17-Hydroxyprogesterone
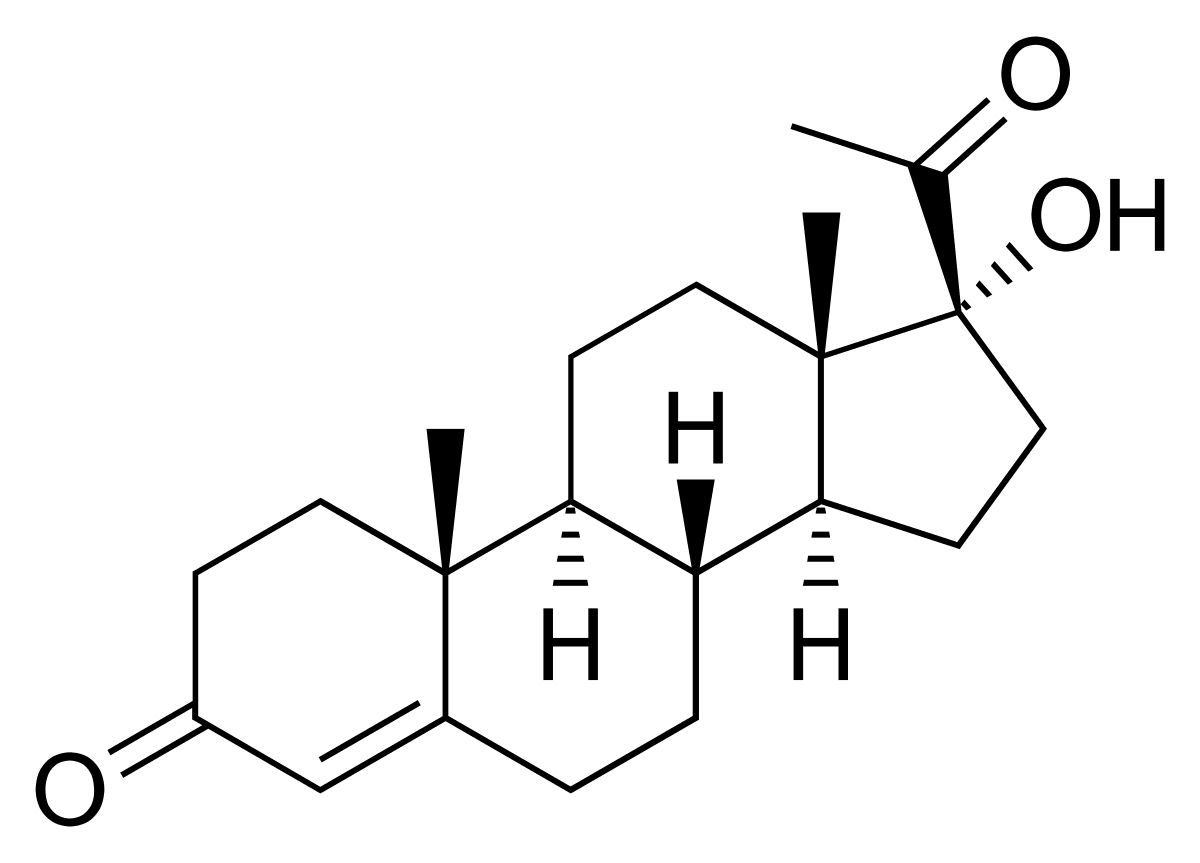
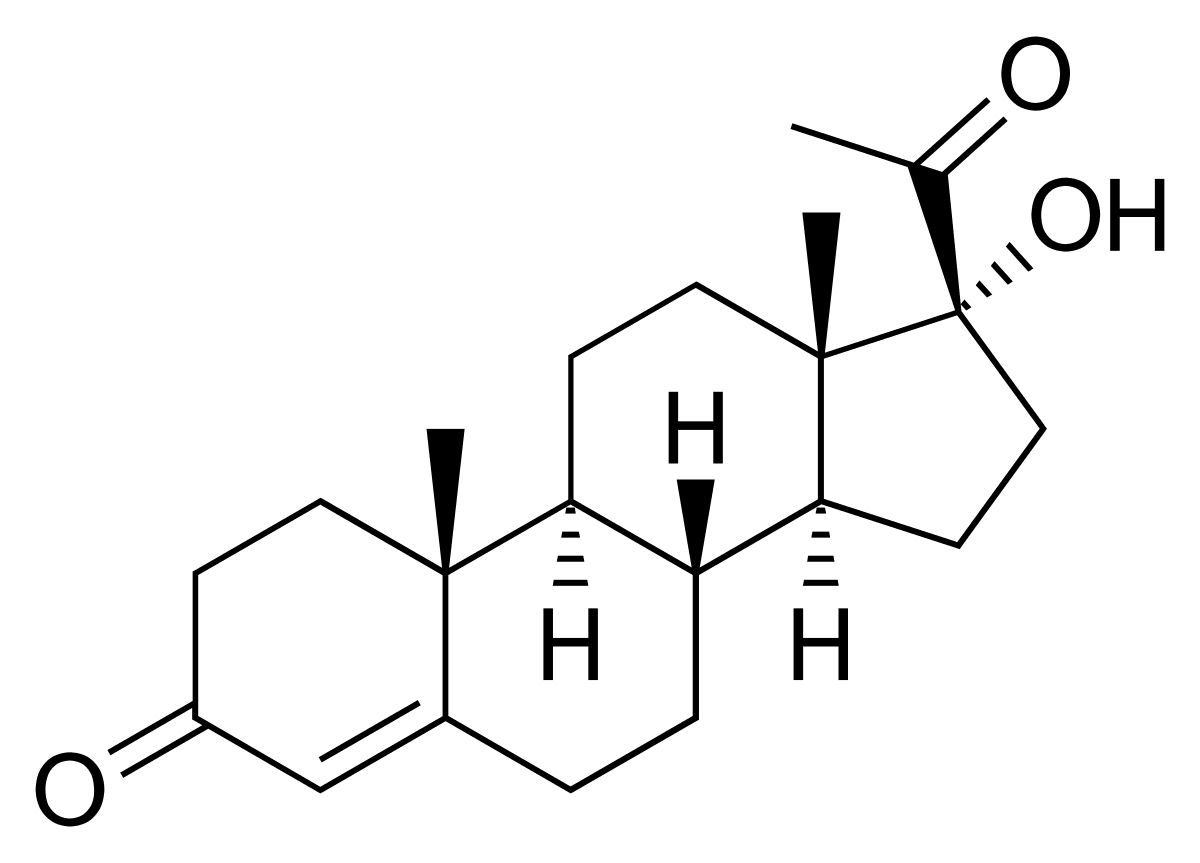
17-Hydroxyprogesterone (17-OHP) is a critical hormone involved in the intricate network of steroid biosynthesis. It plays a key intermediary role in the formation of cortisol and androgens, acting as a precursor in the metabolic pathway that governs a host of vital biological processes. Primarily produced by the adrenal glands, ovaries, and the placenta during pregnancy, 17-OHP is essential in maintaining hormonal balance and supporting healthy development during gestation. Its synthesis and regulation are tightly controlled by the hypothalamic-pituitary-adrenal (HPA) axis, a fundamental hormonal system that influences numerous aspects of growth, stress response, and metabolic regulation.
In addition to its central role during foetal development, 17-OHP continues to play an important part in adult endocrine function. Its levels fluctuate naturally due to circadian rhythms and physiological states such as puberty and pregnancy. However, abnormal concentrations—particularly elevated levels—may be indicative of underlying health disorders such as congenital adrenal hyperplasia (CAH), adrenal tumours, or ovarian cysts. Measurement of this hormone in blood or serum is a crucial diagnostic tool in paediatrics and endocrinology, particularly for screening newborns for CAH or investigating symptoms of androgen excess in adolescents and adults. One helpful tool for accessing diagnostic services is the Welzo home blood testing platform, which allows users to order tests and track hormone levels from the comfort of their own home.
This comprehensive guide explores the biosynthesis, function, clinical relevance, and diagnostic use of 17-hydroxyprogesterone. It aims to offer clear, in-depth information to help patients, clinicians, and healthcare enthusiasts better understand the hormone's role, especially in relation to adrenal and reproductive health. With mounting evidence highlighting the importance of early diagnosis and targeted therapy for conditions associated with hormonal imbalance, a deeper understanding of 17-OHP is increasingly vital in the landscape of modern medicine.
17-Hydroxyprogesterone is a naturally occurring steroid hormone produced primarily in the adrenal cortex and, to a lesser extent, by the ovaries and placenta. It is part of the glucocorticoid pathway and serves as a precursor to both cortisol and androgens like testosterone. Its synthesis originates from progesterone through the action of the 17α-hydroxylase enzyme, encoded by the CYP17A1 gene. This hormone does not have significant hormonal activity itself, but it is a vital biochemical marker for assessing adrenal function and disorders related to androgen production.
Key characteristics:
Intermediate product in steroidogenesis
Precursor to cortisol and androgens
Regulated by ACTH (adrenocorticotropic hormone)
Involved in sexual differentiation and stress response
In newborns, the screening of 17-OHP levels is particularly important for identifying congenital adrenal hyperplasia (CAH), a group of genetic disorders that affect adrenal gland function. CAH can lead to the overproduction of androgens, causing abnormal development of sexual characteristics. For individuals wanting to assess androgen levels more closely, the Free Testosterone Blood Test can offer additional insights into hormonal balance and related conditions.
Understanding 17-OHP's place within the endocrine system provides a foundation for diagnosing and managing a variety of metabolic and reproductive conditions. Through careful measurement and clinical correlation, healthcare providers can formulate targeted treatment strategies to address hormone imbalance and promote overall health.
The biosynthesis of 17-hydroxyprogesterone is a complex yet well-defined process occurring within the adrenal glands and gonads. The process begins with cholesterol, the universal precursor for all steroid hormones. Cholesterol is converted into pregnenolone, which is then metabolised into progesterone. At this point, the enzyme 17α-hydroxylase acts on progesterone to convert it into 17-hydroxyprogesterone.
Steps in the biosynthesis pathway:
Cholesterol → Pregnenolone → Progesterone → 17-Hydroxyprogesterone
Enzyme involved: CYP17A1 (17α-hydroxylase)
Location: Zona fasciculata and zona reticularis of the adrenal cortex
From this stage, 17-OHP can take one of two primary pathways:
It can be converted into 11-deoxycortisol and eventually into cortisol, a vital glucocorticoid involved in stress response and metabolism.
Alternatively, it may be converted into androstenedione and then testosterone, influencing sexual development and secondary sex characteristics.
The pathway chosen depends on the enzymatic activity within the cells and the hormonal demands of the body. In individuals with CAH, particularly 21-hydroxylase deficiency, the enzyme responsible for converting 17-OHP into 11-deoxycortisol is deficient. This results in the accumulation of 17-OHP and its diversion into androgen production, leading to symptoms of virilisation and hormonal imbalance.
If cortisol production is a concern, the Cortisol Blood Test available through Welzo offers a convenient way to monitor adrenal output and assess stress-related hormonal shifts.
Understanding the biosynthesis of 17-OHP not only explains its physiological functions but also provides critical insights into the pathophysiology of several endocrine disorders. Monitoring this hormone is an effective way to track enzymatic function in the steroidogenic pathway.
The clinical significance of 17-hydroxyprogesterone primarily lies in its utility as a biomarker for evaluating adrenal and gonadal function. It is especially critical in diagnosing congenital adrenal hyperplasia (CAH), a condition where one or more enzymes in the adrenal steroid pathway are deficient. The most common form of CAH involves 21-hydroxylase deficiency, leading to reduced cortisol production and compensatory overproduction of 17-OHP and adrenal androgens.
In newborn screening programmes, elevated 17-OHP levels are often the first indication of CAH. Early detection allows for timely medical intervention, preventing potentially life-threatening adrenal crises and inappropriate sexual development. Routine measurement is performed using dried blood spot tests on newborns within the first week of life.
Beyond CAH, elevated levels of 17-OHP may indicate:
Adrenal tumours: Excessive hormone production leading to virilisation or Cushing's syndrome
Polycystic ovary syndrome (PCOS): Mild to moderate elevation in 17-OHP due to altered adrenal or ovarian steroidogenesis
Ovarian tumours or adrenal hyperplasia: Resulting in the abnormal secretion of adrenal hormones
Stress and illness: Temporary rises due to increased ACTH stimulation
For those seeking a broad view of potential underlying conditions, the Advanced Thyroid Function Blood Test may complement adrenal assessments, especially when evaluating symptoms like fatigue or hormonal fluctuations.
In contrast, abnormally low levels may suggest adrenal insufficiency, either primary (Addison’s disease) or secondary (pituitary dysfunction). In such cases, 17-OHP measurement is used in conjunction with other hormone assays, including cortisol, ACTH, and testosterone, to arrive at a definitive diagnosis.
Treatment strategies vary based on the underlying cause and may include glucocorticoid replacement, surgical intervention in tumour cases, or hormonal therapies to balance androgen excess. The test remains a cornerstone in endocrinology for monitoring therapy and assessing disease progression or remission.
Congenital adrenal hyperplasia (CAH) is a group of inherited disorders that affect the adrenal glands, resulting in the disrupted production of steroid hormones. The most common cause of CAH is a deficiency in the enzyme 21-hydroxylase. This enzyme is crucial for the synthesis of cortisol and, to a lesser extent, aldosterone. Without adequate levels of 21-hydroxylase, the body cannot efficiently convert 17-hydroxyprogesterone into cortisol, leading to its accumulation and the subsequent overproduction of androgens.
This hormonal imbalance causes a variety of symptoms depending on the severity of the enzyme deficiency. Classic CAH, the most severe form, may present in newborns with ambiguous genitalia, salt-wasting crises, and early virilisation. Non-classic CAH, a milder form, might not appear until later in childhood or adulthood, with symptoms including acne, excessive hair growth, menstrual irregularities, or fertility issues.
17-OHP testing is essential in both diagnosing CAH and monitoring treatment. Newborn screening programmes universally include a 17-OHP blood spot test to catch cases early. Elevated levels of 17-OHP beyond a set threshold prompt further testing and clinical evaluation. Ongoing management includes daily glucocorticoid replacement to suppress excess androgen production and maintain hormonal balance.
Those interested in understanding how their overall health profile might reflect endocrine imbalances could consider browsing Welzo’s All Health Tests Collection, which features a wide range of diagnostic panels.
Timely diagnosis and proper treatment of CAH not only prevent acute adrenal crises but also improve long-term outcomes related to growth, development, and fertility. Regular monitoring of 17-OHP levels is critical to adjusting treatment plans and preventing complications associated with over- or under-treatment.
17-Hydroxyprogesterone plays a notable role in reproductive health, particularly through its influence on androgen levels and the regulation of menstrual and ovulatory cycles. In women, elevated 17-OHP can disrupt the delicate hormonal interplay required for normal follicular development and ovulation. This disruption can result in anovulatory cycles, irregular menstruation, or infertility.
In conditions like PCOS and non-classic CAH, where 17-OHP is often elevated, women may experience symptoms such as:
Oligomenorrhoea or amenorrhoea
Hirsutism (excessive hair growth)
Acne
Reduced fertility
Men experiencing related fertility issues may also benefit from testing DHEA levels. The DHEA Sulphate Blood Test evaluates adrenal androgen output and may uncover hidden causes of hormonal imbalances.
Hormone testing, including 17-OHP, is an integral part of fertility evaluations. By identifying hormone imbalances, clinicians can provide targeted interventions. Treatment options may include:
Glucocorticoid therapy to suppress adrenal androgen overproduction
Ovulation induction agents like clomiphene or letrozole
Surgical removal of adrenal or testicular masses where applicable
Understanding and managing 17-OHP levels is essential for restoring hormonal harmony and improving the likelihood of successful conception. Early detection and treatment can significantly enhance fertility outcomes in affected individuals.
During pregnancy, the placenta and adrenal glands are involved in the production of steroid hormones, including 17-hydroxyprogesterone. Maternal and foetal levels of 17-OHP rise as pregnancy progresses, playing a critical role in supporting uterine function, maintaining gestation, and ensuring appropriate development of foetal organs and endocrine structures.
Elevated 17-OHP in the mother or foetus may signal underlying issues such as CAH or placental dysfunction. In severe cases of untreated CAH, female foetuses may develop virilised genitalia due to excess androgen exposure, often detected via prenatal ultrasound or genetic testing. The condition may also increase the risk of:
Preterm labour
Low birth weight
Neonatal adrenal crises
For parents concerned about these risks, hormone-based testing such as the AMH Blood Test can provide insight into reproductive function and ovarian reserve, which may impact treatment decisions in maternal care.
Prenatal diagnosis and monitoring are essential in pregnancies at risk of CAH, particularly when both parents are carriers. If detected early, treatment with dexamethasone can reduce foetal androgen exposure and prevent virilisation in female foetuses.
Postnatal testing of 17-OHP in newborns is standard practice in many countries, enabling prompt diagnosis and treatment of CAH. With proper care, most affected children lead healthy lives.
Monitoring and understanding 17-OHP in pregnancy not only aids in identifying high-risk cases but also improves maternal-foetal outcomes and guides the provision of appropriate therapies.
17-Hydroxyprogesterone is a vital component of the body’s steroid hormone framework, acting as a precursor in the production of cortisol and androgens. Its presence and concentration are not only essential for maintaining normal endocrine function but also serve as a reliable marker for detecting several medical conditions, most notably congenital adrenal hyperplasia. The hormone’s significance spans across various stages of life, from prenatal development to puberty and beyond, influencing reproductive health, stress responses, and metabolic balance.
Those seeking a broader investigation into endocrine or autoimmune triggers may consider the Intolerance Tests Collection, particularly useful for patients with overlapping symptoms.
Through its diagnostic value, especially in newborn screening and fertility assessments, 17-OHP provides clinicians with a powerful tool to detect imbalances early and initiate effective treatment strategies. Conditions such as CAH, PCOS, adrenal tumours, and hormonal infertility can all be better managed by incorporating regular hormone profiling, including 17-OHP monitoring.
Understanding the physiological pathways and clinical contexts of 17-OHP enables both healthcare professionals and patients to make informed decisions. As advancements in endocrinology and genetics continue, the importance of 17-OHP in preventive and personalised medicine will likely increase. With comprehensive hormonal evaluation, early detection, and targeted interventions, outcomes for individuals affected by hormone-related conditions can be significantly improved.








Plus get the inside scoop on our latest content and updates in our monthly newsletter.