral blood. Therefore, under normal physiological circumstances, there is an absence or a negligible number of these cells present – usually less than 1 per 100 white blood cells.
However; compensatory responses caused by increased demand for RBC production tilt this balance and result in elevated numbers detected during laboratory analysis.
Comparison with Other Diagnostic Markers
Besides solely depending on analysing amounts, it's pivotal to consider other key markers patient's complete cell profile portrayed Full Hemogram test Such as reticulocytes- precursors mature form representing newly released one's Bone Marrow Whereas White Cell Count indicates immunity system status often fluctuating response infections inflammatory conditions.
Therefore comprehensive evaluation involving all players grants a more accurate representation of underlying conditions aiding physicians decide the correct course of action in case management patients Hence importance multi-faceted approach considering diagnosis and prognosis ailments ensures a holistic view of patient health making interpretive science art itself fosters better outcomes therapeutics.
What is the procedure for an NRBC test?
The procedure to identify Nucleated Red Blood Cells (NRBCs) is relatively straightforward and forms part of routine blood test protocols, often performed under doctor's orders.
Initially, a healthcare professional collects a small sample of a patient's blood typically from the arm using a sterile technique. This specimen then undergoes processing in a clinical laboratory where it is evaluated for multiple parameters including complete cell counts both red and white cells haemoglobin levels among others.
Specifically assessing NRBC count involves microscopic examination of peripheral smear-thin spread on a glass slide stained to enhance the visibility of cellular components. Professional lab technicians or hematopathologists scan these smears scrutinising various entities and identifying any unusual presence like an abnormally high number of immature stage circulation.
More recent advancements have seen the introduction of automated counters that are capable of detecting and evaluating without the need for microscopy, greatly increasing efficiency and accuracy.
What happens next if my NRBC count is too high?
If the NRBC count is found to be high, it's an immediate cue for medical professionals to delve deeper into a patient’s health status. A heightened level of these immature cells in peripheral blood indicates that severe bodily stress has triggered bone marrow to increase production and release these cells earlier than normal.
It becomes important - not just merely identifying this abnormal rise but also investigating its cause as it often points toward hidden ailments including hemolytic anemias, hypoxic disorders like lung disease or heart failure, sepsis due to infections, even malignant conditions infiltrating Bone Marrow such as leukaemia.
Therefore; subsequent steps involve thorough clinical evaluation with detailed history taking physical examination accompanied by further diagnostic tests. These might encompass a Full Blood Count test, reticulocytes assessment, liver kidney function markers along inflammation indicators Depending on primary suspicion additional specific investigations are warranted – For instance, Imaging studies Chest X-rays, ultrasounds, and CT scans if respiratory or cardiovascular issues suspected Biopsies aspirates cases where malignancy being ruled out.
Moreover, treatment revolves around addressing underlying conditions leading to overproduction once identified and dealt with effectively leading to eventual normalisation levels providing relief from symptoms, and improving the quality of life of patients concerned Hence higher demands meticulous attention and close follow-up towards achieving successful healthcare outcomes.
Takeaway
Nucleated Red Blood Cells (NRBCs) are immature red blood cells that typically reside within the bone marrow. Their presence in peripheral circulation often indicates severe health disturbances triggering increased production from marrow. Such conditions include anemias where premature destruction of RBCs occurs, systemic hypoxia due to lung diseases or heart failure, infectious states like sepsis, and malignancies infiltrating the bone marrow.
A test counting these entities becomes a vital part of clinical assessment when symptoms suggest extensive disease burden or known history exists with relevant illnesses. It provides essential information regarding disease severity and prognosis aiding physicians towards effective management strategies aimed at patient's better health outcomes.
Frequently Asked Questions
Is nucleated RBC 0.01 normal?
The presence of NRBC at 0.01 does fall within acceptable ranges since a healthy individual typically has less than one Nucleated Red Blood Cell per hundred White Blood Cells.
What is the total nucleated cell count?
The term Total Nucleated Cell Count (TNCC) refers to the total count of all cells in a blood sample with nuclei, which includes white blood cells and nucleated red blood cells, among others.
What is the normal range of NRBC 100 WBC in newborns?
In newborns, attributable to physiological stress during childbirth and adaptation post-delivery, higher numbers of NRBC might be prevalent for short duration after birth, however an excess beyond up to five nRBC/100 WBC is generally considered abnormal requiring further investigation.
What are the advantages of nucleated red blood cells?
NRBCs hold their significance from a diagnostic perspective as they offer valuable insight into a patient's condition. An elevated level indicates serious systemic disease helping physicians assess the severity prognosis aiding them towards optimal management strategies.
What is a good NRBC level?
A good or desirable NRBC level under normal conditions would essentially be zero or negligible; it implies efficient erythropoiesis without any untoward 'stress' on the body triggering premature release of these immature entities into circulation.










 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews