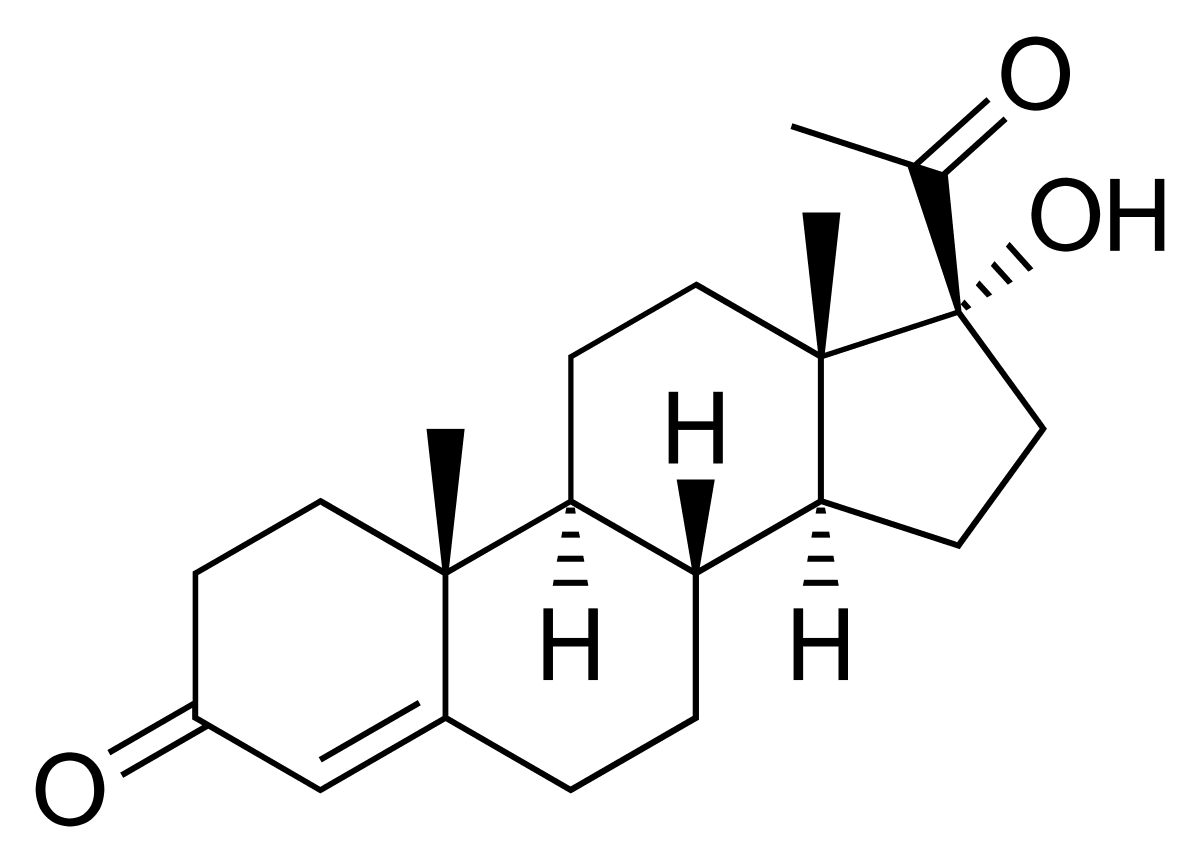
17-hydroxyprogesterone (17-OHP)

Related products
17-Hydroxyprogesterone (17-OH progesterone) is a crucial steroid hormone that plays a foundational role in the synthesis of glucocorticoids, androgens, and estrogens. It is primarily produced in the adrenal glands and gonads, acting as a key precursor in cortisol and aldosterone biosynthesis. Proper regulation of this hormone is vital, especially in early development and reproductive health. Elevated levels of 17-OH progesterone are most notably linked to Congenital Adrenal Hyperplasia (CAH), a potentially life-threatening genetic disorder. With modern diagnostic capabilities, early detection of hormonal irregularities has become more accessible. Patients can now utilise convenient at-home services such as the Welzo home blood test platform, which bridges clinical accuracy with everyday accessibility, offering targeted hormone testing without visiting a clinic.
Biochemical Overview
17-OH progesterone is synthesised from progesterone through enzymatic action and serves as a stepping stone in the cortisol and androgen pathways. Its production occurs in the adrenal cortex, ovaries, and testes, and it is transformed by enzymes like 21-hydroxylase and 11β-hydroxylase into 11-deoxycortisol, eventually becoming cortisol. The biochemical cascade is tightly regulated, and any disruption—especially enzyme deficiencies—can result in an accumulation of 17-OHP, with physiological effects that may manifest as androgen excess or cortisol deficiency. For individuals investigating fertility concerns or irregular hormone patterns, the Female Hormone Blood Test offers a detailed hormone profile that includes relevant markers, supporting differential diagnosis alongside 17-OHP levels.
Molecular Pathway
Cholesterol → Pregnenolone → Progesterone → 17-OH Progesterone → 11-Deoxycortisol → Cortisol
In enzyme deficiencies such as 21-hydroxylase deficiency, this pathway is blocked, leading to the build-up of 17-OH progesterone. Instead of being converted into cortisol, the excess is shunted toward androgen production, causing signs of virilisation, irregular menses, or ambiguous genitalia in severe cases. For patients presenting with these symptoms or adrenal-based hormonal concerns, checking associated metabolic markers can be essential. A test like the DHEA Sulphate (DHEAS) Blood Test provides additional clarity on adrenal androgen status, helping distinguish between overlapping endocrine conditions.
Clinical Importance of 17-OH Progesterone
As a vital precursor in steroid hormone biosynthesis, 17-OH progesterone has multiple key roles:
• It aids in cortisol production, a hormone essential for stress response and glucose metabolism.
• It contributes to androgen biosynthesis, influencing secondary sex characteristics.
• It plays a significant role in sexual development and reproductive function.
Among its clinical roles, 17-OH progesterone is best known for its involvement in Congenital Adrenal Hyperplasia (CAH). CAH is a set of inherited disorders resulting in improper cortisol synthesis, leading to a compensatory increase in adrenocorticotropic hormone (ACTH) and subsequent adrenal hyperplasia. Accurate diagnosis is imperative to initiate early treatment and prevent life-threatening adrenal crises. In patients with borderline 17-OHP levels, additional endocrine assessments such as the Progesterone Blood Test are helpful to interpret fluctuations across the menstrual cycle or evaluate ovulatory health in the context of broader reproductive assessments.
17-OH Progesterone Blood Test
Why the Test is Ordered
The 17-OH progesterone blood test is typically used to:
• Diagnose CAH in newborns and children
• Assess hirsutism, irregular menstruation, and infertility
• Evaluate adrenal tumours and hyperplasia
• Support hormonal evaluations in reproductive disorders
For patients seeking a more expansive diagnostic approach beyond a single hormone, the Fertility Health Tests Collection provides grouped panels designed to investigate hormonal, adrenal, and ovarian function in a single session—particularly useful in complex fertility or endocrine cases.
Normal Reference Ranges
| Group | Range (ng/dL) |
|---|---|
| Newborns (preterm) | 100–5000 |
| Newborns (full-term) | 100–2500 |
| Children | <100 |
| Adult Women (follicular) | 20–100 |
| Adult Women (luteal) | 100–500 |
| Adult Men | <200 |
Sample Collection
Timing: Early morning collection is preferred, when levels peak.
Fasting: Generally not necessary.
Cycle Timing: Women should aim for follicular phase (day 3–5) unless instructed otherwise.
Patients experiencing fatigue, adrenal dysfunction, or unexplained weight changes might benefit from a broader screening panel. The Tiredness and Fatigue Blood Test investigates common contributors such as anaemia, thyroid imbalance, and vitamin deficiencies that may coincide with hormonal imbalances.
Causes of Elevated 17-OH Progesterone
-
Congenital Adrenal Hyperplasia (CAH)
The most common cause, stemming from a 21-hydroxylase deficiency. -
Adrenal Tumours
Rarely, adrenal adenomas or carcinomas may elevate 17-OHP production independently. -
Polycystic Ovary Syndrome (PCOS)
Mild elevations are sometimes noted, though less dramatic than in CAH.
Differentiating PCOS from non-classic CAH is clinically vital. Women with persistent androgenic symptoms and elevated 17-OHP should be further evaluated with ACTH stimulation testing and additional panels. To support this, Men’s Health Tests Collection and related hormone panels can be equally valuable for male patients with androgen-related symptoms such as acne, hair loss, or reduced libido.
Causes of Low 17-OH Progesterone
Low levels of 17-OHP are less common and typically associated with:
• Adrenal insufficiency (e.g., Addison’s disease)
• Hypopituitarism
• Prolonged corticosteroid use
In such cases, checking related hormone levels and electrolytes may guide diagnosis. Adrenal support or hydrocortisone therapy might be initiated based on combined test results.
17-OH Progesterone and Female Health
Elevated 17-OHP interferes with ovulation and leads to menstrual irregularities, which can hinder fertility and overall hormonal balance. Increased androgen activity due to 17-OHP can result in acne and hirsutism. For women facing such symptoms, a targeted hormone profile like the Oestradiol Blood Test can provide vital insights into oestrogen levels, helping clarify the hormonal interplay involved.
17-OH Progesterone in Male Health
In men, abnormally high 17-OH progesterone levels may be a marker of testicular adrenal rest tumours (TARTs) or adrenal disorders. These tumours are often found in males with untreated CAH and may impair fertility. As part of a broader investigation, checking gonadal function and testosterone levels can support fertility assessments in these patients.
ACTH Stimulation Test
The ACTH stimulation test is used to confirm non-classic CAH when 17-OHP levels are borderline. It involves:
• A baseline blood sample
• Administration of synthetic ACTH
• A follow-up sample at 60 minutes
If the post-stimulation 17-OHP level exceeds 1500 ng/dL, a diagnosis of non-classic CAH is highly likely. This test remains a cornerstone of endocrinological evaluation when symptoms are suggestive but not definitive.
Treatment Options
For CAH
• Glucocorticoid therapy to replace deficient cortisol
• Mineralocorticoid supplementation for salt-wasting forms
• Regular monitoring of 17-OHP levels
• Surgery in cases of severe virilisation
For PCOS or Mild Elevations
• Oral contraceptives for hormonal regulation
• Anti-androgens to control symptoms like hirsutism
• Lifestyle modification and weight management
Patients aiming to monitor hormone changes during treatment or evaluate overall wellness can benefit from comprehensive tracking. The Health and Lifestyle Blood Test combines metabolic and hormonal markers, offering ongoing support for complex or long-term management strategies.
Future of 17-OH Progesterone Testing
Advances in LC-MS/MS technologies have dramatically improved the specificity of hormone testing. With these tools, borderline or ambiguous cases—especially in non-classic CAH—can be diagnosed with far greater reliability. These high-precision tests are becoming increasingly available for both clinical and home-based diagnostics, enabling patients to manage conditions proactively and collaboratively with their healthcare providers.
Conclusion: The Clinical Relevance of 17-OH Progesterone in Modern Endocrinology
17-hydroxyprogesterone (17-OH progesterone) occupies a critical intersection in steroid hormone biosynthesis, bridging the pathways between adrenal, reproductive, and metabolic function. Its diagnostic value extends far beyond a single-use test; it is a key biomarker in identifying congenital adrenal hyperplasia (CAH), evaluating unexplained androgen excess, and supporting fertility investigations in both men and women. Timely identification of abnormal 17-OHP levels can influence lifelong treatment decisions, especially in newborns with CAH or in adults navigating complex hormonal conditions such as PCOS or adrenal tumours. Thanks to advancements in hormone assays, including mass spectrometry and genetic screening, clinicians now have a clearer, more precise understanding of how subtle variations in hormone levels can impact health. This precision has allowed for more accurate distinctions between overlapping disorders such as non-classic CAH and PCOS—two conditions with remarkably similar outward symptoms yet vastly different therapeutic approaches.
For patients, the accessibility of reliable hormone testing is a breakthrough in personalised health. Whether prompted by reproductive concerns, skin conditions, irregular cycles, or fatigue, testing 17-OHP as part of a broader hormonal panel can help uncover underlying dysfunctions early. At-home solutions like the All Health Tests Collection offer an efficient, clinically backed alternative to traditional pathways, giving patients more autonomy over their diagnostic journey. With hormone health influencing everything from stress resilience to fertility outcomes, 17-OH progesterone serves as a powerful lens into endocrine health. Continued education, routine monitoring, and professional consultation remain essential pillars in managing hormone-related conditions effectively.
As the landscape of medicine evolves toward precision and convenience, 17-OH progesterone testing represents a convergence of clinical depth and patient-centred care—offering clarity, control, and confidence in navigating complex endocrine disorders.





























 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews