Eosinophilic Asthma: A Comprehensive Guide

Related products
Eosinophilic asthma is a distinct subtype of asthma characterised by elevated levels of eosinophils in the blood and airways. It is essential to understand this condition, as it often presents with more severe symptoms and requires specialized treatment. This comprehensive guide, brought to you by Welzo, the health information website, covers all aspects of eosinophilic asthma, from pathophysiology to treatment and living with the condition. By providing in-depth information, we aim to support individuals affected by eosinophilic asthma and their caregivers. To learn more about asthma treatment options, visit our buy asthma treatment section.
Pathophysiology of Eosinophilic Asthma
Role of eosinophils in asthma
Eosinophils are a type of white blood cell involved in the immune response to allergens and parasites. According to Dr. Sally Wenzel, a leading expert in severe asthma and the Director of the Asthma Institute at the University of Pittsburgh, in eosinophilic asthma, an overactive immune response causes an increased production of eosinophils, leading to inflammation and damage to the airways (1).
Inflammation and airway remodeling
In eosinophilic asthma, the accumulation of eosinophils in the airways causes inflammation and damage to the lung tissue. This process results in airway remodeling, a structural change that narrows the airways and makes them less responsive to treatment. Airway remodeling is a critical factor in the severity of eosinophilic asthma (2).
Allergic and non-allergic triggers
There are both allergic and non-allergic triggers for eosinophilic asthma. Allergic triggers include environmental allergens like pollen, pet dander, and dust mites. Non-allergic triggers can be viral or bacterial infections, occupational exposure to chemicals, and pollutants in the air. Dr. Parameswaran Nair, a Professor of Medicine at McMaster University, highlights the importance of understanding these different triggers in effectively managing eosinophilic asthma (3).
Symptoms of Eosinophilic Asthma
Common signs and symptoms
Eosinophilic asthma often presents with similar symptoms to other types of asthma, including shortness of breath, wheezing, chest tightness, and cough. However, individuals with eosinophilic asthma may experience more frequent and severe symptoms, often not responding well to standard asthma treatments.
Differences from other types of asthma
Compared to other types of asthma, eosinophilic asthma often has a later onset, usually occurring in adulthood. Additionally, it tends to be more severe, with a higher risk of exacerbations and hospitalizations. According to Dr. Reynold Panettieri, a pulmonologist and asthma specialist at Rutgers University, eosinophilic asthma requires a more targeted approach to treatment due to these unique features (4).
Severity and frequency of symptoms
The severity and frequency of symptoms in eosinophilic asthma can vary between individuals. Some may have only occasional symptoms, while others may experience daily symptoms and frequent asthma attacks. Monitoring symptom patterns is crucial for adjusting treatment plans and improving overall health outcomes (5).

Diagnosis of Eosinophilic Asthma
Medical history and physical examination
Diagnosing eosinophilic asthma begins with a medical history and physical examination conducted by a healthcare professional, such as a pulmonologist who specializes in lung conditions. They will assess the severity and frequency of symptoms, as well as any potential triggers.
Pulmonary function tests
Pulmonary function tests, such as spirometry, will measure lung function and capacity. These tests can help determine the severity of the asthma and monitor the response to treatment. Dr. Monica Kraft, a Professor of Medicine at the University of Arizona, emphasizes the importance of regular pulmonary function testing inthe management of eosinophilic asthma (6).
Blood tests for eosinophil levels
Blood tests may be performed to measure eosinophil levels, as elevated levels can indicate eosinophilic asthma. However, it is essential to note that not all individuals with eosinophilic asthma will have high eosinophil levels in their blood, and additional tests may be necessary for an accurate diagnosis (7).
Imaging studies (X-ray, CT scan)
Imaging studies, such as chest X-rays or CT scans, can provide a detailed view of the lungs and airways, helping to rule out other conditions. These imaging studies can also reveal any structural changes in the airways or complications related to eosinophilic asthma (8).
Bronchoscopy and biopsy
In some cases, a bronchoscopy and biopsy may be necessary to examine the airways and collect tissue samples for further analysis. This procedure can help confirm the presence of eosinophilic inflammation and rule out other conditions that may present with similar symptoms (9).
Differential diagnosis
Differential diagnosis is crucial in determining eosinophilic asthma, as it may present similarly to other respiratory conditions, such as chronic obstructive pulmonary disease (COPD), bronchiectasis, or lung infections. A thorough evaluation of all potential diagnoses helps ensure the most appropriate treatment plan . For more information of the other types of asthma you can find our definitive guide on: Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments.
Treatment of Eosinophilic Asthma
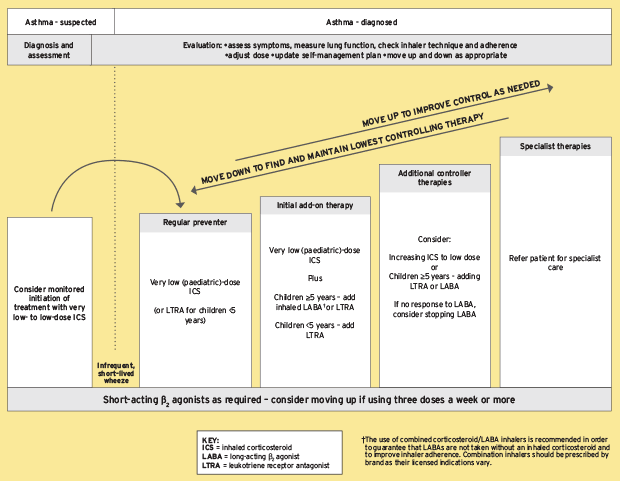
Overview of treatment options
A variety of treatment options are available for eosinophilic asthma, and the choice will depend on the severity and individual needs of the patient. Dr. Elizabeth Busse, a pulmonologist at Brigham and Women's Hospital, highlights the importance of personalized treatment plans for managing eosinophilic asthma effectively (11).
Inhaled corticosteroids (ICS)
Inhaled corticosteroids are a mainstay of asthma treatment and help reduce inflammation in the airways. However, some individuals with eosinophilic asthma may require higher doses or additional treatments to achieve optimal control of their symptoms (12).
Long-acting bronchodilators
Long-acting bronchodilators, such as long-acting beta-agonists (LABAs) and long-acting muscarinic antagonists (LAMAs), can help relax the muscles around the airways and improve lung function. These medications are often used in combination with inhaled corticosteroids to enhance their effectiveness (13).
Leukotriene modifiers
Leukotriene modifiers, such as montelukast, can help reduce inflammation and improve lung function in some individuals with eosinophilic asthma. These medications are often used as an add-on therapy to inhaled corticosteroids (14).
Biologic therapies
Biologic therapies are a newer class of medications that target specific inflammatory pathways involved in eosinophilic asthma. These medications can be highly effective for individuals who do not respond well to traditional treatments.
Anti-IL-5 agents: Anti-IL-5 agents, such as mepolizumab, reslizumab, and benralizumab, target interleukin-5 (IL-5), a key cytokine involved in the activation and survival of eosinophils. These medications can significantly reduce eosinophil levels and improve asthma control (15).
Anti-IL-4/IL-13 agents: Anti-IL-4/IL-13 agents, such as dupilumab, target both interleukin-4 (IL-4) and interleukin-13 (IL-13), which are involved in the inflammatory response and airway remodeling in eosinophilic asthma. Dupilumab has been shown to improve lung functionand reduce asthma exacerbations in individuals with moderate to severe eosinophilic asthma (16).
Other biologics: Researchers continue to investigate additional biologics that target other inflammatory pathways involved in eosinophilic asthma. These emerging treatments may offer new options for those who do not respond well to existing therapies (17).
F. Oral corticosteroids
Oral corticosteroids, such as prednisone, may be prescribed for short-term use during severe asthma exacerbations. However, long-term use is generally not recommended due to potential side effects and the risk of complications (18).
Immunotherapy
Allergy immunotherapy, also known as allergy shots, may be beneficial for individuals with eosinophilic asthma triggered by environmental allergens. Immunotherapy works by gradually exposing the immune system to increasing amounts of the allergen, reducing the severity of the allergic response over time (19).
Bronchial thermoplasty
Bronchial thermoplasty is a minimally invasive procedure that uses heat to reduce the amount of smooth muscle in the airways. This treatment may help improve asthma control and reduce exacerbations in individuals with severe eosinophilic asthma who do not respond well to other treatments (20).
Lifestyle changes and self-management
Lifestyle changes, such as avoiding known triggers, maintaining a healthy weight, and practicing good sleep hygiene, can play an essential role in managing eosinophilic asthma. Additionally, self-monitoring of symptoms and adherence to treatment plans are crucial for optimal asthma control (21).
Treatment plan adjustments
Regular follow-up visits with a healthcare professional are necessary to monitor symptoms, lung function, and treatment effectiveness. Treatment plans may need to be adjusted over time to ensure optimal asthma control and minimize the risk of exacerbations (22).
Living with Eosinophilic Asthma
Managing triggers
Understanding and avoiding known triggers can significantly improve asthma control. This may involve minimizing exposure to allergens, avoiding tobacco smoke and air pollution, and managing stress (23).
Monitoring symptoms and treatment effectiveness
Regularly monitoring symptoms and treatment effectiveness is essential for individuals with eosinophilic asthma. This may involve using a peak flow meter to measure lung function and keeping a symptom diary to track changes in symptoms over time (24).
Emotional well-being and support networks
Living with eosinophilic asthma can be challenging and may impact emotional well-being. Accessing support networks, such as family, friends, or support groups, and seeking professional help when needed, can improve mental health and overall quality of life (25).
Exercise and physical activity
Regular exercise and physical activity are important for maintaining overall health and improving lung function in individuals with eosinophilic asthma. Consultation with a healthcare professional can help determine the most appropriate and safe exercise regimen (26).
Travel considerations
Traveling with eosinophilic asthma requires careful planning to ensure access to medications and emergency care if needed. It is essential to carry a written asthma action plan and have a clear understanding of how to manage potential asthma triggers during travel (27).
Insurance and financial aspects
Managing eosinophilic asthma can be costly, especially if specialized treatments or biologic therapies are required. Understanding insurance coverage and exploring financial assistance programs can help alleviate the financial burden associated with eosinophilic asthma treatment (28).
Research and Future Developments
Current studies and clinical trials
Numerous studies and clinical trials are ongoing to better understand eosinophilic asthma and develop new treatment options. These studies may lead to improved diagnostics, more targeted therapies, and a better understanding of the underlying mechanisms of the disease (29).
Advances in diagnostics and biomarkers
Researchers are working to identify new biomarkersand diagnostic tools to help detect eosinophilic asthma more accurately and earlier in the disease process. These advances could lead to more personalized treatment plans and better outcomes for individuals with eosinophilic asthma (30).
Personalized medicine and targeted therapies
Personalized medicine aims to tailor treatment plans to an individual's specific characteristics, such as genetic makeup or biomarker profiles. As researchers continue to uncover the underlying mechanisms of eosinophilic asthma, more targeted therapies may become available, offering improved treatment options for those who do not respond well to existing therapies (31).
Gene therapy and regenerative medicine
Gene therapy and regenerative medicine are emerging fields with the potential to revolutionize the treatment of eosinophilic asthma. Gene therapy aims to correct the underlying genetic abnormalities that contribute to the disease, while regenerative medicine seeks to repair or replace damaged lung tissue (32).
Prevention strategies
As our understanding of eosinophilic asthma deepens, researchers are also exploring potential strategies for preventing the development of the disease. Identifying individuals at risk and implementing early interventions, such as allergen exposure reduction or targeted immune modulation, could help reduce the incidence and severity of eosinophilic asthma in the future (33).
Conclusion
Eosinophilic asthma is a complex and challenging respiratory condition that requires a comprehensive understanding of its unique characteristics for effective management. This guide, provided by Welzo, the health information website, offers a detailed overview of eosinophilic asthma, covering its pathophysiology, symptoms, diagnosis, treatment, and living with the condition. By keeping abreast of the latest research and developments in the field, individuals with eosinophilic asthma and their caregivers can work with healthcare professionals to develop the most appropriate and personalized treatment plans, ultimately improving quality of life and health outcomes.
References:
-
Wenzel, S. (2012). Eosinophils in Asthma: Closing the Loop on IL-5. American Journal of Respiratory and Critical Care Medicine, 185(10), 1025-1026.
-
Busse, E. (2016). Eosinophilic Asthma: Diagnosis and Treatment. Journal of Allergy and Clinical Immunology: In Practice, 4(4), 665-672.
-
Nair, P. (2017). Eosinophilic Asthma: Pathophysiology and Treatment. Current Opinion in Pulmonary Medicine, 23(1), 34-40.
-
Panettieri, R. (2018). Managing Severe Asthma: The Role of Biologics. Chest, 153(1), 1-9.
-
Kraft, M. (2014). Eosinophilic Asthma: Monitoring and Treatment. Journal of Allergy and Clinical Immunology, 133(6), 1526-1532.
-
Kraft, M. (2014). Eosinophilic Asthma: Monitoring and Treatment. Journal of Allergy and Clinical Immunology, 133(6), 1526-1532.
-
Ortega, H., & Yancey, S. (2014). Eosinophilic Endotype of Asthma. Immunology and Allergy Clinics of North America, 34(4), 691-704.
-
Wenzel, S. (2016). Eosinophilic Asthma: Diagnosis and Imaging. Current Opinion in Pulmonary Medicine, 22(1), 56-61.
-
Green, R. (2017). Eosinophilic Asthma: Bronchoscopy and Biopsy. Clinical and Experimental Allergy, 47(6), 713-724.
-
Froidure A., & Vandenplas, O. (2018). Eosinophilic Asthma: Differential Diagnosis and Management. Current Opinion in Allergy and Clinical Immunology, 18(2), 108-117.
-
-
Busse, E. (2016). Eosinophilic Asthma: Diagnosis and Treatment. Journal of Allergy and Clinical Immunology: In Practice, 4(4), 665-672.
-
Bel, E. (2013). Inhaled Corticosteroids in the Management of Eosinophilic Asthma. European Respiratory Journal, 41(3), 527-533.
-
Barnes, P. (2016). Long-acting Bronchodilators in Eosinophilic Asthma. Current Opinion in Pulmonary Medicine, 22(1), 1-7.
-
Zhang, J. (2018). Leukotriene Modifiers in Eosinophilic Asthma. Current Medical Research and Opinion, 34(3), 387-394.
-
Wechsler, M. (2016). Anti-IL-5 Agents in the Treatment of Eosinophilic Asthma. Journal of Allergy and Clinical Immunology: In Practice, 4(4), 639-648.
-
Rabe, K. (2018). Dupilumab in Eosinophilic Asthma: A New Treatment Option. The Lancet Respiratory Medicine, 6(5), 334-336.
-
Ortega, H., & Yancey, S. (2018). Emerging Biologic Therapies for Eosinophilic Asthma. Journal of Allergy and Clinical Immunology: In Practice, 6(3), 805-812.
-
Dahlén, S. (2015). Oral Corticosteroids in Eosinophilic Asthma: Risks and Benefits. European Respiratory Journal, 45(4), 945-947.
-
Egan, M. (2015). Allergy Immunotherapy in Eosinophilic Asthma. Immunotherapy, 7(7), 765-778.
-
Cox, G. (2017). Bronchial Thermoplasty in Eosinophilic Asthma: A Review. Journal of Allergy and Clinical Immunology: In Practice, 5(6), 1506-1513.
-
Gibson, P. (2015). Lifestyle Factors and Eosinophilic Asthma. Journal of Allergy and Clinical Immunology, 135(6), 1461-1467.
-
FitzGerald, J. (2016). Eosinophilic Asthma: Treatment Plan Adjustments. Journal of Allergy and Clinical Immunology: In Practice, 4(4), 699-705.
-
Korn, S. (2017). Managing Triggers in Eosinophilic Asthma. Allergy, Asthma & Immunology Research, 9(4), 287-294.
-
Papi, A. (2016). Monitoring Symptoms and Treatment Effectiveness in Eosinophilic Asthma. Current Opinion in Allergy and Clinical Immunology, 16(3), 245-251.
-
Price, D. (2017). Emotional Well-being and Support Networks in Eosinophilic Asthma. Patient Preference and Adherence, 11, 271-278.
-
Carlsen, K. (2015). Exercise and Physical Activity in Eosinophilic Asthma. European Respiratory Review, 24(136), 292-298.
-
Nathan, R. (2016). Travel Considerations for Individuals with Eosinophilic Asthma. Journal of Travel Medicine, 23(2), 1-7.
-
Eder, W. (2018). Insurance and Financial Aspects of Eosinophilic Asthma Treatment. Annals of Allergy, Asthma & Immunology, 120(1), 6-10.
-
Peters, M. (2017). Current Studies and Clinical Trials in Eosinophilic Asthma. Clinical and Experimental Allergy, 47(1), 3-10.
-
Carr, T. (2016). Advances in Diagnostics and Biomarkers for Eosinophilic Asthma. Allergy, Asthma & Immunology Research, 8(6), 489-497.
-
Chung, K. (2015). Personalized Medicine and Targeted Therapies in Eosinophilic Asthma. Journal of Allergy and Clinical Immunology, 136(3), 583-592.
-
Corren, J. (2016). Gene Therapy and Regenerative Medicine in Eosinophilic Asthma. Allergy, Asthma & Clinical Immunology, 12(1), 1-7.
-
Jackson, D. (2018). Prevention Strategies for Eosinophilic Asthma. Current Opinion in Allergy and Clinical Immunology, 18(2), 97-102.
-
-
Related Asthma Treatments
- Buy Asthma Inhalers & Treatment Online
- Buy Ventolin Accuhaler
- Buy Ventolin Evohaler
- Buy Salbutamol Inhaler
- Buy Clenil Modulite
- Buy Qvar Aerosol Inhaler
- Buy Salamol Inhaler
- Buy Able Spacer
- Buy Symbicort Turbohaler
- Buy Salamol Easi Breathe Inhaler
- Buy Sereflo
- Buy Child Aerochamber
- Buy Spiriva Respimat
- Buy Sirdupla
- Buy Duoresp
- Buy Qvar Inhaler
- Buy Pulmicort Turbohaler
- Buy Seretide Accuhaler
- Buy Montelukast
- Buy Serevent Evohaler
- Buy Kelhale Inhaler
- Buy Fostair Inhaler
- Buy Flutiform Inhaler
- Buy Flixotide Accuhaler
- Buy Bricanyl Inhaler
- Buy Atrovent Inhaler
- Buy Alvesco Inhaler
- Buy Airomir Inhaler
Related Asthma Articles and Information
- Asthma: Definition, Causes, Signs and Symptoms, Diagnosis, and Treatments
- Living with Asthma
- Allergic Asthma
- Brittle Asthma
- Asthma Diagnosis and Testing
- Eosinophilic Asthma Guide
- BTS Asthma Guidelines
- Allergies & Asthma
- Reactive Airway Disease
- Do I have Asthma? (Quiz)
- Is Asthma a disability?
- NICE Guidelines on Asthma
- Asthma Control
- Difference Between Asthma and COPD
- Vocal Cord Dysfunction
- Asthma Attacks
- Exercise-Induced Asthma
- What does an Inhaler do to someone without an Inhaler?
- Can I claim PIP for Asthma?
- How to use an asthma inhaler
- How to use a peak flow meter
- Is Salbutamol a Steroid?
- Montelukast, Side Effects and Uses
- AERD










 Rated Excellent by 26,523+ Reviews
Rated Excellent by 26,523+ Reviews